When the doctor hands you that pathology report after your mole removal, it might as well be written in ancient hieroglyphics. 📋 Those medical terms, numbers, and classifications can transform what should be relief into anxiety. Understanding your pathology report is crucial for making informed decisions about your health and determining if any follow-up care is needed.
Every year, millions of people undergo mole removal procedures, yet most receive their pathology reports without proper explanation of what the findings actually mean. This comprehensive guide will demystify your pathology report after mole removal, translating complex medical terminology into clear, understandable language that empowers you to take control of your skin health journey.
• Pathology reports contain vital information about your removed mole, including cell type, margins, and any signs of abnormal growth
• Most mole removals result in benign findings, but understanding the terminology helps you interpret results accurately
• Margins, dysplasia, and mitotic rate are key terms that indicate whether additional treatment may be necessary
• Clear communication with your healthcare provider is essential for understanding your specific results and next steps
• Regular skin monitoring remains important regardless of your pathology report findings
A pathology report serves as your mole's medical biography, documenting everything a pathologist discovers when examining your tissue sample under a microscope. Think of pathologists as medical detectives who analyze cellular evidence to determine exactly what type of growth was removed and whether it poses any health concerns.
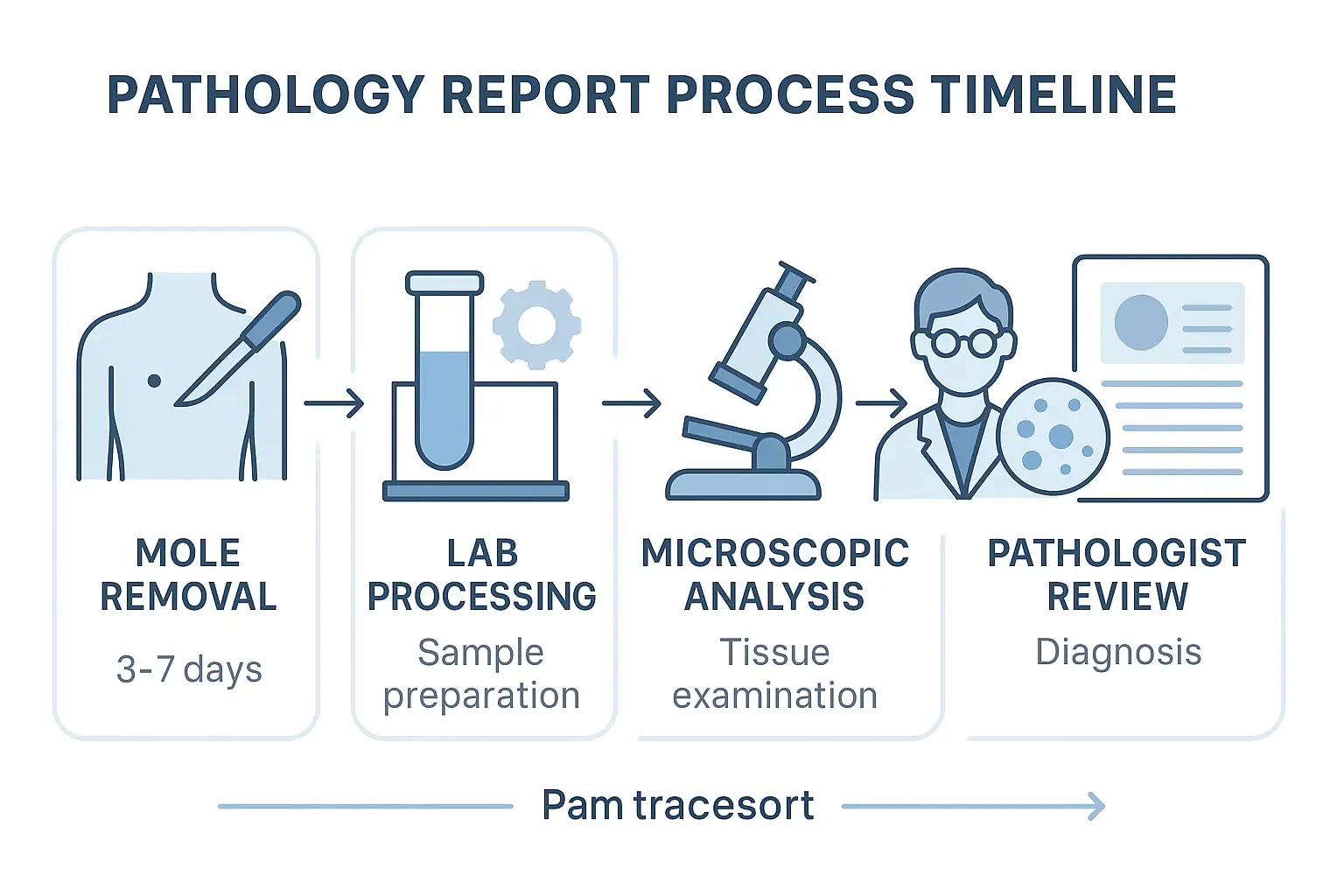
