When you think of melanoma, you probably picture a dark, irregular mole. But what if the most dangerous skin cancer didn't look dark at all?
Amelanotic melanoma is a rare and often overlooked form of skin cancer that appears pink, red, or even skin-colored—making it one of the most challenging skin cancers to detect early. Unlike typical melanomas that show up as dark spots, amelanotic melanoma produces little to no pigment, which means it can easily be mistaken for a harmless bump, scar, or irritated skin.
This lack of color isn't just a cosmetic difference—it's a diagnostic challenge that can delay treatment and put lives at risk. Understanding what amelanotic melanoma looks like, who's at risk, and when to seek help can make all the difference in catching this cancer early.
At The Minor Surgery Center, our experienced surgical team specializes in safe and efficient surgery for suspicious skin lesions. We believe in expert outpatient care delivered with a comfort-first approach, helping you get back to your life with peace of mind.
Amelanotic melanoma lacks typical dark pigmentation, appearing pink, red, skin-colored, or colorless—making it harder to spot than traditional melanomas.
Amelanotic melanoma is a subtype of melanoma—the most serious form of skin cancer—where the malignant cells produce little to no melanin, the pigment that gives skin, hair, and moles their color [1].
The word "amelanotic" literally means "without melanin." While most melanomas appear as dark brown or black spots, amelanotic melanoma breaks this pattern entirely.
Research shows that approximately 5% of all melanomas are amelanotic [2]. However, the percentage varies depending on the location:
These statistics matter because they highlight just how often this cancer can hide in plain sight.
Melanin production is controlled by melanocytes—the same cells that become cancerous in melanoma. In amelanotic melanoma, these cells have lost their ability to produce pigment while still maintaining their capacity to grow aggressively and spread.
Think of it like a burglar who's turned off the alarm system. The danger is still there, but the warning signal you'd normally rely on is silent.
This biological quirk makes amelanotic melanoma particularly dangerous. Without the dark color that typically alerts people to melanoma, these lesions often go unnoticed until they've grown larger or spread deeper into the skin.
Unlike the dark, irregular moles associated with typical melanoma, amelanotic melanoma can appear in several deceptive forms [4].
Pink or Red Lesions
The most common presentation is a pink or red bump or patch that might look like:
Skin-Colored or Colorless
Some amelanotic melanomas match your surrounding skin tone exactly, appearing as:
Subtle Pigmentation
Early amelanotic melanomas may show faint hints of color:
Changing Characteristics
What makes these lesions particularly concerning is their evolution:
Amelanotic melanoma can develop anywhere on the body, but common locations include:
For a comprehensive understanding of various skin lesions and how they differ, explore our guide on 25 types of skin lesions explained.
The biggest challenge with amelanotic melanoma is that it doesn't follow the rules we've been taught to watch for.
For decades, dermatologists have taught patients to look for the ABCDE warning signs of melanoma [5]:
Amelanotic melanoma often fails to trigger these traditional red flags because:
Because of its atypical appearance, amelanotic melanoma is frequently mistaken for [6]:
Benign Conditions:
Other Skin Cancers:
This diagnostic confusion often leads to delayed treatment. Studies show that amelanotic melanomas are typically diagnosed at more advanced stages compared to pigmented melanomas [7].
To better understand different types of skin cancer and their characteristics, read our article on 4 types of skin cancer.
To improve detection of amelanotic melanoma, experts now recommend expanding the traditional criteria to include the "3 R's" [8]:
These additional warning signs better capture the appearance of amelanotic melanomas and can help you identify concerning lesions earlier.
While amelanotic melanoma can affect anyone, certain factors increase your risk [9].
Personal or Family History
If you or a close family member has had melanoma, your risk increases significantly. Genetic factors play a role in melanoma susceptibility.
Sun Exposure History
Blistering sunburns, especially in childhood, dramatically increase melanoma risk. Research shows that five or more blistering sunburns before age 20 substantially elevate your lifetime risk [10].
Skin Type and Coloring
People with certain physical characteristics face higher risk:
Age and Gender
While melanoma can occur at any age, risk increases with age. Certain subtypes of amelanotic melanoma show different patterns in men versus women.
Weakened Immune System
People with compromised immune systems—whether from organ transplants, HIV/AIDS, or immunosuppressive medications—face increased melanoma risk.
