Every year, millions of people notice a new or changing mole and face a critical question: does it need to be tested, or does it need to come off entirely? The answer often comes down to understanding the difference between a mole biopsy and a mole removal — two procedures that sound similar but serve very different purposes. Whether a mole is causing cosmetic concern or raising a red flag for skin cancer, knowing which procedure is right can make all the difference. This comprehensive guide on mole biopsy vs mole removal breaks down everything — from what each procedure involves and why it's done, to recovery timelines, costs, and how to decide which option fits a specific situation.
Skin health awareness has never been higher, and with good reason. Skin cancer remains one of the most common cancers worldwide, and early detection through proper biopsy techniques saves lives. At the same time, many people simply want a bothersome or unsightly mole removed for cosmetic reasons. Understanding the distinction between these two approaches is the first step toward making an informed, confident decision.
Before diving deeper into mole biopsy vs mole removal, it helps to understand what a mole actually is.
A mole (medically called a nevus) is a common skin growth that occurs when pigment-producing cells called melanocytes cluster together. Moles can appear anywhere on the body, and most adults have between 10 and 40 moles by the time they reach adulthood [3].
Moles come in many forms:
Most moles are completely harmless — what dermatologists call benign moles. However, certain changes in a mole's appearance can signal the development of melanoma or other types of skin cancer. This is exactly where the decision between biopsy and removal becomes important.
💡 Did You Know? The ABCDE rule is a simple way to monitor moles: Asymmetry, Border irregularity, Color variation, Diameter larger than 6mm, and Evolving shape or size. Any of these signs warrant a professional evaluation.
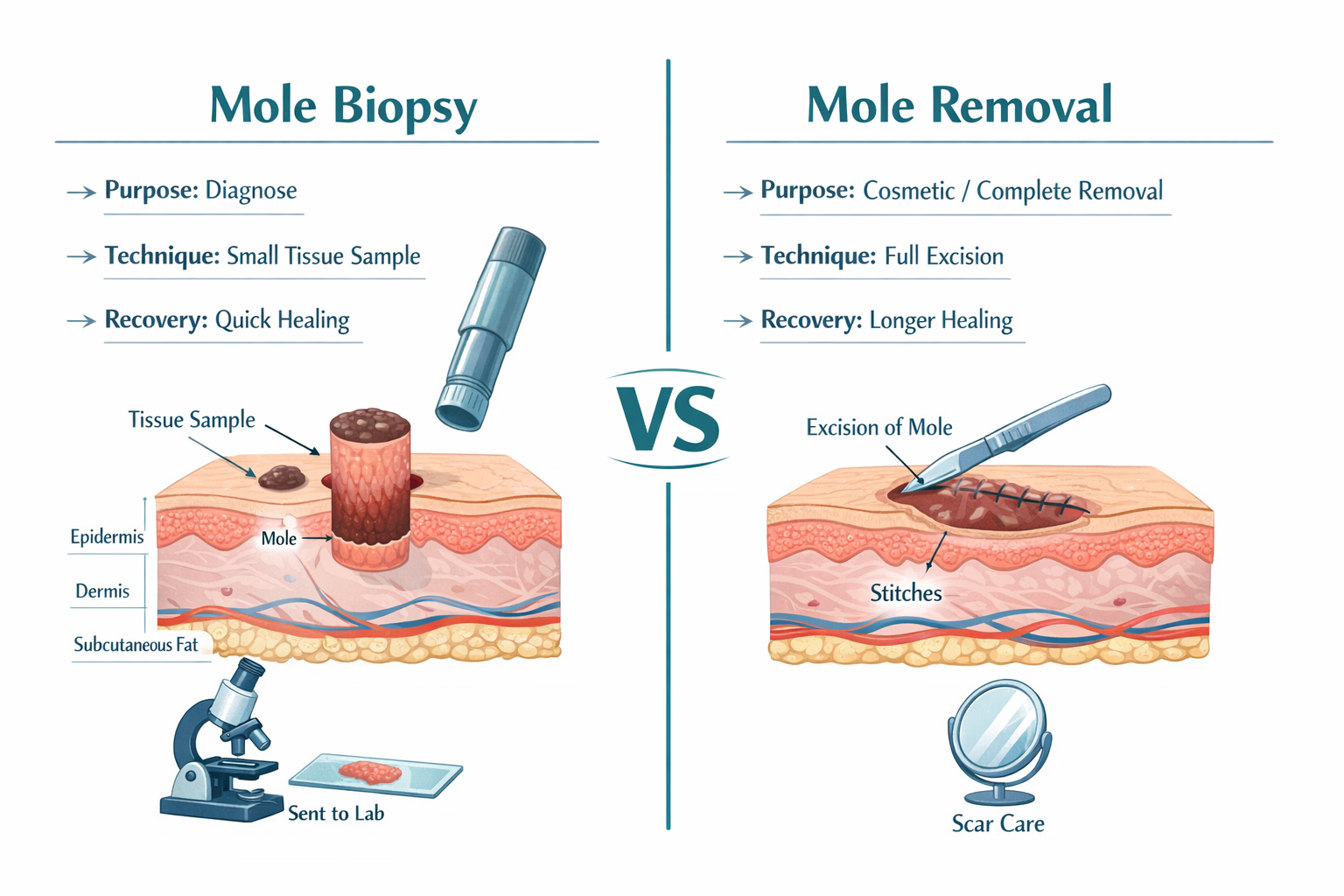
A mole biopsy is a medical procedure in which a small sample of tissue is removed from a mole and sent to a laboratory for microscopic examination. The primary goal is diagnosis — determining whether the mole contains abnormal, precancerous, or cancerous cells [4][5].
A biopsy does not necessarily remove the entire mole. Instead, it focuses on gathering enough tissue to give a pathologist the information needed to make an accurate diagnosis [1].
A dermatologist or physician may recommend a mole biopsy when:
The biopsy answers one critical question: Is this mole dangerous?
