When Sarah noticed a small, dark mole on her shoulder changing shape, her doctor recommended removal for testing. Like many patients, her first concern wasn't the procedure itself—it was whether can removing a mole cause cancer. This fear stops countless individuals from seeking necessary medical care, potentially putting their health at risk.
The relationship between mole removal and cancer development is one of the most misunderstood topics in dermatology. While concerns about medical procedures are natural, understanding the science behind mole removal can help patients make informed decisions about their skin health.
Mole removal is one of the most common minor surgical procedures performed worldwide, with millions of cases completed safely each year. Yet persistent myths continue to circulate, suggesting that disturbing a mole might somehow trigger cancerous changes or cause existing cancer cells to spread throughout the body.
• Removing a mole does not cause cancer - the procedure eliminates abnormal tissue rather than creating it
• Proper surgical techniques ensure complete removal with minimal risk of complications
• Early detection and removal of suspicious moles significantly improves treatment outcomes
• Professional evaluation is essential for determining which moles require removal
• Post-removal care and regular skin monitoring help maintain optimal skin health
Moles, medically known as nevi, represent clusters of pigmented cells called melanocytes that develop when these cells grow in groups rather than spreading evenly throughout the skin. Most individuals develop between 10 to 40 moles during their lifetime, with the majority appearing during childhood and adolescence.
The formation process involves several factors:
Genetic predisposition plays a significant role, as family history strongly influences mole development patterns. Individuals with parents or siblings who have numerous moles typically develop more moles themselves.
Sun exposure accelerates mole formation, particularly during childhood years when skin is most vulnerable to ultraviolet radiation damage. This explains why moles commonly appear on sun-exposed areas like the face, arms, and back.
Hormonal changes during puberty, pregnancy, and menopause can trigger new mole development or cause existing moles to change in appearance.
Understanding different mole types helps patients recognize when professional evaluation becomes necessary:
Common Moles (Acquired Nevi)
Congenital Moles
Atypical Moles (Dysplastic Nevi)
Cancer development involves a complex process where normal cells undergo genetic mutations that cause uncontrolled growth and division. These mutations typically accumulate over time through various factors including genetic predisposition, environmental exposures, and cellular aging.
The transformation from normal cells to cancerous ones follows a predictable pattern:
When melanoma develops within a mole, the cancerous changes occur at the cellular level long before any surgical intervention. Research indicates that approximately 20-30% of melanomas arise from existing moles, while the majority develop in previously normal skin.
The question can removing a mole cause cancer becomes irrelevant when understanding that cancerous changes either exist before removal or don't exist at all. Surgical removal cannot create genetic mutations that weren't already present.
Extensive medical research spanning decades has consistently demonstrated that removing a mole does not cause cancer. This conclusion stems from multiple lines of evidence:
Cellular Biology: Cancer requires specific genetic mutations within cell DNA. Physical removal of tissue cannot create these mutations—it simply eliminates the cells entirely.
Clinical Studies: Large-scale studies following thousands of patients after mole removal show no increased cancer rates compared to individuals who never had moles removed.
Pathological Analysis: When removed moles undergo laboratory examination, pathologists can determine whether cancerous changes existed before removal. These findings consistently show that cancer, when present, preceded the surgical procedure.
Several persistent myths continue to worry patients considering mole removal:
Myth: "Cutting into a mole spreads cancer cells throughout the body" Reality: Proper surgical techniques include wide margins and complete removal, preventing any theoretical cell dispersal. Additionally, if cancer isn't present before surgery, there are no cancer cells to spread.
Myth: "Air exposure during surgery activates dormant cancer cells" Reality: Cancer cells don't remain "dormant" waiting for air exposure. Cells are either cancerous or normal—there's no intermediate state activated by surgical exposure.
Myth: "Disturbing a mole triggers malignant transformation" Reality: Malignant transformation requires genetic mutations that develop over time through various factors, not mechanical disruption.