Previous Skin Cancers
A history of any skin cancer, including basal cell or squamous cell carcinoma, increases your risk for melanoma.
Atypical Moles
Having many moles or unusual-looking moles (dysplastic nevi) raises melanoma risk. Learn more about atypical moles and their significance.
Occupational or Recreational UV Exposure
Jobs or hobbies that involve prolonged sun exposure without adequate protection increase risk over time.
It's important to remember that having risk factors doesn't guarantee you'll develop amelanotic melanoma. Conversely, people without obvious risk factors can still develop this cancer.
The key is awareness and vigilance—knowing what to look for and taking action when something doesn't seem right.
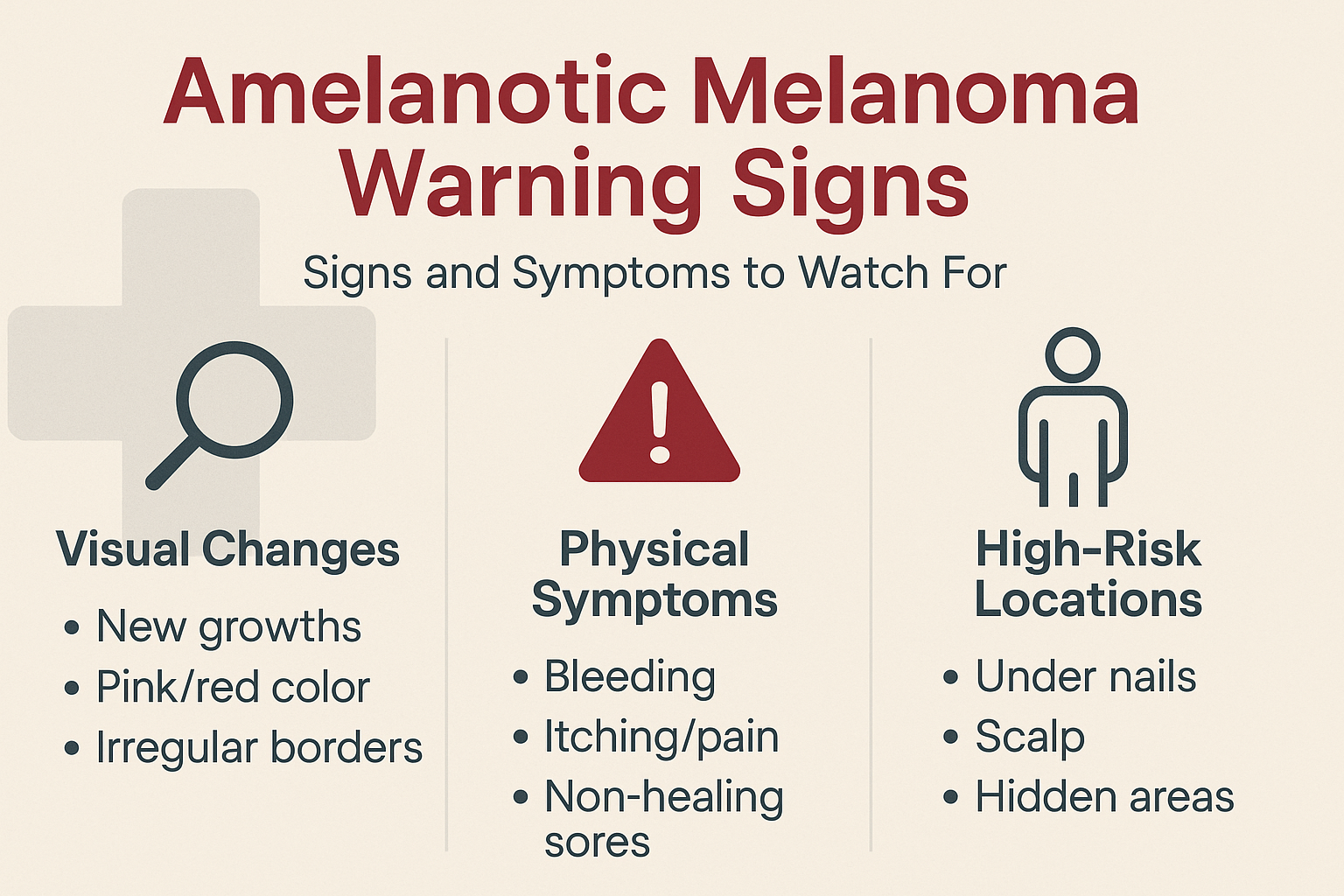
Recognizing the warning signs of amelanotic melanoma can save your life. Here's what to monitor [11].
