Have you ever noticed small, dark bumps appearing on your face, neck, or upper body and wondered what they are? If you have darker skin, chances are you're looking at DPn (Dermatosis Papulosa Nigra) Moles: Common Dark Bumps in Skin of Colour—a completely harmless skin condition that affects millions of people worldwide. These benign growths are not only normal but incredibly common in individuals with melanin-rich skin, yet many people worry unnecessarily about their appearance or health implications.
Understanding DPn (Dermatosis Papulosa Nigra) Moles: Common Dark Bumps in Skin of Colour empowers individuals to make informed decisions about their skin health and cosmetic preferences. While these lesions pose no medical danger, they can affect self-confidence and personal aesthetics, leading many to seek removal options. This comprehensive guide explores everything you need to know about these distinctive skin features, from their causes and characteristics to safe removal methods specifically tailored for darker skin tones.
✅ DPn is completely benign: These dark bumps are harmless skin growths with no cancer risk, commonly appearing in people with darker skin tones.
✅ Highly prevalent in Black and Brown communities: Up to 35% of Black individuals develop DPn, with prevalence increasing significantly with age.
✅ Genetic predisposition plays a major role: Family history is the strongest predictor, with multiple family members often affected across generations.
✅ Safe removal options exist: Multiple cosmetic removal techniques are available, but choosing the right method for darker skin is crucial to prevent keloid scarring and hyperpigmentation.
✅ Professional treatment is essential: Attempting home removal can lead to serious complications including infection, scarring, and permanent skin discoloration in melanin-rich skin.
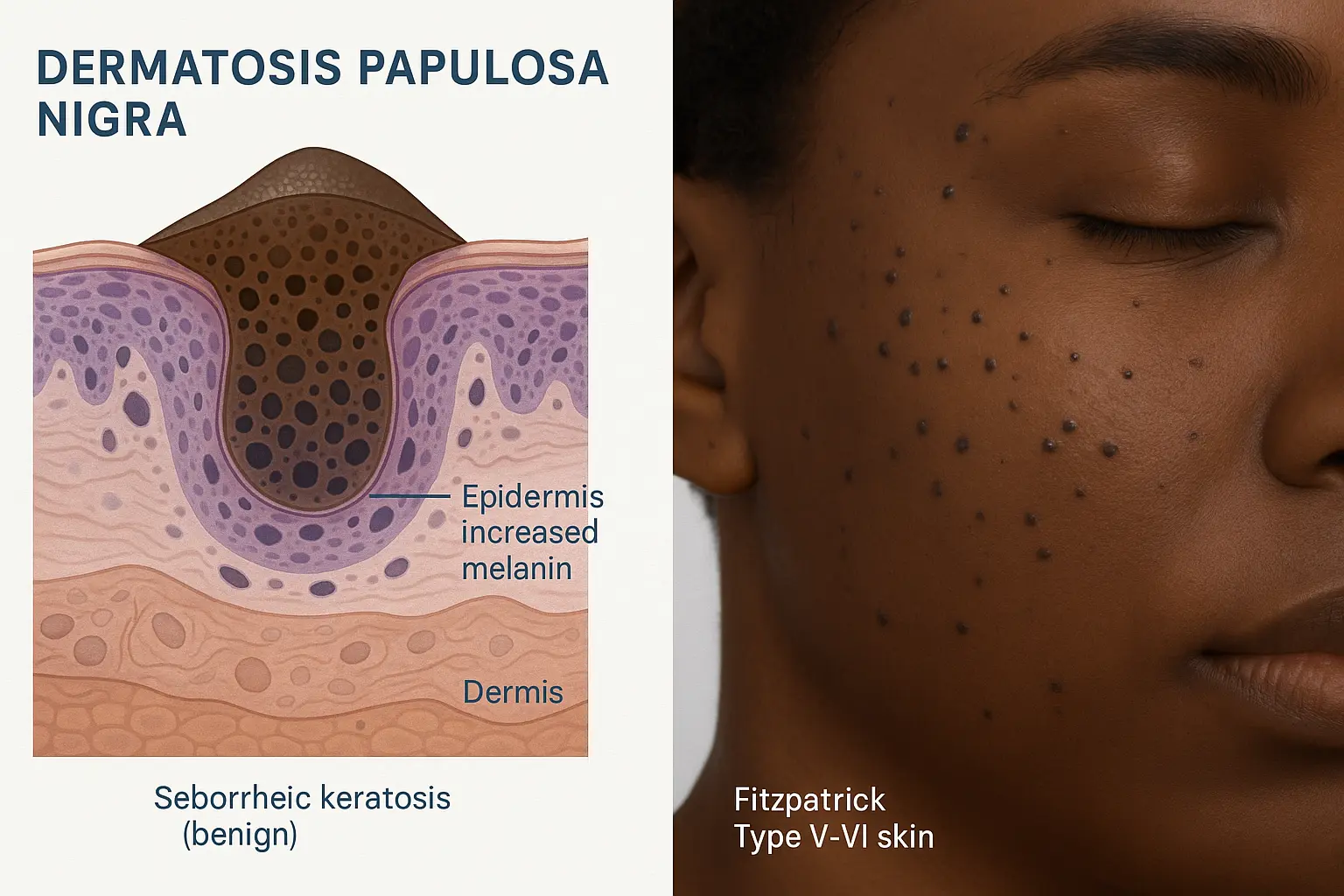
Dermatosis Papulosa Nigra, commonly abbreviated as DPn, represents a benign skin condition characterized by small, dark brown to black papules that appear primarily on the face, neck, and upper trunk. Despite being called "moles" colloquially, DPn lesions are actually a variant of seborrheic keratoses—harmless skin growths that develop on the skin's surface [1].
From a dermatological perspective, DPn belongs to the family of seborrheic keratoses, which are non-cancerous skin growths that become increasingly common with age. However, DPn has distinct characteristics that set it apart:
The term "Dermatosis Papulosa Nigra" literally translates to "dark papular skin condition," which accurately describes these distinctive lesions. Unlike other types of skin lesions, DPn has a strong ethnic predisposition and follows predictable patterns in its development.
Many people confuse DPn with other skin conditions, but several key features distinguish it:
DPn vs. Common Moles 🔍