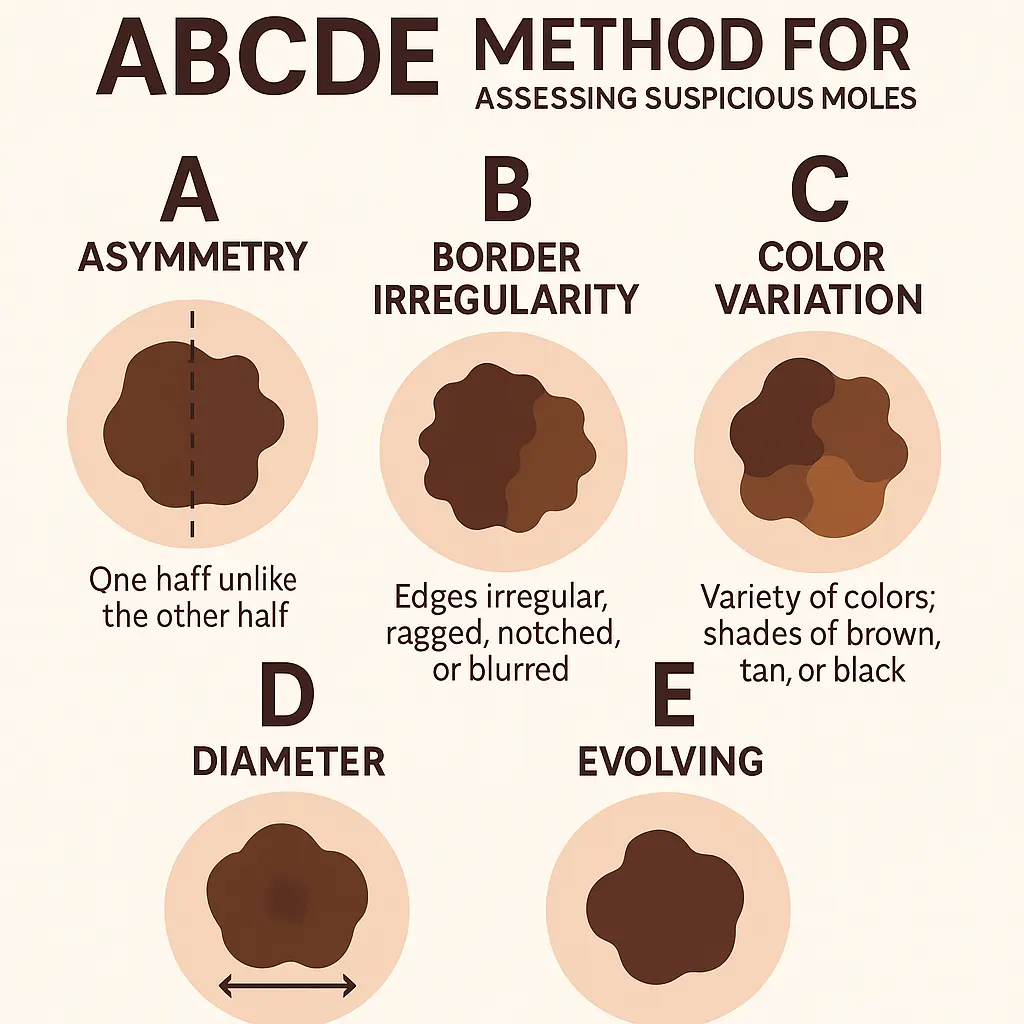
Professional mole removal begins with comprehensive evaluation using established criteria. Dermatologists employ the ABCDE method for assessing suspicious moles:
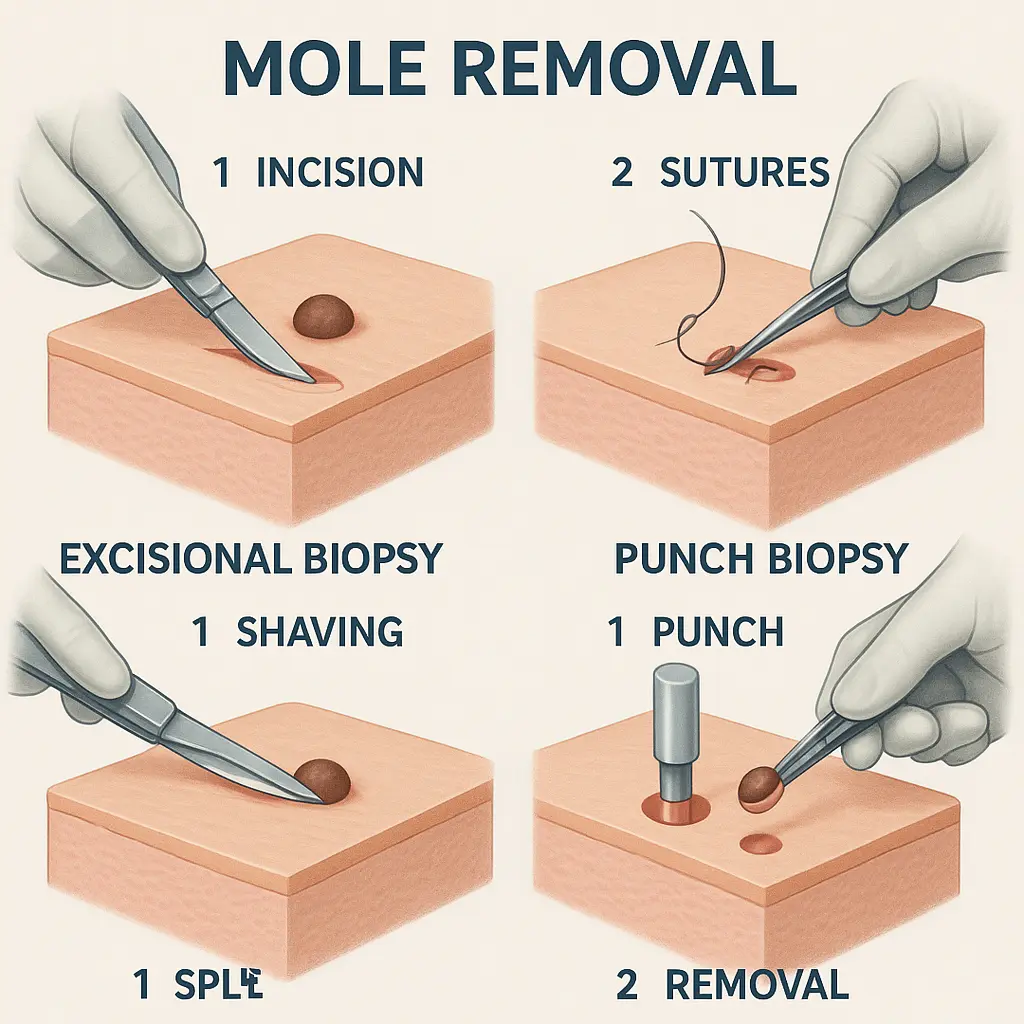
Modern mole removal employs several proven techniques, each selected based on mole characteristics and location:
Excisional Biopsy This method involves complete mole removal with surrounding healthy tissue margins. The procedure ensures complete elimination while providing adequate tissue for pathological examination.
Shave Biopsy Surface-level removal using a specialized blade works well for raised moles that don't extend deep into skin layers. This technique leaves minimal scarring while removing visible mole tissue.
Punch Biopsy A circular cutting tool removes cylindrical tissue sections, ideal for small, deep moles requiring complete removal down to subcutaneous layers.
Every removed mole undergoes microscopic examination by board-certified pathologists. This analysis determines:
The pathological report provides definitive answers about whether cancer existed before removal, conclusively addressing concerns about can removing a mole cause cancer.
Healthcare providers recommend mole removal for several specific reasons:
Suspicious Appearance Changes Any mole exhibiting ABCDE characteristics requires prompt evaluation and likely removal for definitive diagnosis.
Bleeding or Irritation Moles that spontaneously bleed, itch persistently, or become tender may indicate underlying changes requiring investigation.
Location-Related Issues Moles in areas prone to frequent trauma (such as under bra straps or collar lines) may require removal to prevent ongoing irritation.
Family History Concerns Individuals with strong family histories of melanoma may benefit from prophylactic removal of atypical moles.
Beyond medical necessity, many patients choose mole removal for aesthetic reasons. Cosmetic removal remains safe and effective when performed by qualified professionals, regardless of whether medical concerns exist.