Once your healthcare provider removes a mole, the tissue sample embarks on a detailed journey through the laboratory. The specimen gets preserved in formalin, a chemical solution that maintains the tissue's structure. Laboratory technicians then process the sample, creating ultra-thin slices that can be examined under powerful microscopes.
Pathologists examine multiple aspects of your mole sample:
This thorough analysis typically takes 3-7 business days, though complex cases may require additional time for specialized testing or consultation with other pathologists.
Benign (Non-cancerous) Results represent the vast majority of mole removal outcomes. These findings indicate normal skin growths that pose no immediate health threat. Common benign diagnoses include:
Atypical or Dysplastic Results fall into a gray area between normal and abnormal. These findings suggest some unusual cellular features that require monitoring but aren't necessarily cancerous. Dysplastic nevi show irregular growth patterns that may increase future skin cancer risk.
Malignant (Cancerous) Results require immediate attention and treatment planning. While less common, these findings include various types of skin cancer that need prompt medical intervention.
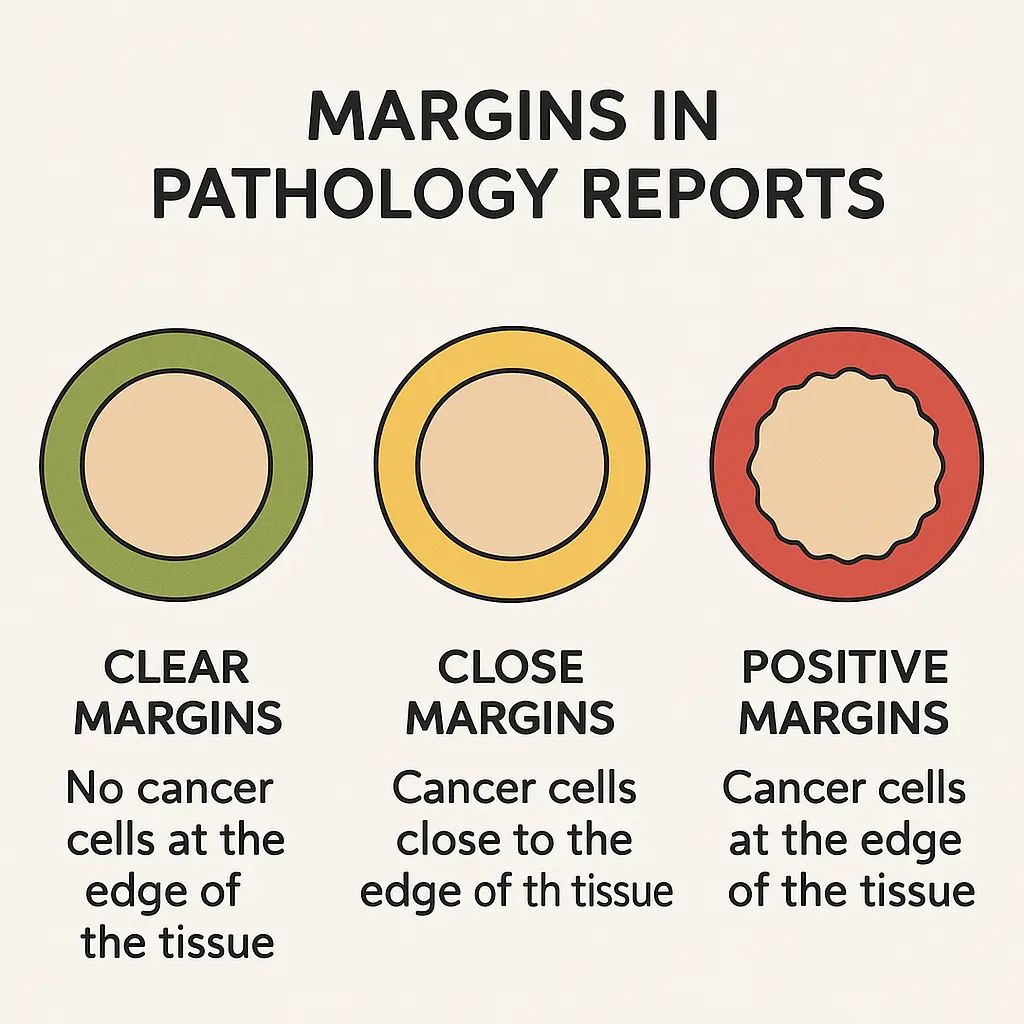
Margins represent one of the most critical elements in your pathology report. This term describes the edge of tissue surrounding your removed mole and indicates whether the entire growth was successfully eliminated.
Clear margins (also called "negative margins") mean the pathologist found normal, healthy tissue at all edges of the removed sample. This finding suggests complete removal of the mole and typically requires no additional treatment.