New Growths
Any new spot, bump, or patch that appears on your skin deserves attention, especially if it:
Color Characteristics
While amelanotic melanomas lack dark pigmentation, watch for:
Shape and Border
Even without dark color, concerning features include:
Bleeding or Oozing
Lesions that bleed spontaneously or with minimal trauma are concerning. This includes:
Itching or Tenderness
Unusual sensations in a skin lesion warrant evaluation:
Non-Healing Sores
A sore or wound that doesn't heal within a few weeks is a red flag, especially if it:
Subungual (Under Nails)
Amelanotic melanoma under fingernails or toenails may appear as:
For more information on this specific presentation, read about acral melanoma, which includes subungual melanomas.
Scalp and Hidden Areas
Melanomas in areas you can't easily see require extra vigilance:
Early and accurate diagnosis of amelanotic melanoma requires a combination of clinical expertise and advanced diagnostic tools [12].
Visual Inspection
Your healthcare provider will carefully examine the suspicious lesion and surrounding skin, looking for:
Dermoscopy
Dermoscopy (also called dermatoscopy) uses a specialized magnifying device with polarized light to examine skin lesions in detail. This tool helps identify subtle features not visible to the naked eye, including:
For amelanotic melanomas, dermoscopy can reveal distinctive vascular patterns—such as dotted, linear, or irregular vessels—that raise suspicion for melanoma even without pigmentation [13].
When Biopsy Is Needed
If a lesion appears suspicious, your provider will recommend a biopsy—the only definitive way to diagnose amelanotic melanoma.
Types of Biopsy
Several biopsy methods may be used:
At The Minor Surgery Center, we perform expert outpatient care for skin lesion biopsies and removal, using minimally invasive solutions with a personalised treatment plan tailored to your needs.
What Happens to the Sample
The tissue sample is sent to a pathology laboratory where a specialist examines it under a microscope. The pathologist looks for:
Breslow Thickness
One of the most important prognostic factors is the Breslow thickness—the measurement of how deeply the melanoma has invaded the skin, measured in millimeters [14].
Sentinel Lymph Node Biopsy
For thicker melanomas or those with certain high-risk features, your doctor may recommend a sentinel lymph node biopsy to determine if cancer has spread to nearby lymph nodes.
Imaging Studies
Depending on the stage and characteristics of the melanoma, imaging tests may be ordered:
These help determine if the cancer has spread to other parts of the body.
To understand more about melanoma progression, explore our article on advanced melanoma stages.
Treatment for amelanotic melanoma follows the same principles as treatment for pigmented melanoma, with the primary goal being complete removal of the cancer [15].
Wide Local Excision
The standard treatment for amelanotic melanoma is surgical excision with adequate margins. This means:
The Procedure
Surgical excision is typically performed as an outpatient procedure under local anesthesia. The process involves:
At The Minor Surgery Center, our experienced surgical team specializes in safe and efficient surgery for melanoma removal, providing expert outpatient care with a comfort-first approach.
Mohs Surgery
For melanomas in cosmetically sensitive areas (like the face), Mohs micrographic surgery may be considered. This technique allows for precise removal while preserving as much healthy tissue as possible.
Sentinel Lymph Node Biopsy
For melanomas with certain risk features, a sentinel lymph node biopsy may be performed during the same surgery as the wide excision. This procedure:
Lymph Node Dissection
If cancer is found in sentinel lymph nodes or if lymph nodes are clinically enlarged, complete lymph node dissection may be recommended to remove all nodes in that region.
For amelanotic melanomas that have spread beyond the original site, additional treatments may include [16]:
Immunotherapy
Medications that help your immune system recognize and attack melanoma cells:
Targeted Therapy
For melanomas with specific genetic mutations (like BRAF mutations):
Radiation Therapy
May be used for:
Chemotherapy
Less commonly used now due to more effective immunotherapy and targeted therapy options, but may be considered in certain situations.