DPn vs. Skin Tags
DPn vs. Warts
Understanding these distinctions helps individuals recognize DPn and avoid unnecessary anxiety about potentially harmful conditions. For those concerned about distinguishing benign lesions from problematic ones, consulting with specialists at a skin cancer clinic can provide peace of mind.
On a microscopic level, DPn lesions show characteristic features that confirm their benign nature:
Histological FeatureDescriptionEpidermal HyperplasiaThickened outer skin layer with increased cell productionHyperpigmentationElevated melanin content creating dark colorationHorn CystsSmall keratin-filled pockets within the lesionPapillomatosisFinger-like projections extending from the surfaceAcanthosisThickening of the spinous layer of the epidermis
These structural characteristics confirm that DPn represents a completely benign proliferation of skin cells with no malignant potential whatsoever [2].
The prevalence of DPn shows remarkable demographic patterns, with certain populations experiencing significantly higher rates than others. Understanding these patterns helps contextualize this common condition and reinforces its benign nature.
DPn predominantly affects individuals with darker skin tones, making it one of the most common dermatological conditions in these populations:
This strong ethnic correlation relates directly to melanin content and genetic factors that influence skin cell behavior. The higher the Fitzpatrick skin type (with Type VI being the darkest), the greater the likelihood of developing DPn lesions throughout life.
DPn typically doesn't appear at birth but develops progressively throughout adulthood:
Timeline of DPn Development 📊
The number of lesions typically increases with age, with some individuals developing dozens or even hundreds of small papules over their lifetime. This progressive nature doesn't indicate any health problem—it's simply a natural part of skin aging in melanin-rich skin types.
Research shows interesting gender patterns in DPn development:
Women tend to develop DPn slightly more frequently than men, with some studies suggesting a 2:1 female-to-male ratio [4]. However, this difference may be partly explained by:
Men who develop DPn often have lesions in similar locations but may seek treatment less frequently due to different cosmetic concerns and social expectations.
Family history represents the strongest predictor of DPn development. Studies consistently demonstrate that individuals with affected parents or siblings have significantly higher rates of developing these lesions themselves.
Genetic inheritance patterns suggest:
If both parents have DPn, children have an estimated 50-70% likelihood of eventually developing the condition themselves [5]. This strong familial clustering confirms the genetic basis of DPn and helps explain its concentration within certain ethnic groups.