Positive margins indicate that abnormal cells extend to the edge of the removed tissue. This finding suggests that some of the mole may remain in your skin, potentially requiring additional removal or closer monitoring.
Close margins describe situations where abnormal cells come very near the tissue edge without actually reaching it. Your healthcare provider may recommend additional removal or enhanced monitoring depending on the specific circumstances.
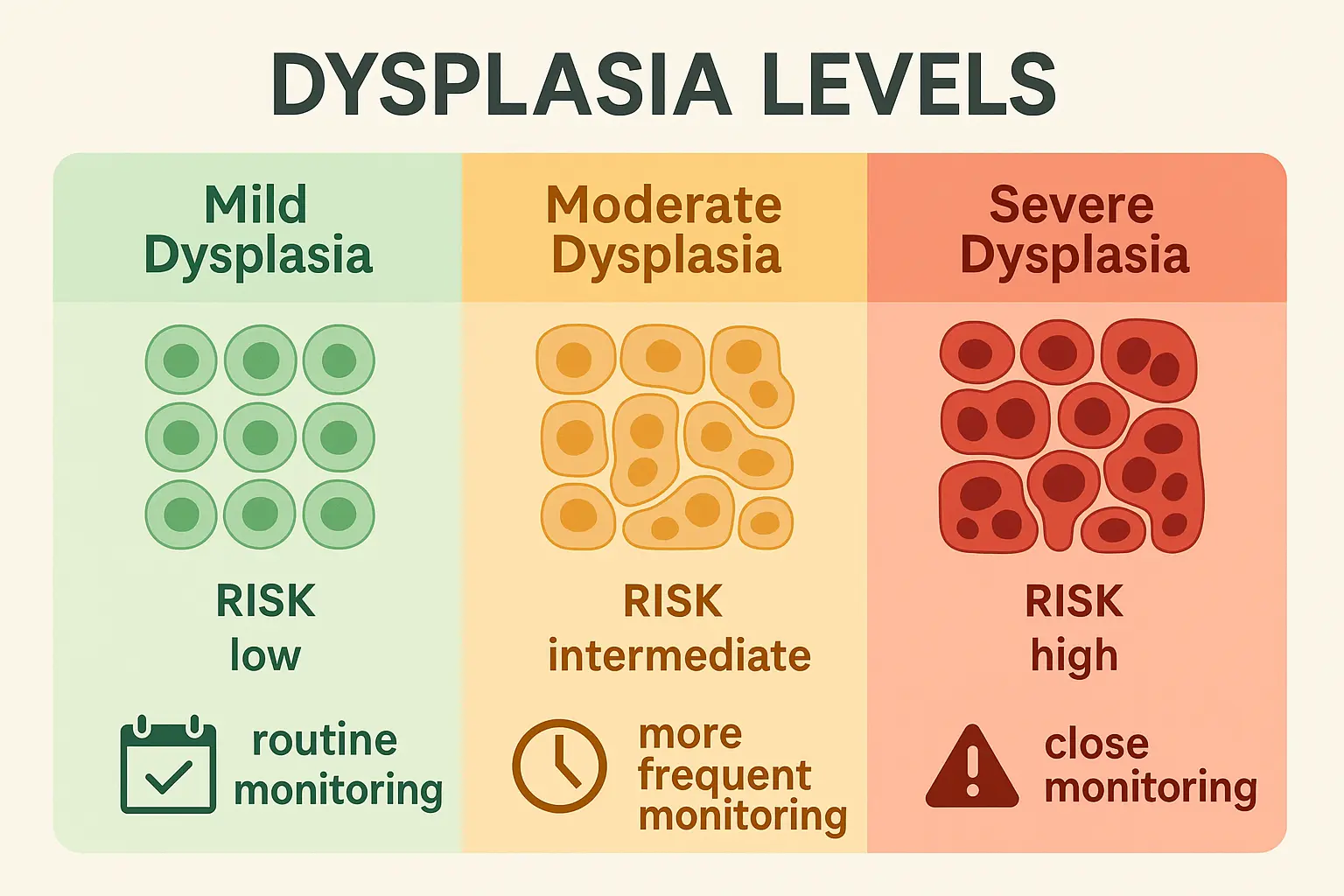
Dysplasia refers to abnormal cellular development that appears somewhere between normal and cancerous. When pathologists identify dysplasia in your mole, they're observing cells that don't follow typical growth patterns but haven't yet become malignant.
Mild dysplasia shows slight irregularities in cell size, shape, or organization. These changes often require routine monitoring but rarely need immediate intervention.
Moderate dysplasia displays more pronounced cellular abnormalities. Your healthcare provider may recommend more frequent skin examinations or additional preventive measures.
Severe dysplasia exhibits significant cellular irregularities that approach, but don't quite reach, cancerous changes. This finding typically warrants close monitoring and may require additional tissue removal.
Mitotic rate measures how rapidly cells within your mole were dividing when the tissue was removed. Cell division is a normal process, but excessive division rates can indicate aggressive growth patterns.
Low mitotic rates suggest slow, controlled cell division typical of benign growths. Most normal moles exhibit minimal mitotic activity.
Elevated mitotic rates may indicate more aggressive cellular behavior. Pathologists count the number of dividing cells in specific tissue areas to calculate this measurement.
The significance of mitotic rate varies depending on other pathology findings. High mitotic rates combined with other abnormal features may suggest malignant potential, while isolated elevation might simply indicate active but benign growth.
This section provides basic information about your removed tissue, including size, color, and general appearance. Pathologists document these details before beginning microscopic examination.
Size measurements appear in centimeters or millimeters, describing the specimen's length, width, and depth. These measurements help determine whether the removal was adequate and provide baseline information for future comparisons.
Gross appearance describes how your mole looked to the naked eye before processing. Terms like "pigmented," "raised," or "irregular" help characterize the growth's basic features.
The microscopic examination section contains the most detailed analysis of your mole's cellular characteristics. Pathologists describe cell types, organization patterns, and any unusual features observed under magnification.
Cell morphology refers to the size, shape, and appearance of individual cells within your mole. Normal cells typically display uniform characteristics, while abnormal cells may show irregular features.
Architectural patterns describe how cells organize themselves within the tissue. Benign moles usually show orderly arrangements, while problematic growths may display chaotic organization.
Inflammatory changes indicate your body's immune response to the mole. Some inflammation is normal, but excessive inflammatory activity might suggest irritation or other concerns.