After treatment, regular follow-up is essential:
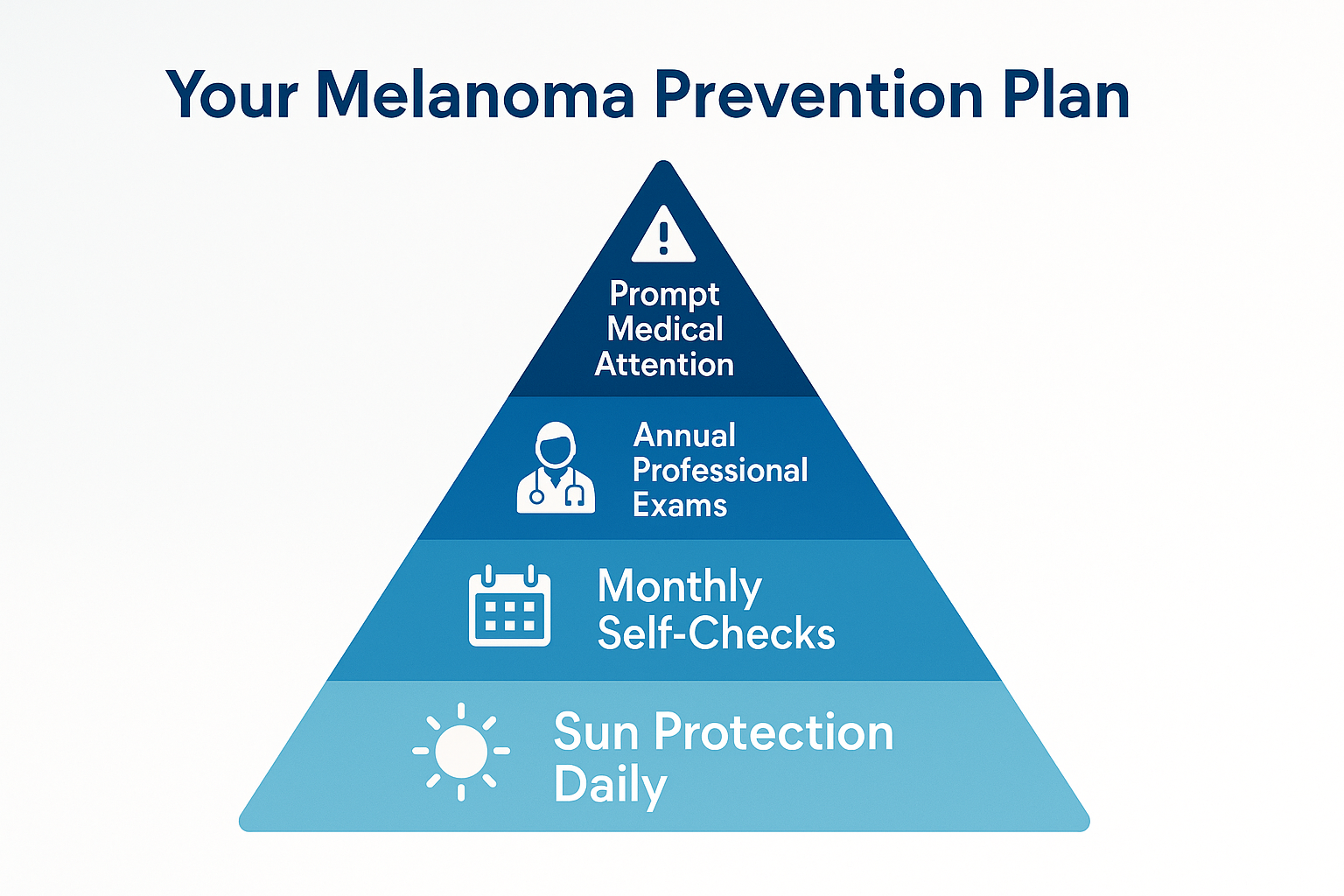
While you can't completely eliminate your risk of amelanotic melanoma, you can take meaningful steps to reduce it and catch problems early [17].
Daily Sunscreen Use
Apply broad-spectrum sunscreen with SPF 30 or higher:
Protective Clothing
Physical barriers provide excellent protection:
Seek Shade
Minimize direct sun exposure, especially during peak hours:
Avoid Tanning Beds
Indoor tanning significantly increases melanoma risk. There is no such thing as a "safe tan" from tanning beds.