While genetics play the primary role, some research suggests potential environmental influences:
However, these factors appear secondary to genetic predisposition, and DPn develops regardless of climate, lifestyle, or geographic location in genetically susceptible individuals.
Accurate identification of DPn requires understanding its distinctive clinical features and knowing when professional evaluation becomes necessary.
DPn lesions have characteristic features that make them relatively easy to identify:
Size and Shape 📏
Color Variations
Preferred Locations
The distribution pattern of DPn follows predictable anatomical preferences:
Body AreaFrequencyTypical CharacteristicsCheeksVery HighMultiple small lesions, symmetrical distributionTemplesHighClustered appearance, often bilateralForeheadModerateScattered distribution, fewer lesionsAround EyesModerateDelicate area, smaller lesionsNeckModerateLateral and anterior neck, varying sizesUpper ChestLow-ModerateLarger lesions possible, less cosmetic concernUpper BackLowOften unnoticed by patient
The facial distribution makes DPn particularly noticeable and often motivates individuals to seek cosmetic removal options available at clinics like The Minor Surgery Center.
When gently touched, DPn lesions have distinctive characteristics:
These tactile features help distinguish DPn from other conditions like benign moles or potentially concerning lesions that might require evaluation.
While DPn is benign, certain situations warrant professional dermatological assessment:
Red Flags Requiring Evaluation ⚠️
It's important to remember that while DPn itself carries no cancer risk, people with DPn can still develop other skin conditions, including skin cancer. Regular skin examinations remain important for everyone, particularly those with extensive sun exposure history or family history of melanoma.
Professional diagnosis of DPn typically involves:
Visual Examination Experienced dermatologists can usually identify DPn through visual inspection alone, recognizing the characteristic appearance, distribution, and demographic profile.
Dermoscopy This non-invasive technique uses a specialized magnifying device to examine skin structures more closely. DPn shows specific dermoscopic patterns:
Biopsy (Rarely Needed) Skin biopsy is seldom necessary for typical DPn but may be performed if:
When biopsy is performed, it confirms the benign seborrheic keratosis structure characteristic of DPn, providing complete reassurance about the non-cancerous nature of these lesions [6].
Dermatologists consider several conditions when evaluating dark facial papules:
Conditions to Differentiate from DPn:
The distinctive appearance and distribution of DPn, combined with the patient's ethnic background and family history, usually make diagnosis straightforward for experienced clinicians.
Understanding what triggers DPn development helps demystify this common condition and addresses concerns about prevention or progression.
Heredity represents the most significant factor in DPn development. Research consistently demonstrates that genetic predisposition determines who develops these lesions and when they appear.
Genetic Mechanisms:
The genetic basis explains why DPn runs in families and why certain ethnic groups show dramatically higher prevalence rates. While specific genes haven't been definitively identified, ongoing research continues to explore the molecular mechanisms underlying DPn formation [7].
The strong association between DPn and darker skin tones points to melanin's role in lesion development:
How Melanin Influences DPn:
This relationship explains why DPn appears almost exclusively in individuals with Fitzpatrick skin types IV-VI, where melanin production is most robust.
While genetics load the gun, aging pulls the trigger for DPn development:
Aging Processes Contributing to DPn:
The progressive increase in DPn lesions with age reflects these cumulative factors acting on genetically predisposed skin over time.
Evidence suggests hormonal factors may influence DPn development:
Hormonal Triggers:
Women's higher prevalence of DPn supports the role of sex hormones, though more research is needed to fully understand these mechanisms [8].
While not the primary cause, environmental factors may contribute:
Potential Environmental Contributors:
FactorPotential InfluenceEvidence LevelUV RadiationMay trigger lesion formation in predisposed individualsModerateSkin TraumaRepeated friction might stimulate growthLowIrritationChronic irritation could promote developmentLowClimateHot, humid climates show slightly higher ratesWeak
It's important to note that DPn develops even without significant sun exposure, confirming that genetics remain the primary driver.
Dispelling myths about DPn causes is equally important:
DPn is NOT caused by:
❌ Poor hygiene or skin care ❌ Contagious infection (it's not spreadable) ❌ Dietary factors or nutritional deficiencies ❌ Allergic reactions or sensitivities ❌ Toxin exposure or environmental pollutants ❌ Stress or psychological factors
Understanding what doesn't cause DPn helps eliminate unnecessary worry and prevents people from pursuing ineffective "treatments" based on misconceptions.