Professional mole removal provides several immediate benefits for patient health and well-being:
Definitive Diagnosis Complete pathological analysis eliminates uncertainty about mole characteristics, providing peace of mind or enabling prompt treatment if abnormalities are discovered.
Prevention of Progression Early removal of atypical or pre-cancerous moles prevents potential progression to invasive cancer, significantly improving long-term outcomes.
Symptom Relief Removal eliminates ongoing irritation, bleeding, or discomfort associated with problematic moles.
The long-term advantages of appropriate mole removal extend far beyond immediate concerns:
Reduced Monitoring Burden Removing suspicious moles simplifies future skin surveillance, allowing patients and healthcare providers to focus attention on remaining moles and new developments.
Improved Quality of Life Elimination of cosmetically bothersome moles or those causing physical discomfort enhances daily comfort and self-confidence.
Baseline Establishment Professional removal and analysis establish clear baselines for future skin health monitoring, making it easier to detect new concerning changes.
While mole removal is generally safe, patients should understand potential complications to make informed decisions:
Infection Risk Like any surgical procedure, mole removal carries a small infection risk, typically less than 1-2% when proper post-operative care is followed.
Scarring All surgical procedures result in some degree of scarring, though modern techniques minimize this concern. Scar appearance depends on factors including:
Incomplete Removal Rarely, deep or extensive moles may require additional procedures to ensure complete removal, particularly if initial pathology reveals concerning features at removal margins.
When considering can removing a mole cause cancer, patients must weigh the minimal risks of removal against the potentially serious consequences of leaving suspicious moles untreated:
Removal Risks:
Non-Removal Risks:
The risk-benefit analysis clearly favors removal when medical professionals recommend the procedure.
Proper aftercare significantly influences healing outcomes and minimizes complication risks:
Wound Care Protocol
Activity Modifications
Monitoring for Complications Patients should contact their healthcare provider if they experience:
Successful mole removal represents just one component of comprehensive skin health management:
Regular Self-Examinations Patients should perform monthly skin checks, examining all body areas for new moles or changes in existing ones. This includes areas not easily visible, requiring assistance from family members or mirrors.
Professional Surveillance Dermatological follow-up schedules depend on individual risk factors:
Photographic Documentation Many dermatology practices now employ digital photography systems to document baseline skin appearance, making future change detection more accurate and objective.
Leading medical organizations worldwide have established clear positions regarding mole removal safety:
American Academy of Dermatology The AAD strongly supports appropriate mole removal when indicated, emphasizing that proper surgical techniques pose no cancer risk while providing significant diagnostic and therapeutic benefits.
International Society of Dermatology Global dermatological experts consistently recommend prompt removal of suspicious moles, noting that delays in removal pose far greater health risks than the procedures themselves.
American Cancer Society Cancer specialists advocate for aggressive early detection and removal strategies, particularly for individuals with elevated melanoma risk factors.
Modern mole removal follows evidence-based protocols developed through decades of clinical research:
Surgical Margin Guidelines Current standards recommend removing 2-5 millimeters of normal-appearing skin around suspicious moles to ensure complete elimination of abnormal cells.
Pathological Review Requirements All removed moles must undergo histopathological examination by board-certified pathologists to determine the presence or absence of cancerous changes.
Follow-Up Care Standards Standardized follow-up protocols ensure appropriate wound healing monitoring and long-term surveillance for new skin concerns.
Mole removal procedures typically involve minimal discomfort due to effective local anesthesia. Most patients report feeling only slight pressure during the procedure, with mild soreness for 24-48 hours afterward that responds well to over-the-counter pain medications.
Healing timelines vary based on several factors:
Individual healing rates depend on age, overall health, location of removal, and adherence to aftercare instructions.
Insurance coverage depends on the medical necessity of the procedure:
Patients should verify coverage details with their insurance providers before scheduling procedures.
Modern dermatology employs sophisticated technologies to enhance mole evaluation accuracy:
Dermoscopy This specialized magnification technique allows dermatologists to examine mole structures invisible to the naked eye, improving diagnostic accuracy by up to 30%.
Digital Imaging Systems High-resolution photography enables precise documentation of mole characteristics, facilitating accurate comparison during follow-up examinations.