For a comprehensive understanding of UV exposure and protection, check out our complete UV index guide.
Monthly Skin Checks
Perform thorough self-examinations once a month:
What to Look For
During self-exams, watch for:
Partner Checks
Have a partner, family member, or friend check areas you can't easily see:
Annual Dermatology Visits
Schedule yearly full-body skin exams with a dermatologist or qualified healthcare provider, especially if you have:
High-Risk Surveillance
If you're at elevated risk, your doctor may recommend:
Don't Wait
If you notice any concerning changes, don't adopt a "wait and see" approach. Early detection dramatically improves outcomes.
Contact a healthcare provider promptly if you notice:
At The Minor Surgery Center, we understand that skin concerns can be worrying. Our team provides expert assessment and personalised treatment plans to address suspicious lesions promptly and professionally.
A diagnosis of amelanotic melanoma naturally brings concerns about the future. Understanding what to expect can help you navigate this journey with confidence [18].
Initial Reactions
It's completely normal to experience a range of emotions after diagnosis:
Seeking Support
You don't have to face this alone:
Managing Anxiety
Practical strategies to cope with cancer-related anxiety:
After Surgery
Recovery from melanoma excision typically involves:
Managing Side Effects
If you require additional treatments like immunotherapy or targeted therapy:
Sun Protection Becomes Non-Negotiable
After melanoma, sun protection isn't optional:
Vigilant Monitoring
Ongoing surveillance becomes part of your life:
Healthy Living
While no lifestyle changes can guarantee prevention of recurrence, general health supports overall wellbeing:
Prognosis Factors
The outlook for amelanotic melanoma depends on several factors [19]:
Survival Rates
When caught early, melanoma is highly curable:
These statistics emphasize why early detection is so critical.
Hope and Advances
Treatment for melanoma has advanced dramatically in recent years:
At The Minor Surgery Center, we believe in helping you get back to your life. A melanoma diagnosis is serious, but with proper treatment and follow-up, many people go on to live full, active lives.
Our comfort-first approach means we support you not just through treatment, but in your journey toward recovery and wellness.
Understanding how amelanotic melanoma differs from other skin conditions helps explain why it's so often misdiagnosed [20].
Similarities:
Differences:
Learn more about basal cell carcinoma treatment options.
Similarities:
Differences:
For information on precancerous lesions, read about actinic keratosis.
Similarities:
Differences:
To understand normal moles better, explore our article on benign moles explained.
Similarities:
Differences:
For more information on cysts, visit our guide on 17 types of cysts.
Similarities:
Differences:
The bottom line: If you can't tell whether a lesion is concerning or benign, it's always better to have it evaluated by a healthcare professional.
At The Minor Surgery Center, our experienced surgical team can assess suspicious lesions and provide expert guidance on whether removal or biopsy is warranted.
Yes, amelanotic melanoma can be completely colorless or skin-colored. However, many have subtle hints of pink, red, tan, or grey, especially at the edges. The key is that they lack the dark brown or black pigmentation typical of most melanomas.
Growth rate varies, but amelanotic melanomas can grow relatively quickly compared to benign lesions. Some may develop over weeks to months, while others progress more slowly. Any lesion that's noticeably changing deserves prompt evaluation.
Yes, amelanotic melanoma can appear as a new lesion that wasn't there before. However, it can also develop from a pre-existing mole that loses its pigmentation. This is why monitoring both new and existing spots is important.
Amelanotic melanoma isn't inherently more aggressive biologically, but it tends to be diagnosed at later stages because it's harder to recognize. This delayed diagnosis can lead to worse outcomes, making early detection especially critical.
Yes, amelanotic melanoma can occur in people of all skin tones, including those with dark skin. In fact, because melanoma in darker-skinned individuals is often diagnosed later, awareness of atypical presentations like amelanotic melanoma is particularly important.
Don't wait or try to self-diagnose. Contact a healthcare provider—preferably a dermatologist—for evaluation. If you're in the Toronto area, The Minor Surgery Center offers expert assessment and treatment of suspicious skin lesions with a personalised treatment plan.
While you can't prevent all melanomas, you can significantly reduce your risk through sun protection, avoiding tanning beds, and monitoring your skin. Early detection through regular self-exams and professional skin checks is your best defense.