Not all biopsies are the same. The method chosen depends on the mole's characteristics, location, and the level of suspicion for malignancy [5].
Biopsy TypeHow It WorksBest ForDepthShave BiopsyA thin blade shaves off the top layers of the moleRaised or superficial molesShallowPunch BiopsyA circular tool punches out a small, cylindrical core of tissueFlat moles or deeper lesionsModerate to deepExcisional BiopsyThe entire mole is cut out along with a margin of surrounding skinHighly suspicious molesFull depthIncisional BiopsyA portion of a large mole is removed for testingVery large moles where full removal isn't practicalVaries
The excisional biopsy is considered the gold standard for suspicious moles because it removes the entire lesion and sends it for pathological review [5]. In many cases, an excisional biopsy can serve as both a diagnostic and therapeutic procedure — meaning if the mole turns out to be benign, no further treatment is needed.
Here's what to expect step by step [7][9]:
After receiving results, patients can learn more about interpreting their findings through resources like this guide on demystifying your pathology report after mole removal.
Recovery from a mole biopsy is generally quick and straightforward [1]:
Mole removal is a procedure designed to completely eliminate a mole from the skin. Unlike a biopsy, which focuses on diagnosis, removal is a treatment — either for cosmetic reasons or because the mole has been identified as medically concerning [1][2].
Mole removal involves excising the entire mole, including its deeper roots, and typically requires local anesthesia and suturing (stitches) to close the wound [1].
The reasons for mole removal generally fall into two categories:
Cosmetic Reasons:
For those considering aesthetic procedures, cosmetic mole removal techniques have advanced significantly in recent years.
Medical Reasons:
Removal MethodDescriptionIdeal ForStitches Required?Surgical ExcisionThe mole is cut out with a scalpel along with a margin of healthy tissueSuspicious or deep molesYesShave ExcisionThe mole is shaved off at or just below the skin surfaceRaised, benign molesUsually noLaser RemovalA laser destroys the mole tissueSmall, flat, non-cancerous molesNoCryotherapyLiquid nitrogen freezes and destroys the moleSmall, superficial molesNoCurettage & ElectrodesiccationThe mole is scraped off and the base is cauterizedSuperficial benign molesNo
⚠️ Important: Laser removal and cryotherapy destroy the mole tissue, meaning no sample is available for pathology testing. These methods should only be used when a mole has already been confirmed as benign [5][10].
