Every two minutes, someone in North America is diagnosed with melanoma — the deadliest form of skin cancer. Yet when caught early, the five-year survival rate exceeds 99%. The difference between life and death often comes down to one simple habit: knowing what to look for on your own skin. A thorough suspicious mole checklist is the single most accessible tool available to help identify warning signs before they become a serious health threat.
Most adults have between 10 and 40 moles on their body, and the vast majority are completely harmless [2]. But among those common spots, a single dangerous mole can hide in plain sight. The challenge is knowing which moles deserve attention and which ones are simply part of normal skin. This guide breaks down every element of a comprehensive suspicious mole checklist — from the well-known ABCDE rule to the lesser-known "ugly duckling" sign — so that anyone can perform a confident self-examination at home.
Whether a mole has recently changed shape, developed an unusual color, or simply "feels different," this article provides the knowledge needed to take informed action. Early detection saves lives, and it starts with awareness.
A suspicious mole checklist is a structured set of criteria used to evaluate whether a mole (also called a nevus) shows features associated with skin cancer — particularly melanoma. Think of it as a screening tool that empowers everyday people to monitor their own skin between professional dermatology appointments.
Melanoma accounts for only about 1% of all skin cancers, but it is responsible for the vast majority of skin cancer deaths [7]. The reason? Melanoma can spread (metastasize) to other organs quickly if not detected and removed in its earliest stages. A suspicious mole checklist helps bridge the gap between annual doctor visits by giving individuals a reliable way to spot trouble early.
The short answer: everyone. Skin cancer does not discriminate. While certain populations face higher statistical risk — including people with fair skin, a history of sunburns, or a family history of melanoma — skin cancer can develop in people of all skin tones and backgrounds [1][4].
That said, the following groups should be especially vigilant:
Risk FactorWhy It Matters50+ moles on the bodyHigher statistical melanoma risk [2]Fair skin, light eyes, red/blond hairLess natural melanin protectionHistory of blistering sunburnsUV damage accumulates over timeFamily history of melanomaGenetic predispositionWeakened immune systemReduced ability to fight abnormal cellsPrevious skin cancer diagnosisElevated recurrence riskAtypical (dysplastic) molesMoles already showing unusual features