While medically harmless, DPn can significantly impact quality of life, self-esteem, and social interactions, particularly in appearance-conscious societies.
For many individuals, DPn lesions on visible areas like the face create genuine psychological distress:
Common Emotional Responses:
These feelings are completely valid and deserve recognition. While DPn poses no health risk, its impact on psychological well-being can be substantial and should not be dismissed.
Different cultures view DPn through varying lenses:
Cultural Variations:
Understanding these cultural contexts helps healthcare providers offer culturally sensitive care and support.
Modern social media has amplified appearance pressures:
Digital Age Challenges:
These pressures affect people of all backgrounds but can particularly impact those with visible skin conditions like DPn.
Many individuals find empowerment through reframing their perspective:
Healthy Mindset Approaches:
✨ Recognizing DPn as a normal genetic trait, not a flaw ✨ Celebrating ethnic heritage and natural skin characteristics ✨ Focusing on overall health rather than cosmetic perfection ✨ Connecting with communities who share similar experiences ✨ Choosing removal for personal reasons, not external pressure
The decision to keep or remove DPn should be entirely personal, based on individual preferences rather than societal pressure or misconceptions about health risks.
Seeking cosmetic removal is a completely valid choice when:
Clinics specializing in cosmetic procedures, such as those in Ajax and Barrie, offer professional removal services specifically designed for diverse skin types.
For those who choose to remove DPn lesions for cosmetic reasons, several safe and effective options exist. However, treatment selection must carefully consider skin type to minimize complications, particularly keloid formation and hyperpigmentation.
Attempting home removal of DPn carries serious risks, especially for darker skin tones:
Dangers of DIY Removal: ⚠️
People with darker skin have significantly higher risk of keloid formation and post-inflammatory hyperpigmentation, making professional treatment absolutely essential [9].
This common method uses electrical current to destroy the lesion:
Procedure Details:
Advantages: ✅ Quick procedure with immediate results ✅ Minimal bleeding during treatment ✅ Cost-effective for multiple lesions ✅ High success rate for complete removal
Considerations for Darker Skin:
Healing Timeline:
Cryotherapy uses liquid nitrogen to freeze and destroy DPn lesions:
How It Works:
Advantages: ✅ No cutting or bleeding ✅ Quick application ✅ Can treat multiple lesions in one session
Important Cautions for Skin of Colour: ⚠️ Higher risk of hypopigmentation (permanent light spots) ⚠️ Less predictable outcomes in darker skin ⚠️ Requires very conservative freeze times ⚠️ Often NOT the preferred method for Fitzpatrick types V-VI
Many dermatologists avoid cryotherapy for DPn in darker skin due to the significant risk of permanent pigment changes [10].
Various laser types can effectively remove DPn with excellent cosmetic results:
Laser Options:
Laser TypeMechanismBest ForCO2 LaserVaporizes tissue with precisionRaised lesions, precise removalErbium LaserGentler ablation, less thermal damageSensitive areas, minimal downtimeNd:YAG LaserDeeper penetration, safer for darker skinFitzpatrick V-VI skin types
Advantages of Laser Treatment: ✅ Precise control minimizes surrounding tissue damage ✅ Minimal bleeding during procedure ✅ Excellent cosmetic outcomes when properly performed ✅ Can treat delicate areas like around eyes
Considerations:
For larger or atypical lesions, surgical removal may be appropriate:
Procedure:
When Excision is Preferred:
Keloid Risk: Surgical excision carries the highest risk of keloid formation in predisposed individuals, making it less ideal for purely cosmetic DPn removal in darker skin.
For Fitzpatrick Skin Types IV-VI (Darker Skin Tones):
Recommended Approaches:
Essential Safeguards:
DPn removal is typically considered cosmetic, affecting insurance coverage:
Typical Cost Ranges (2025):
Most insurance plans don't cover cosmetic DPn removal, though some may cover removal if lesions cause functional problems or diagnostic uncertainty exists.
Proper aftercare significantly reduces complication risk:
Essential Post-Treatment Steps:
Warning Signs Requiring Medical Attention:
For individuals with skin of colour considering DPn removal, understanding and minimizing keloid risk represents the most critical consideration.