For patients curious about freezing techniques, learning about cryotherapy for mole removal can help clarify what to expect.
The surgical excision process follows these general steps [8][9]:
Many patients wonder does mole removal hurt? The honest answer is that the local anesthetic eliminates pain during the procedure, though mild soreness afterward is normal.
Recovery from a full mole removal takes longer than a simple biopsy [1][9]:
For a detailed recovery timeline, this resource on how long mole removal takes to heal provides helpful guidance.
Now that both procedures have been explored individually, here is a comprehensive comparison to clarify the differences in the mole biopsy vs mole removal debate:
FeatureMole BiopsyMole RemovalPrimary PurposeDiagnosis (testing for cancer)Treatment (eliminating the mole)Tissue RemovedSmall sample or partial moleEntire mole + marginSent to Lab?AlwaysUsually (except laser/cryo)AnesthesiaLocalLocalStitchesSometimes (1–2)Usually (multiple)Procedure Time10–20 minutes20–45 minutesRecovery Time1–3 weeks2–4 weeks+ScarringMinimalModerate (depends on method)CostGenerally lowerGenerally higherFollow-up NeededIf results are abnormalSuture removal + healing checkCan It Be Cosmetic?No (purely diagnostic)YesCan It Be Medical?YesYes
🔑 Key Insight: An excisional biopsy can sometimes serve as both a biopsy AND a removal — if the entire mole is excised for testing and the results come back benign, no further procedure is needed [5].
✅ A mole has recently changed in appearance ✅ There are suspicious features (asymmetry, irregular borders, multiple colors) ✅ A dermatologist wants to rule out melanoma or other skin cancers ✅ The mole is new and unusual, especially after age 30 ✅ There's a family history of skin cancer ✅ The goal is information, not elimination
✅ A biopsy has already confirmed abnormal or cancerous cells ✅ The mole is cosmetically bothersome ✅ The mole is in a location where it's frequently irritated (under bra straps, waistband, collar) ✅ A doctor recommends preventive removal of an atypical mole ✅ The patient wants the mole permanently gone ✅ Multiple moles need to be addressed — many clinics can remove multiple moles in one visit
It's worth emphasizing that the line between biopsy and removal isn't always clear-cut. The excisional biopsy sits at the intersection of both procedures:
Research from NYU Langone found that using a 2-millimeter margin during initial excision achieved complete mole removal in over 90% of cases, and no recurrent suspicious growths were found in monitored patients over 18 months [6]. This finding supports the effectiveness of excisional biopsy as a combined diagnostic and therapeutic approach.
One of the most important technical differences between a simple biopsy and a full removal is the concept of surgical margins.
A surgical margin refers to the ring of normal, healthy skin removed along with the mole. Margins serve as a safety buffer to ensure that no abnormal cells are left behind.
If a mole is cancerous, adequate margins are critical to prevent recurrence. The NYU Langone study demonstrated that a 2-millimeter margin was sufficient for complete removal in the vast majority of cases involving suspicious moles [6]. For confirmed melanoma, wider margins (up to 1–2 centimeters) may be recommended depending on the cancer's depth.
Understanding margins helps explain why mole removal typically results in a larger wound and more noticeable scar than a biopsy.
Both mole biopsies and mole removals are considered safe, low-risk procedures when performed by qualified medical professionals. However, as with any medical procedure, there are potential risks to be aware of.
⚠️ A common concern: Many patients worry that disturbing a mole through biopsy could "spread" cancer. Medical evidence does not support this fear. Biopsy is a safe and essential diagnostic tool, and there is no credible evidence that it causes cancer to spread [5]. For more on this topic, read about whether removing a mole causes cancer.
Cost is often a practical factor in the decision-making process. Here's a general breakdown of what to expect in 2026:
For a more detailed cost breakdown, this resource on mole removal costs provides additional information.