Artificial Intelligence Analysis Emerging AI technologies assist dermatologists in identifying subtle pattern changes that might indicate malignant transformation.
Technological advances continue to improve mole removal procedures:
Laser Removal Appropriate for certain superficial moles, laser technology offers precise tissue removal with minimal surrounding tissue damage.
Radiofrequency Surgery This technique provides excellent precision and hemostasis, reducing bleeding and improving cosmetic outcomes.
Cryotherapy Applications Controlled freezing techniques work well for specific benign mole types, offering quick procedures with minimal discomfort.
While the question can removing a mole cause cancer focuses on treatment concerns, prevention remains the most effective strategy for maintaining skin health:
Daily Sunscreen Use
Protective Clothing
Behavioral Modifications
Understanding and managing personal risk factors helps prevent problematic mole development:
Genetic Counseling Individuals with strong family histories of melanoma may benefit from genetic counseling to understand inherited risk factors and develop appropriate surveillance strategies.
Regular Monitoring Establishing baseline skin examinations and maintaining regular follow-up schedules enables early detection of concerning changes.
Lifestyle Factors Maintaining overall health through proper nutrition, regular exercise, and stress management supports optimal immune function and skin health.
Selecting an appropriately qualified healthcare provider ensures optimal outcomes for mole removal procedures:
Board Certification Choose providers certified by recognized dermatology or plastic surgery boards, indicating completion of rigorous training and ongoing education requirements.
Experience Levels Inquire about provider experience with mole removal procedures, particularly for complex cases or cosmetically sensitive locations.
Facility Accreditation Ensure procedures are performed in accredited facilities meeting established safety and quality standards.
Informed patients achieve better outcomes by asking relevant questions during consultations:
Ongoing research continues to improve mole assessment and removal techniques:
Genetic Testing Advances Researchers are developing more sophisticated genetic tests to identify individuals at highest risk for melanoma development, enabling more targeted surveillance strategies.
Biomarker Development Scientists are investigating blood and tissue biomarkers that might predict mole behavior, potentially identifying concerning moles before visible changes occur.
Immunotherapy Applications Early-stage research explores whether immunotherapy approaches might prevent progression of atypical moles to invasive cancer.
Future developments promise to further improve patient care:
Telemedicine Applications Remote mole monitoring using smartphone photography and AI analysis may enable more frequent surveillance without requiring office visits.
Precision Medicine Approaches Personalized treatment recommendations based on individual genetic profiles and risk factors will likely become standard practice.
Minimally Invasive Techniques Continued technological development aims to reduce procedure invasiveness while maintaining diagnostic accuracy and therapeutic effectiveness.
The question can removing a mole cause cancer reflects understandable patient concerns about medical procedures. However, comprehensive scientific evidence clearly demonstrates that professional mole removal does not cause cancer. Instead, appropriate removal of suspicious moles represents one of the most effective strategies for preventing cancer progression and ensuring optimal patient outcomes.
Understanding the facts about mole removal empowers patients to make informed healthcare decisions. The procedure's minimal risks pale in comparison to the potential consequences of leaving suspicious moles untreated. Modern surgical techniques, combined with expert pathological analysis, provide definitive diagnosis while eliminating concerning tissue.
Patients considering mole removal should focus on selecting qualified healthcare providers and following recommended aftercare protocols rather than worrying about unfounded cancer risks. Regular skin monitoring, sun protection practices, and prompt professional evaluation of concerning changes form the foundation of effective skin health management.
For individuals with suspicious moles or those seeking professional evaluation, consulting with qualified dermatologists provides the expertise necessary for optimal outcomes. The Minor Surgery Center offers comprehensive mole evaluation and removal services, ensuring patients receive evidence-based care from experienced professionals.
Remember that early detection and appropriate treatment significantly improve outcomes for all skin conditions, including melanoma. Don't let unfounded fears about can removing a mole cause cancer prevent you from seeking necessary medical care. Professional evaluation and treatment, when indicated, provide the best protection for your long-term skin health.
Take charge of your skin health today by scheduling regular dermatological examinations and addressing any concerning changes promptly. Your skin—and your peace of mind—will benefit from proactive, informed healthcare decisions based on scientific evidence rather than persistent myths.