Understanding the different types of moles — including atypical moles — is an important first step in knowing what to watch for.
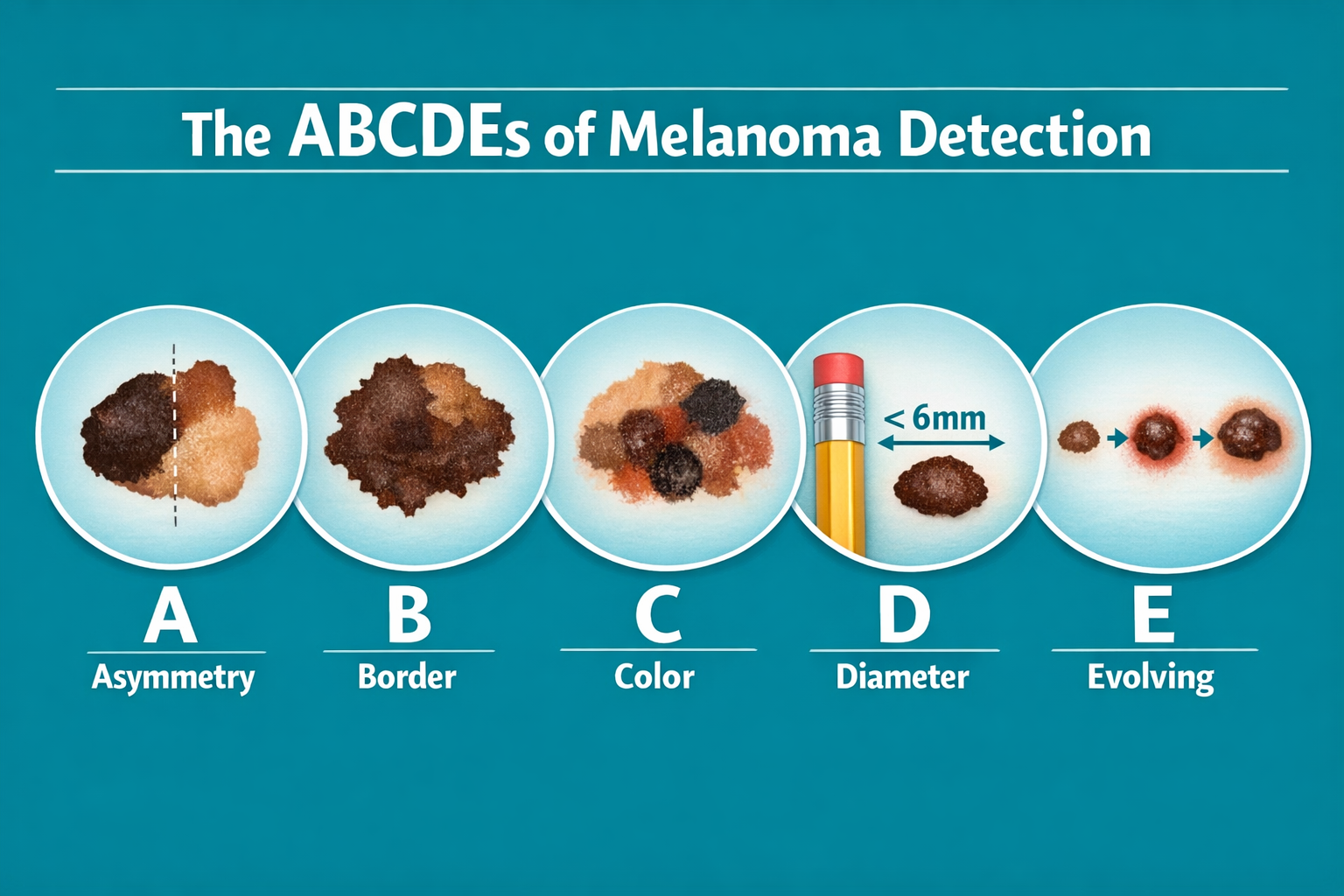
The ABCDE rule is the most widely recognized and clinically validated framework for evaluating moles. Developed by dermatologists, it provides five clear criteria that anyone can learn and apply during a self-examination [5][7]. Each letter represents a specific feature to assess.
What to check: Draw an imaginary line through the center of the mole. Do both halves match?
A benign (harmless) mole is typically symmetrical — meaning one half mirrors the other. A suspicious mole, on the other hand, will have two halves that look noticeably different in shape, size, or structure [3][7].
💡 Quick Test: If the mole were folded in half, would the two sides line up? If not, that asymmetry is a red flag.
What to check: Are the edges of the mole smooth and well-defined, or are they ragged, notched, blurred, or scalloped?
Normal moles typically have clean, even borders. Melanomas often display borders that are:
What to check: Is the mole one uniform color, or does it contain multiple shades?
Most benign moles are a single shade of brown. A mole that contains multiple colors — such as different shades of brown, black, tan, red, white, or blue — is considered suspicious [3][6]. The presence of blue-black coloring is particularly concerning, though it is worth noting that some benign moles, such as a blue nevus, can naturally appear blue without being dangerous.
What to check: Is the mole larger than 6 millimeters (about the size of a pencil eraser)?
While melanomas can technically be any size, moles larger than 6–7 mm in diameter are flagged for closer inspection [5][7]. That said, this criterion alone is not definitive — some melanomas are detected at smaller sizes, and some large moles are perfectly benign.
Size ReferenceApproximate DiameterPencil tip1–2 mmPencil eraser6 mm ⚠️Dime18 mmQuarter24 mm
What to check: Has the mole changed in any way — size, shape, color, elevation, or texture — over weeks or months?
Many dermatologists consider "E" the most critical letter in the ABCDE rule. A mole that is evolving — growing, changing color, becoming raised, or developing new symptoms — demands prompt medical evaluation, even if it does not meet the other ABCDE criteria [3][7].