The diagnosis section provides the pathologist's conclusion about your mole's nature. This represents the most important part of your report, summarizing all findings into a clear medical classification.
Primary diagnosis identifies the main type of growth that was removed. This might be a specific type of benign mole, an atypical growth, or a malignant lesion.
Additional findings may include secondary observations like inflammation, infection, or other tissue changes noted during examination.
Intradermal nevi represent the most common type of mole, consisting of nevus cells located entirely within the deeper skin layers. These typically appear as dome-shaped, flesh-colored growths and rarely cause concern.
Compound nevi contain nevus cells in both the surface (epidermis) and deeper (dermis) skin layers. These often appear as raised, pigmented spots and generally remain benign throughout life.
Junctional nevi feature nevus cells located at the junction between skin layers. These typically appear as flat, dark spots and may require monitoring due to their location and appearance.
Blue nevi contain specialized cells that create a distinctive blue or blue-black appearance. While usually benign, their unusual coloration often prompts removal for definitive diagnosis.
Cytologic atypia describes abnormal cellular appearance, including irregular size, shape, or internal structure. Mild atypia may be insignificant, while severe atypia requires careful evaluation.
Architectural disorder refers to disorganized growth patterns within the mole. Normal moles show orderly cell arrangements, while atypical moles may display chaotic organization.
Increased cellularity indicates higher-than-normal cell density within the tissue. This finding may suggest active growth or abnormal proliferation.
Melanocytes are specialized cells that produce melanin, the pigment responsible for skin and mole coloration. Most moles consist primarily of melanocytes or related cells.
Melanocytic hyperplasia describes increased numbers of melanin-producing cells. This finding may be normal in certain locations or concerning in others.
Pagetoid spread refers to abnormal melanocyte migration patterns within the skin. This finding often indicates atypical or malignant behavior.
Positive margins in atypical or malignant lesions require immediate attention. This finding suggests incomplete removal and typically necessitates additional surgery or treatment.
High-grade dysplasia indicates significant cellular abnormalities that may progress to cancer. These findings warrant close monitoring and potentially preventive treatment.
Ulceration or tissue breakdown within a mole may suggest aggressive behavior. This finding often prompts additional testing or treatment recommendations.
High mitotic rates combined with other abnormal features may indicate malignant potential. Your healthcare provider will evaluate these findings in context with other pathology results.
Moderate dysplasia typically requires enhanced monitoring through more frequent skin examinations. While not immediately dangerous, these findings indicate increased future risk.
Close margins in atypical lesions may prompt additional tissue removal or careful observation. The specific recommendation depends on the degree of atypia and margin proximity.
Atypical melanocytic proliferation represents a broad category of concerning but not definitively malignant findings. These results often require specialist consultation.
Even completely benign results may warrant ongoing attention if you have multiple atypical moles, family history of skin cancer, or other risk factors.
Irritated or inflamed benign moles might require monitoring to ensure proper healing and rule out recurrence.
Large or numerous benign moles may indicate increased overall skin cancer risk, warranting regular dermatologic surveillance.