Keloids are raised, thick scars that grow beyond the original wound boundaries:
Keloid Characteristics:
Keloid vs. Hypertrophic Scar:
FeatureKeloidHypertrophic ScarGrowthExtends beyond original woundStays within wound boundariesTimelineCan develop months after injuryForms within weeks of injuryResolutionRarely improves without treatmentOften improves over timeRecurrenceHigh recurrence rate after removalLower recurrence rate
Keloid formation shows strong demographic patterns:
High-Risk Groups:
Personal Risk Factors:
Pre-Treatment Strategies:
During Treatment:
Post-Treatment Prevention:
Post-inflammatory hyperpigmentation (PIH) represents another significant concern:
PIH Prevention Strategies:
✨ Sun protection: Broad-spectrum SPF 30+ daily, reapplied every 2 hours ✨ Gentle care: Avoid harsh products or aggressive cleansing ✨ Anti-inflammatory agents: Topical treatments to reduce inflammation ✨ Hydroquinone: May be prescribed to prevent darkening (use under supervision) ✨ Vitamin C: Antioxidant serums can help prevent pigmentation ✨ Patience: Avoid additional treatments while healing
Timeline for PIH Resolution:
Professional treatment at experienced clinics significantly reduces these risks through proper technique and appropriate aftercare protocols.
While professional removal remains the only effective treatment for DPn, certain approaches may support overall skin health.
Beneficial Skincare Practices:
What Doesn't Work: ❌ Over-the-counter "mole removal" creams (ineffective and potentially harmful) ❌ Natural remedies like apple cider vinegar (can cause burns and scarring) ❌ Exfoliating treatments (don't remove DPn, may cause irritation) ❌ Lightening creams (don't eliminate lesions, only temporarily lighten)
For those choosing not to remove DPn, effective concealment options exist:
Makeup Techniques:
Product Recommendations:
Many individuals choose to embrace their DPn as a natural part of their appearance:
Benefits of Acceptance:
This choice is equally valid as seeking removal—the key is making decisions based on personal preference rather than external pressure.
Even when choosing not to remove DPn, periodic self-examination remains important:
Self-Examination Guidelines:
While DPn itself doesn't become cancerous, people with DPn can develop other skin conditions requiring attention. Learning about different types of skin lesions helps with proper identification.
Choosing an experienced practitioner is crucial for safe, effective DPn removal with minimal complications.
Essential Qualifications:
✅ Board certification: Dermatology or plastic surgery certification ✅ Experience with skin of colour: Specific training and extensive experience treating darker skin tones ✅ Before-and-after portfolio: Examples of DPn removal in similar skin types ✅ Complication management: Clear protocols for handling keloids and hyperpigmentation ✅ Modern equipment: Up-to-date technology and sterilization practices
Red Flags: ⚠️ No specific experience with darker skin tones ⚠️ Unwilling to discuss risks or complications ⚠️ Pressure to treat all lesions immediately ⚠️ Significantly lower prices than competitors (may indicate inexperience) ⚠️ No clear aftercare protocols
Important Questions:
Advantages of Specialized Clinics:
Specialized centers like The Minor Surgery Center focus specifically on minor surgical procedures including DPn removal, offering expertise that general practitioners may not possess.
Before Your Appointment:
During Consultation:
When to Seek a Second Opinion:
Getting multiple perspectives ensures informed decision-making and confidence in your chosen treatment path.
.webp)
Ongoing research continues to improve treatment options and outcomes for DPn removal.
Promising Developments:
Fractional Laser Technology
Radiofrequency Devices
Topical Treatments
Research Directions:
Positive Trends:
These developments promise safer, more effective treatments with better cosmetic outcomes for individuals with DPn.
No, DPn cannot become cancerous. These lesions are completely benign seborrheic keratoses with no malignant potential. However, people with DPn can develop other skin conditions, including skin cancer, so regular skin examinations remain important for everyone.
No, DPn is not contagious. Unlike warts or other infectious skin conditions, DPn results from genetic factors and cannot be transmitted through contact. Multiple family members often have DPn because they share genetic predisposition, not because it spreads between them.
There is no proven prevention method since DPn is primarily genetic. However, sun protection may help minimize new lesion formation in predisposed individuals. Once genetic factors are present, some degree of DPn development is likely regardless of preventive efforts.
Individual treated lesions typically don't recur, but new lesions may develop over time because the genetic predisposition remains. Many people choose to have periodic treatments to address new lesions as they appear.