Preparation for either procedure is relatively simple, but taking the right steps can improve the experience and outcome [7]:
Seek medical attention if any of the following occur:
Yes — an excisional biopsy removes the entire mole for testing. If the results are benign, no further procedure is needed, effectively making it both a biopsy and a removal [5].
Not always. If a mole is clearly benign and being removed for cosmetic reasons, a biopsy may not be required beforehand. However, the removed tissue should still be sent for pathological analysis as a precaution [10].
Use the ABCDE rule as a starting guide, and see a dermatologist for any mole that is asymmetric, has irregular borders, shows color variation, is larger than 6mm, or is evolving in any way. A professional evaluation with dermoscopy provides the most reliable assessment. Learn more about identifying healthy vs. early cancerous moles.
In most cases, a properly removed mole will not grow back. However, if removal is incomplete (some cells are left behind), regrowth is possible [8]. Surgical excision with adequate margins provides the lowest recurrence rate.
Medically necessary procedures — including biopsies for suspicious moles and removal of confirmed cancerous or precancerous moles — are typically covered by insurance. Cosmetic removals are generally not covered and are considered out-of-pocket expenses [2].
The decision is best made in consultation with a doctor. If there's any suspicion of cancer, a biopsy (or excisional biopsy) is the medically appropriate first step. If the mole is clearly benign and the goal is cosmetic improvement, removal can be discussed directly.
A mole biopsy typically takes 10 to 20 minutes, while a full surgical removal may take 20 to 45 minutes depending on the mole's size and location [1].
Selecting a qualified, experienced clinic is essential for both safety and optimal results. Here's what to look for:
For guidance on finding a reputable provider, explore this resource on choosing the best mole removal clinic.
Whether a person ultimately needs a biopsy, a removal, or neither, regular skin monitoring is the single most important habit for catching problems early.
Advances in technology continue to improve both the diagnosis and treatment of moles:
These innovations are making the mole biopsy vs mole removal decision more nuanced and personalized than ever before.
Understanding the difference between a mole biopsy and mole removal empowers patients to have informed conversations with their healthcare providers and make confident decisions about their skin health.
Here's a quick summary of the key distinctions:
The bottom line? Don't ignore a changing mole, and don't fear the procedures designed to protect you. Both mole biopsies and mole removals are safe, effective, and routinely performed — and the right choice depends on individual circumstances, medical history, and the professional judgment of a qualified physician.
Your skin is your body's largest organ. Treat it with the attention it deserves. 🌟
[1] Mole Removal Vs Mole Biopsy Whats The Difference - https://chicagofacialcosmetics.com/mole-removal-vs-mole-biopsy-whats-the-difference/
[2] Mole Removal Vs Mole Biopsy Understanding The Differences - https://chicagofacialcosmetics.com/mole-removal-vs-mole-biopsy-understanding-the-differences/
[3] Mole Removal - https://rendoncenter.com/clinical-dermatology/mole-removal/
[4] Mole Removal Biopsy - https://facebyfisher.com/mole-removal-biopsy/
[5] Dermatology Perspective On Mole Removal - https://wisconsinplasticsurgery.com/blog/dermatology-perspective-on-mole-removal/
[6] Doctors Define Safe Effective Margins One Done Skin Removal Around Suspicious Moles - https://nyulangone.org/news/doctors-define-safe-effective-margins-one-done-skin-removal-around-suspicious-moles
[7] How To Prepare For A Skin Biopsy Or Mole Removal - https://www.skincancerandderm.com/blog/1339792-how-to-prepare-for-a-skin-biopsy-or-mole-removal/
[8] Is Mole Removal Really Effective - https://advanceddermatologyctr.com/is-mole-removal-really-effective/
[9] What To Expect When You Have A Mole Removed - https://www.mdanderson.org/cancerwise/what-to-expect-when-you-have-a-mole-removed.h00-159775656.html
[10] How To Remove A Non Cancerous Mole Medical Options - https://www.scripps.org/news_items/4584-how-to-remove-a-non-cancerous-mole-medical-options