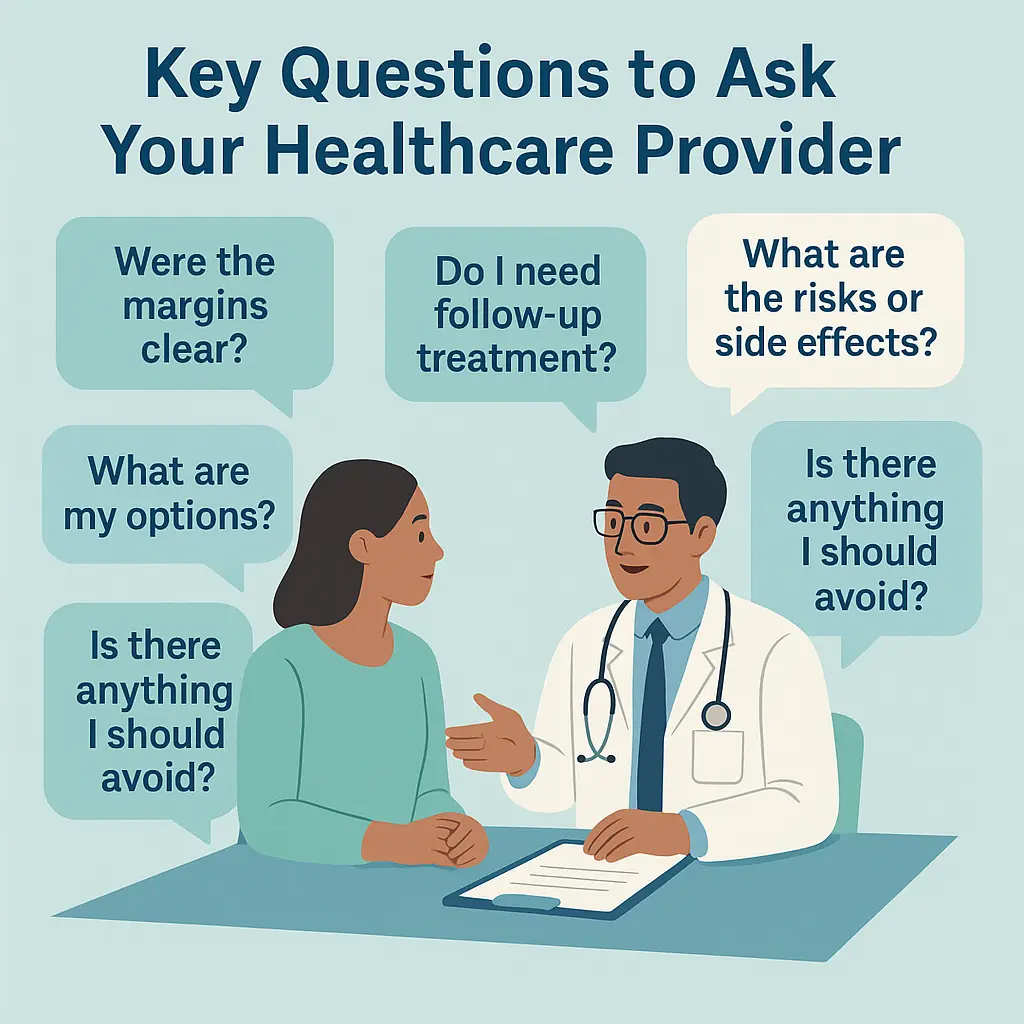
"What specific type of mole was removed?" This fundamental question helps you understand your diagnosis and any associated implications for future skin health.
"Were the margins clear?" Understanding margin status is crucial for determining whether additional treatment is necessary and assessing the completeness of removal.
"Do I need any follow-up treatment?" Some pathology results require additional procedures, while others need only routine monitoring.
"How often should I have skin examinations?" Your pathology results may influence the recommended frequency of future skin cancer screenings.
"Does this result increase my skin cancer risk?" Understanding how your pathology findings affect future cancer risk helps guide prevention strategies.
"Should my family members be screened?" Some pathology findings may have hereditary implications worth discussing with relatives.
"What signs should I watch for?" Knowing specific warning signs relevant to your pathology results empowers proactive monitoring.
"How can I reduce my risk of developing similar growths?" Your healthcare provider can offer personalized prevention recommendations based on your specific situation.
"Are there any lifestyle changes I should make?" Sun protection, diet, and other factors may influence your future skin health.
"Should I see a dermatologist regularly?" Depending on your results and risk factors, specialist care may be beneficial.
Routine monitoring represents the primary recommendation for most benign mole removals. Continue regular skin self-examinations and maintain scheduled healthcare visits.
Sun protection remains crucial regardless of benign results. Use broad-spectrum sunscreen, wear protective clothing, and avoid peak sun exposure hours.
Annual skin examinations may be sufficient for low-risk individuals with benign results, though your healthcare provider may recommend different intervals based on personal risk factors.
Enhanced monitoring typically includes more frequent professional skin examinations and careful self-monitoring for new or changing growths.
Dermatology referral may be recommended for specialized evaluation and ongoing care management.