Most melanoma excisions can be closed with standard surgical techniques. For larger excisions or those in cosmetically sensitive areas, your surgeon may use plastic surgery techniques to optimize the cosmetic outcome. Our experienced surgical team at The Minor Surgery Center prioritizes both complete cancer removal and optimal cosmetic results.
Follow-up schedules vary based on the stage of your melanoma and other risk factors. Typically, you'll have exams every 3-6 months for the first few years, then annually. Your healthcare provider will create a surveillance plan tailored to your situation.
Melanoma can recur, either at the original site (local recurrence), in nearby lymph nodes (regional recurrence), or in distant organs (metastatic recurrence). This is why lifelong surveillance is essential after melanoma treatment.
When it comes to amelanotic melanoma, professional expertise makes all the difference [21].
While self-awareness and monthly skin checks are valuable, they have limitations:
Think of self-exams as your early warning system, but professional evaluation as your diagnostic confirmation.
Comprehensive Assessment
A thorough skin examination includes:
Clear Communication
Healthcare providers should:
Timely Action
When a lesion is suspicious:
Experience Matters
Look for providers with:
Comfort and Trust
You should feel:
At The Minor Surgery Center, we combine expert outpatient care with a comfort-first approach. Our experienced surgical team specializes in minimally invasive solutions for suspicious skin lesions, helping you get back to your life with confidence and peace of mind.
Consider getting a second opinion if:
Trust your instincts. You know your body better than anyone.
The field of melanoma research is rapidly evolving, bringing hope for better detection and treatment [22].
Artificial Intelligence and Machine Learning
Researchers are developing AI algorithms that can:
Advanced Imaging Techniques
New technologies under investigation include:
Molecular and Genetic Testing
Research into genetic markers may help:
Immunotherapy Breakthroughs
Recent years have seen remarkable progress:
Targeted Therapy Expansion
For melanomas with specific genetic mutations:
Vaccine Development
Melanoma vaccines are being investigated:
Biomarker Discovery
Scientists are searching for:
Risk Prediction Models
Advanced algorithms combining:
These models may help identify who needs more intensive surveillance.
While amelanotic melanoma presents unique challenges, ongoing research offers hope for:
Knowledge is powerful, but action saves lives. Here's what to do with the information you've learned [23].
Examine Your Skin Today
Set aside 15 minutes for a thorough self-examination:
Schedule Professional Evaluation
If you find anything suspicious:
Assess Your Risk Factors
Review the risk factors discussed in this article:
Understanding your risk helps you determine appropriate surveillance frequency.
Make Sun Protection a Habit
Starting today:
Establish a Skin Check Routine
Create a sustainable system:
Schedule Annual Professional Exams
Make skin health a priority:
Share What You've Learned
Help others by:
Advocate for Yourself
In healthcare settings:
Don't let anyone dismiss your concerns. You are your own best advocate.
Choose the Right Healthcare Team
When you need evaluation or treatment:
At The Minor Surgery Center, we understand that skin concerns can be worrying. Our experienced surgical team provides expert outpatient care for suspicious lesions, combining minimally invasive solutions with a comfort-first approach.
We believe in:
Our goal is simple: help you get back to your life with confidence and peace of mind.
Amelanotic melanoma may be challenging to detect, but awareness and vigilance make all the difference.
By knowing what to look for, examining your skin regularly, protecting yourself from sun damage, and seeking professional evaluation when needed, you're taking powerful steps to protect your health.
Don't let the lack of dark color fool you. Pink, red, or skin-colored lesions that are new, changing, or just don't look right deserve attention.
Your life is worth protecting. Take action today.
Amelanotic melanoma represents one of skin cancer's most deceptive forms—a serious malignancy hiding in plain sight without the dark pigmentation we've been taught to watch for.
This lack of color isn't just a curiosity; it's a diagnostic challenge that can delay detection and potentially impact outcomes. When melanoma appears pink, red, or skin-colored, it can easily be mistaken for harmless bumps, scars, or other benign conditions.
But knowledge changes everything.
By understanding that melanoma doesn't always look dark, by learning to watch for the "3 R's" (Red, Raised, Recent change), and by staying vigilant about any new or changing skin lesions, you're equipped to catch this cancer early when treatment is most effective.