Evolution can include:
Understanding the difference between flat moles and raised moles and their respective cancer risks can provide additional context when evaluating this criterion.
"A mole that changes is a mole that needs checking. When in doubt, get it looked at." — Common dermatology guidance
While the ABCDE rule is excellent for home use, clinicians often rely on an expanded 7-point checklist that provides additional diagnostic depth [1]. This tool is particularly useful in clinical settings where a more nuanced evaluation is needed.
ScoreRecommended Action0–2Low suspicion — continue monitoring monthly3+Higher suspicion — seek professional evaluation promptly
A score of 3 or more on the 7-point checklist is generally considered the threshold for referral to a dermatologist or skin cancer specialist [1]. Even a single major feature (scoring 2 points) combined with one minor feature warrants professional assessment.
For those who want expert evaluation, finding the best melanoma specialist nearby can make a significant difference in outcomes.
One of the most intuitive and effective methods for spotting a potentially dangerous mole is the "ugly duckling" sign [2][6]. This concept is simple but powerful.
Most benign moles on a single individual tend to look similar to each other. They share a general family resemblance in terms of size, color, shape, and pattern. The "ugly duckling" is the mole that stands out — the one that looks noticeably different from all the others.
🦆 Think of it this way: If all the moles on the body are like a flock of similar-looking ducks, the "ugly duckling" is the one that clearly does not belong.
The ugly duckling sign is especially useful for people who have many moles (50 or more), where applying the ABCDE rule to every single mole can feel overwhelming [2]. Instead of analyzing each mole individually, the ugly duckling approach encourages a broader comparison.
It is also worth understanding that certain conditions can cause the appearance of many new moles, which may require medical attention in their own right.
Dermatologists recommend performing a full-body skin self-examination once per month [3][4][6]. Consistency is key — the goal is to become so familiar with one's own skin that any change, no matter how subtle, is noticed quickly.
Step 1: Face and Scalp 🧑 Examine the face closely, including the nose, lips, ears (front and back), and around the eyes. Use a comb or hair dryer to part the hair and inspect the scalp section by section. The scalp is a commonly overlooked high-risk location [1][4].
Step 2: Hands and Arms 🤲 Check the palms, backs of the hands, between the fingers, and under the fingernails. Extend the examination up the forearms and upper arms, including the underarms.
Step 3: Torso (Front and Back) 👕 Stand in front of the full-length mirror and examine the chest, abdomen, and sides. Then use the handheld mirror to inspect the entire back, shoulders, and the back of the neck.
Step 4: Lower Body 🦵 Examine the buttocks, the backs of the legs, and the fronts of the legs. Sit down and check the tops and soles of the feet, between the toes, and under the toenails.
Step 5: Intimate Areas 🩺 Do not skip the genital area, groin folds, or inner thighs. Melanoma can develop in areas that receive little or no sun exposure [4]. For concerns in these sensitive areas, consulting a professional about genital mole removal is advisable.
Taking photos of moles over time is one of the most effective ways to track changes. Here are best practices:
Professional mole mapping services use dermoscopy and digital photography to create a detailed baseline of all moles on the body. For those interested, exploring mole mapping clinics in Toronto can provide access to advanced screening technology.
While visual features (ABCDE and the ugly duckling sign) form the core of any suspicious mole checklist, there are additional symptoms and sensations that should not be ignored [7][9].
SymptomWhat It May IndicateItchingPossible inflammatory changes within the moleTenderness or painUnusual nerve involvement or growthBleeding without injuryPossible ulceration of a melanomaOozing or crustingBreakdown of skin surface integrityNon-healing soreA lesion that heals and reopens repeatedly may be cancerousRedness or swelling beyond the mole borderInflammation suggesting abnormal activitySatellite lesionsNew small spots appearing near an existing mole
Standard ABCDE criteria can sometimes miss nodular melanoma, a particularly aggressive subtype that may appear as a raised, dome-shaped bump rather than a flat, spreading lesion. For this type, dermatologists have developed the supplementary EFG rule:
A firm, growing nodule — even if it is skin-colored or reddish rather than dark — should be evaluated urgently [9].