Photographic documentation of existing moles can help track changes over time and improve early detection of new abnormalities.
Family screening might be advisable since atypical moles can have hereditary components.
Immediate specialist referral is essential for cancer staging, treatment planning, and coordination of care.
Additional testing may include imaging studies, lymph node evaluation, or genetic testing depending on the specific cancer type and stage.
Treatment planning involves developing a comprehensive approach that may include surgery, medication, or other interventions.
Long-term surveillance becomes critically important for monitoring treatment response and detecting any recurrence or new cancers.
"How accurate are pathology reports?" Pathology reports are highly accurate, with error rates typically below 1-2%. However, complex cases may benefit from second opinions or additional testing.
"Why did my doctor remove a mole that looked normal?" Healthcare providers often remove moles based on subtle changes, patient symptoms, or preventive considerations that may not be obvious to patients.
"Can pathology results change over time?" While the original tissue analysis remains constant, your risk assessment and monitoring recommendations may evolve based on new developments or additional findings.
Processing timeframes typically range from 3-7 business days for routine cases. Complex specimens requiring special stains, additional testing, or consultation may take longer.
Factors affecting timing include laboratory workload, specimen complexity, need for additional testing, and requirements for specialist consultation.
Communication protocols vary among healthcare providers. Some offices call with results, while others schedule follow-up appointments or use patient portals for result delivery.
Waiting for results can be stressful. Focus on the fact that most mole removals yield benign results, and early detection and treatment lead to excellent outcomes even for problematic findings.
Understanding terminology helps reduce anxiety by eliminating fear of the unknown. Don't hesitate to ask for clarification of any terms or findings you don't understand.
Support resources including patient education materials, support groups, and counseling services can help manage anxiety related to skin health concerns.
When to consider second opinions include complex diagnoses, borderline findings, or situations where treatment recommendations seem unclear or overly aggressive.
How to obtain second opinions typically involves requesting that your original pathology slides be sent to another pathologist or institution for review.
Insurance considerations often cover second opinion costs, especially for cancer diagnoses or when recommended by your healthcare provider.
Personal risk factors including family history, sun exposure history, skin type, and previous skin cancer influence your ongoing monitoring needs.
Baseline documentation through full-body photography or detailed skin mapping helps track changes over time and improves early detection capabilities.
Monitoring schedules should be individualized based on your pathology results, risk factors, and healthcare provider recommendations.
Sun protection remains the cornerstone of skin cancer prevention. Use broad-spectrum SPF 30+ sunscreen daily, seek shade during peak hours, and wear protective clothing.
Regular self-examinations using the ABCDE criteria (Asymmetry, Border irregularity, Color variation, Diameter >6mm, Evolving characteristics) help identify concerning changes early.
Professional examinations by qualified healthcare providers or dermatologists provide expert evaluation and early detection capabilities beyond self-monitoring.
Mobile apps for mole tracking and skin examination reminders can support your ongoing monitoring efforts.
Dermoscopy and other advanced imaging techniques may be recommended for high-risk individuals or those with numerous atypical moles.
Genetic testing might be considered for individuals with strong family histories of skin cancer or multiple atypical findings.
Demystifying your pathology report after mole removal empowers you to take an active role in your skin health journey. Understanding the terminology, implications, and next steps outlined in your report transforms medical jargon into actionable information that guides your healthcare decisions.
Remember that most mole removals result in benign findings that require only routine monitoring and preventive care. Even atypical or concerning results often have excellent outcomes when detected early and managed appropriately. The key lies in maintaining open communication with your healthcare provider, following recommended monitoring schedules, and staying vigilant about skin changes.
Take action today by reviewing your pathology report with these guidelines in mind, scheduling any recommended follow-up appointments, and implementing a comprehensive skin protection strategy. Your proactive approach to understanding and managing your skin health creates the foundation for lifelong wellness and peace of mind.
Whether your results show benign findings or require additional attention, knowledge remains your most powerful tool for navigating the path forward. Stay informed, stay protected, and stay engaged with your healthcare team to ensure the best possible outcomes for your skin health journey.