The key messages to remember:
✓ Amelanotic melanoma lacks dark pigmentation but is just as serious as typical melanoma
✓ Traditional ABCDE criteria may not apply—expand your awareness to include atypical presentations
✓ Any new, changing, or unusual lesion deserves professional evaluation—don't wait or self-diagnose
✓ Sun protection and regular skin checks are your best defense against all forms of melanoma
✓ Early detection dramatically improves outcomes—when caught early, melanoma is highly curable
If you've discovered a suspicious lesion or simply want peace of mind about a changing spot, don't hesitate to seek expert evaluation. At The Minor Surgery Center, our experienced surgical team provides expert outpatient care for skin lesions, combining minimally invasive solutions with a personalised treatment plan and comfort-first approach.
We're here to help you get back to your life—free from worry, pain, and uncertainty.
Your skin tells a story. Make sure you're paying attention to what it's saying.
For more information about skin health and minor surgical procedures, visit our blog for comprehensive resources and expert guidance.
[1] Gong HZ, Zheng HY, Li J. Amelanotic melanoma. Melanoma Res. 2019;29(3):221-230.
[2] Koch SE, Lange JR. Amelanotic melanoma: the great masquerader. J Am Acad Dermatol. 2000;42(5 Pt 1):731-734.
[3] Cheung WL, Patel RR, Leonard A, Firoz B, Meehan SA. Amelanotic melanoma: a detailed morphologic analysis with clinicopathologic correlation of 75 cases. J Cutan Pathol. 2012;39(1):33-39.
[4] Giuliano AE, Cochran AJ, Morton DL. Melanoma from unknown primary site and amelanotic melanoma. Semin Oncol. 1982;9(4):442-447.
[5] American Academy of Dermatology. Melanoma warning signs and images. AAD.org. 2025.
[6] Menzies SW, Kreusch J, Byth K, et al. Dermoscopic evaluation of amelanotic and hypomelanotic melanoma. Arch Dermatol. 2008;144(9):1120-1127.
[7] Jaimes N, Braun RP, Thomas L, Marghoob AA. Clinical and dermoscopic characteristics of amelanotic melanomas that are not of the nodular subtype. J Eur Acad Dermatol Venereol. 2012;26(5):591-596.
[8] Zalaudek I, Kreusch J, Giacomel J, Ferrara G, Catricala C, Argenziano G. How to diagnose nonpigmented skin tumors: a review of vascular structures seen with dermoscopy: part II. Nonmelanocytic skin tumors. J Am Acad Dermatol. 2010;63(3):377-386.
[9] American Cancer Society. Melanoma skin cancer risk factors. Cancer.org. 2025.
[10] Dennis LK, Vanbeek MJ, Beane Freeman LE, Smith BJ, Dawson DV, Coughlin JA. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Ann Epidemiol. 2008;18(8):614-627.
[11] Pizzichetta MA, Stanganelli I, Bono R, et al. Dermoscopic features of difficult melanoma. Dermatol Surg. 2007;33(1):91-99.
[12] Argenziano G, Soyer HP, Chimenti S, et al. Dermoscopy of pigmented skin lesions: results of a consensus meeting via the Internet. J Am Acad Dermatol. 2003;48(5):679-693.
[13] Menzies SW. Evidence-based dermoscopy. Dermatol Clin. 2013;31(4):521-524.
[14] Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27(36):6199-6206.
[15] National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Melanoma. Version 1.2025.
[16] Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al. Overall survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2017;377(14):1345-1356.
[17] Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur J Cancer. 2005;41(1):45-60.
[18] Kasparian NA, McLoone JK, Butow PN. Psychological responses and coping strategies among patients with malignant melanoma: a systematic review of the literature. Arch Dermatol. 2009;145(12):1415-1427.
[19] Gershenwald JE, Scolyer RA, Hess KR, et al. Melanoma staging: Evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(6):472-492.
[20] Pizzichetta MA, Talamini R, Stanganelli I, et al. Amelanotic/hypomelanotic melanoma: clinical and dermoscopic features. Br J Dermatol. 2004;150(6):1117-1124.
[21] Carli P, De Giorgi V, Chiarugi A, et al. Addition of dermoscopy to conventional naked-eye examination in melanoma screening: a randomized study. J Am Acad Dermatol. 2004;50(5):683-689.
[22] Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115-118.
[23] Skin Cancer Foundation. Skin cancer facts & statistics. SkinCancer.org. 2025.