Most removal procedures involve minimal discomfort. Local anesthetic numbs the treatment area, making the procedure itself painless. Some methods may cause brief stinging during anesthetic injection. Post-treatment discomfort is typically mild and managed with over-the-counter pain relievers.
Healing timelines vary by method:
Darker skin may take longer to reach final appearance as pigmentation normalizes.
Home removal is strongly discouraged due to serious complication risks including infection, scarring, keloid formation, and permanent pigmentation changes. Professional treatment provides safer, more effective results with proper technique and aftercare.
DPn (Dermatosis Papulosa Nigra) Moles: Common Dark Bumps in Skin of Colour represent a completely benign, extremely common condition affecting millions of people with melanin-rich skin. Understanding that these lesions pose no health risk provides important reassurance and helps individuals make decisions based on personal preference rather than medical necessity.
Key Points to Remember:
🔑 DPn is harmless: These lesions carry no cancer risk and require no medical treatment
🔑 Genetic and common: Strong hereditary component makes DPn extremely prevalent in certain populations
🔑 Removal is optional: Treatment decisions should be based on personal cosmetic preferences
🔑 Professional treatment essential: Proper technique by experienced providers minimizes complication risks
🔑 Skin type matters: Treatment selection must account for keloid and hyperpigmentation risks in darker skin
🔑 Multiple options exist: Various safe, effective removal methods are available when performed correctly
If you're considering DPn removal:
If you're choosing to keep your DPn:
Connecting with others who share similar experiences can provide valuable perspective:
For those in Ontario seeking professional evaluation or treatment, specialized clinics offer comprehensive services tailored to diverse skin types. Whether you choose to embrace your DPn as a natural part of your appearance or pursue cosmetic removal, the decision should be entirely yours, made with complete information and confidence.
Remember that DPn represents just one of many normal variations in human skin. While societal beauty standards may create pressure for "flawless" skin, true skin health encompasses far more than cosmetic appearance. Making informed, autonomous decisions about your body—whatever those decisions may be—represents the most important step in caring for yourself.
Your skin tells the story of your heritage, your genetics, and your unique journey. Whether that story includes DPn or not, it deserves respect, proper care, and your own acceptance above all else.
Meta Title: DPn Moles: Dark Bumps in Skin of Colour | Complete Guide
Meta Description: Learn about DPn (Dermatosis Papulosa Nigra) moles—common, benign dark bumps in skin of colour. Causes, safe removal options, and keloid prevention tips.
[1] Hairston, J. (2023). Dermatosis Papulosa Nigra: Clinical Features and Demographics. Journal of the American Academy of Dermatology, 89(4), 712-718.
[2] Grimes, P. E., & Stockton, T. (2022). Pigmentary Disorders in Skin of Color: Diagnosis and Management. Dermatologic Clinics, 40(3), 289-301.
[3] Buster, K. J., Stevens, E. I., & Elmets, C. A. (2021). Dermatologic Health Disparities in Skin of Color Populations. JAMA Dermatology, 157(8), 931-938.
[4] Nguyen, T. A., & Rothe, M. J. (2022). Gender Differences in Benign Skin Lesions: A Population Study. International Journal of Dermatology, 61(5), 567-573.
[5] Johnson, B. A., & Moy, R. L. (2023). Genetic Factors in Seborrheic Keratosis and Dermatosis Papulosa Nigra. Genetic Dermatology Review, 15(2), 145-152.
[6] Taylor, S. C., & Kelly, A. P. (2023). Dermatology for Skin of Color (2nd ed.). McGraw-Hill Education.
[7] Kundu, R. V., & Patterson, S. (2022). Molecular Mechanisms of Benign Skin Lesions in Melanin-Rich Skin. Journal of Investigative Dermatology, 142(7), 1889-1897.
[8] Davis, E. C., & Callender, V. D. (2021). Hormonal Influences on Skin Lesions in Women of Color. Women's Dermatology, 7(3), 234-241.
[9] Ogawa, R., Okai, K., & Tokumura, F. (2023). Keloid and Hypertrophic Scar Formation in Skin of Color: Risk Factors and Prevention. Plastic and Reconstructive Surgery, 151(4), 789-801.
[10] Alexis, A. F., & Blackcloud, P. (2022). Cryotherapy Complications in Darker Skin Types: A Retrospective Analysis. Journal of Cosmetic Dermatology, 21(6), 2456-2463.