Learning to recognize the signs of early-stage basal cell carcinoma is also valuable, as this common skin cancer can sometimes be confused with a changing mole.
Not all body locations carry equal risk. Certain areas are more prone to developing melanoma or are more easily overlooked during self-examinations [1][4].
While UV exposure is a major risk factor, melanoma can also develop in areas that rarely see sunlight — such as the palms, soles, and genital region [4]. This is why a complete head-to-toe examination is essential, not just a check of sun-exposed skin.
For individuals with darker skin tones, moles in specific locations may have unique characteristics. Understanding conditions like DPN (Dermatosis Papulosa Nigra) — common dark bumps in skin of color — can help distinguish benign growths from truly suspicious lesions.
Below is a consolidated checklist that combines the ABCDE rule, the 7-point checklist, the ugly duckling sign, and additional warning symptoms into one comprehensive tool. Consider printing this out and keeping it near the bathroom mirror for monthly self-examinations.
ABCDE Criteria:
Ugly Duckling Assessment:
Physical Symptoms:
EFG Criteria (Nodular Melanoma):
High-Risk Location Check:
⚠️ Action Threshold: If any single item on this checklist is checked, schedule a professional skin evaluation. If multiple items are checked, seek evaluation as soon as possible.
Identifying a suspicious mole is only the first step. Knowing what to do next is equally important.
The vast majority of moles that meet one or two ABCDE criteria turn out to be benign (non-cancerous). Having a suspicious-looking mole does not automatically mean cancer. It means the mole deserves professional evaluation [2][3].
Before the appointment, take clear, well-lit photographs of the mole from multiple angles. Note:
A dermatologist or trained clinician can perform a dermoscopic examination — using a specialized magnifying instrument to view the mole's internal structures that are invisible to the naked eye [8]. This non-invasive assessment can often determine whether a biopsy is needed.
For those who prefer not to wait for a referral, walk-in dermatology clinics can provide timely access to professional evaluation.
If the clinician determines that a mole warrants further investigation, a biopsy will be performed. This involves removing all or part of the mole and sending the tissue to a pathology laboratory for microscopic analysis [8].
The pathology report will confirm whether the mole is:
Understanding the results can feel overwhelming. A detailed guide to demystifying pathology reports after mole removal can help make sense of the medical terminology.
If a mole is found to be cancerous, treatment typically involves surgical excision with clear margins. Early-stage melanoma that has not spread is usually curable with surgery alone. More advanced cases may require additional treatments such as immunotherapy or radiation [7].
Even after successful treatment, ongoing surveillance with regular skin checks is essential to monitor for recurrence or new suspicious moles.

Misinformation about moles and skin cancer is widespread. Here are some of the most common myths, along with the facts.
Fact: While many melanomas are dark brown or black, some are pink, red, skin-colored, or even colorless [3][7]. Amelanotic melanomas (those lacking pigment) are among the most dangerous because they are easily overlooked. Even flesh-colored moles deserve attention if they are changing.
Fact: Most early melanomas are completely painless. Pain, itching, or tenderness may develop as the melanoma progresses, but the absence of pain is not a reliable indicator of safety [7].
Fact: Melanoma is one of the most common cancers in young adults aged 25–29. No age group is immune [6].
Fact: There is no scientific evidence that properly removing a mole causes cancer to spread. In fact, removal and biopsy are the standard of care for diagnosing and treating suspicious moles [8].
Fact: While melanoma is less common in individuals with darker skin, it tends to be diagnosed at later, more advanced stages — making it more dangerous. Special attention should be paid to the palms, soles, and nail beds [1][4].
Fact: Over-the-counter mole removal products can cause scarring, infection, and — most dangerously — can destroy the surface of a mole while leaving potentially cancerous cells beneath the skin undetected. Professional evaluation is always recommended for suspicious moles [8].
Not every mole change requires an emergency visit, but certain scenarios demand urgent attention. Here is a general timeline guide:
While detection is the primary purpose of a suspicious mole checklist, prevention plays an equally important role in reducing skin cancer risk.
Understanding the complete UV index guide can help individuals make informed decisions about daily sun exposure.
The suspicious mole checklist applies universally, but certain populations may need to adjust their approach.
People with a high mole count face statistically higher melanoma risk [2]. For these individuals:
Melanoma in darker-skinned individuals most commonly occurs on the palms, soles, nail beds, and mucous membranes [1][4]. The ABCDE rule still applies, but extra attention should be paid to:
Moles in children are common and usually benign. However, any mole that is rapidly growing, unusually large, or symptomatic should be evaluated. Congenital moles (present at birth) that are very large may carry increased risk and should be monitored by a pediatric dermatologist.
Anyone who has had a previous skin cancer diagnosis should undergo more frequent professional skin examinations (typically every 3–6 months) and perform monthly self-checks with heightened vigilance [8].
Advances in technology have made mole monitoring more accessible than ever. However, these tools should supplement — not replace — professional evaluation.
Several smartphone apps allow users to photograph moles and track changes over time using AI-powered analysis. While these can be helpful for documentation, studies show that 3D mole mapping apps vary significantly in reliability and should not be used as a substitute for clinical assessment.
Dermoscopy uses a specialized magnifying device with polarized light to examine the subsurface structures of a mole. This technique can reveal patterns invisible to the naked eye and significantly improves diagnostic accuracy [8].
Some dermatology clinics offer total body photography — a comprehensive photographic record of the entire skin surface that serves as a baseline for future comparisons. This is particularly valuable for high-risk individuals.
Perform a full-body self-examination once per month [3][6]. Mark a recurring date on the calendar to build consistency.
Absolutely. Many moles that meet one or more ABCDE criteria are ultimately benign. Atypical (dysplastic) moles, for example, may look unusual but are not cancerous [2]. Only a biopsy can provide a definitive diagnosis.
Not necessarily. A dermatologist will assess the mole and determine whether removal and biopsy are warranted. Some moles may simply need closer monitoring [8].
A healthy mole is typically symmetrical, evenly colored, smooth-bordered, smaller than 6 mm, and stable over time. A cancerous mole may display one or more ABCDE features. For a visual comparison, exploring healthy vs. early cancerous moles can be very helpful.
No. Home removal methods (creams, pens, cutting) are dangerous because they can cause infection, scarring, and — most critically — can mask or delay the diagnosis of skin cancer [8]. Always seek professional removal.
In some cases, a mole may partially recur after removal. This is usually benign but should be evaluated to rule out incomplete removal of abnormal cells. Learn more about whether moles grow back after removal.
Skin cancer is one of the most preventable and treatable cancers — when caught early. The suspicious mole checklist outlined in this guide provides a practical, evidence-based framework that anyone can use to monitor their skin and identify potential warning signs.
Here are the actionable next steps to take right now:
Early detection is not just a medical recommendation — it is a life-saving habit. The few minutes spent each month examining the skin could make all the difference. Start today.
[1] The ABCDE Skin Cancer Guide for Quick Melanoma Detection - https://bhskin.com/blog/the-abcde-skin-cancer-guide-for-quick-melanoma-detection/
[2] A Guide to Moles and Suspicious Spots - https://optimadermatology.com/2025/05/07/a-guide-to-moles-and-suspicious-spots
[3] Skin Moles: A Guide on What to Look For - https://www.reformedermatology.com/skin-moles-a-guide-on-what-to-look-for/
[4] Skin Check Leaflet - https://melanomafocus.org/about-melanoma/skin-check-leaflet/
[5] How to Monitor Your Moles - https://www.mdveins.com/blog/how-to-monitor-your-moles
[6] Melanoma Detection ABCDE Guide - https://www.psdermgroup.com/melanoma-detection-abcde-guide
[7] The ABCDEs of Moles - https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/the-abcdes-of-moles
[8] Skin Self-Exam - https://my.clevelandclinic.org/health/diagnostics/8648-skin-self-exam
[9] Taking Action with Concerns - https://www.skcin.org/skin-cancer-types/taking-action-with-concerns/