You wake up one morning, look in the mirror, and notice small yellowish patches near the inner corners of your eyes. They weren't there before—or maybe they were, but now they're impossible to ignore. These cholesterol deposits, known as xanthelasma, can make you feel self-conscious and wondering if there's an easy fix. Enter the world of xanthelasma removal cream products flooding online marketplaces with bold promises of dissolving these stubborn deposits without surgery. But do these creams actually work, or are they just another expensive skincare disappointment?
This comprehensive guide examines the science, effectiveness, and reality behind xanthelasma removal creams. Whether you're considering purchasing one of these products or exploring alternative treatment options, understanding what works—and what doesn't—can save you both money and frustration.
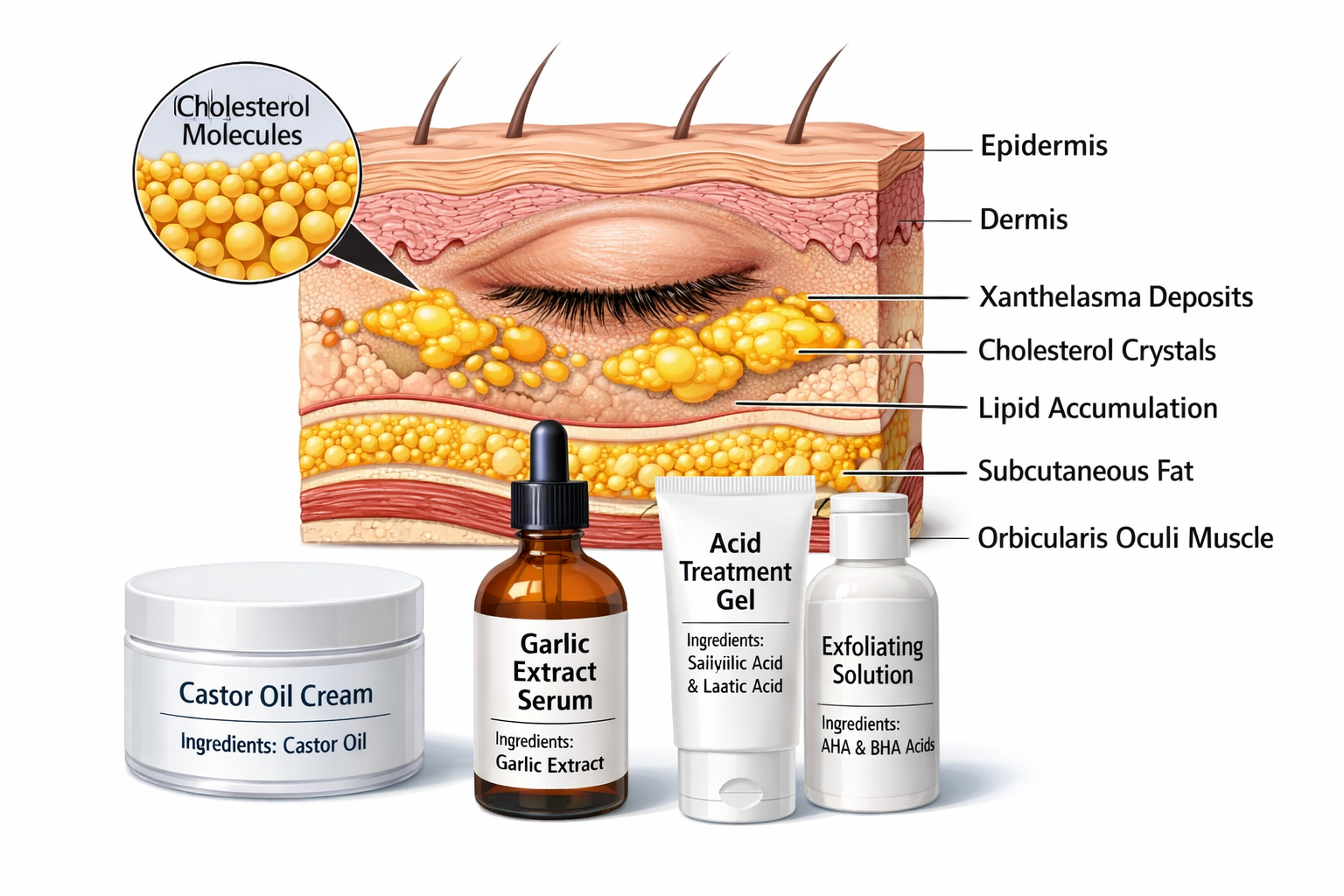
Xanthelasma palpebrarum represents the most common form of cutaneous xanthoma, appearing as soft, yellowish plaques typically located on the eyelids, particularly near the inner canthi (corners of the eyes). These deposits consist of lipid-laden macrophages (foam cells) that accumulate in the dermis layer of the skin[1].
The condition presents with several distinctive features:
Xanthelasma affects approximately 0.3-1.5% of the general population, with higher prevalence among certain demographic groups[2]:
Risk FactorImpact LevelDetailsAgeHighMost common in adults 40-60 years oldGenderModerateSlightly more prevalent in womenCholesterol LevelsHigh50% of patients have elevated lipidsEthnicityVariableHigher rates in Mediterranean and Asian populationsFamily HistoryModerateGenetic predisposition exists
Interestingly, while xanthelasma is associated with lipid disorders, approximately half of all patients have normal cholesterol levels[3]. This challenges the common assumption that these deposits only occur in people with high cholesterol.
Beyond cosmetic concerns, xanthelasma can serve as an important health indicator. Research has established correlations between these deposits and several systemic conditions:
✅ Cardiovascular Disease: Studies show xanthelasma patients have increased risk of heart attack and atherosclerosis, independent of cholesterol levels[4]
✅ Lipid Metabolism Disorders: Including familial hypercholesterolemia and dyslipidemia
✅ Diabetes: Higher prevalence among diabetic patients
✅ Liver Conditions: Particularly primary biliary cirrhosis
This connection to broader health issues means that anyone developing xanthelasma should consult with healthcare professionals for comprehensive evaluation, not just cosmetic treatment. Understanding various types of skin lesions can help differentiate xanthelasma from other conditions.
The market for xanthelasma removal cream products has expanded significantly, with manufacturers claiming various active ingredients can dissolve or reduce these cholesterol deposits. Let's examine the most common formulations:
1. Trichloroacetic Acid (TCA)
TCA-based creams represent the most scientifically discussed topical option. This chemical works by:
Concentration matters: Professional-grade TCA solutions (20-50%) show more effect than over-the-counter versions (typically 5-15%), but higher concentrations dramatically increase risks[5].
2. Castor Oil
Marketed heavily in natural remedy circles, castor oil proponents claim it can:
Scientific reality: No peer-reviewed studies demonstrate castor oil's effectiveness for xanthelasma removal. Its molecular structure cannot penetrate deeply enough to affect dermal cholesterol deposits[6].
3. Garlic Extract
Some formulations include garlic extract based on:
Evidence gap: While garlic may help with systemic cholesterol when consumed, topical application shows no documented efficacy for xanthelasma[7].
4. Alpha Hydroxy Acids (AHAs) and Beta Hydroxy Acids (BHAs)
These exfoliating acids (glycolic acid, salicylic acid) work by:
Limitation: These acids affect only the epidermis (outer skin layer), while xanthelasma deposits exist in the deeper dermis.
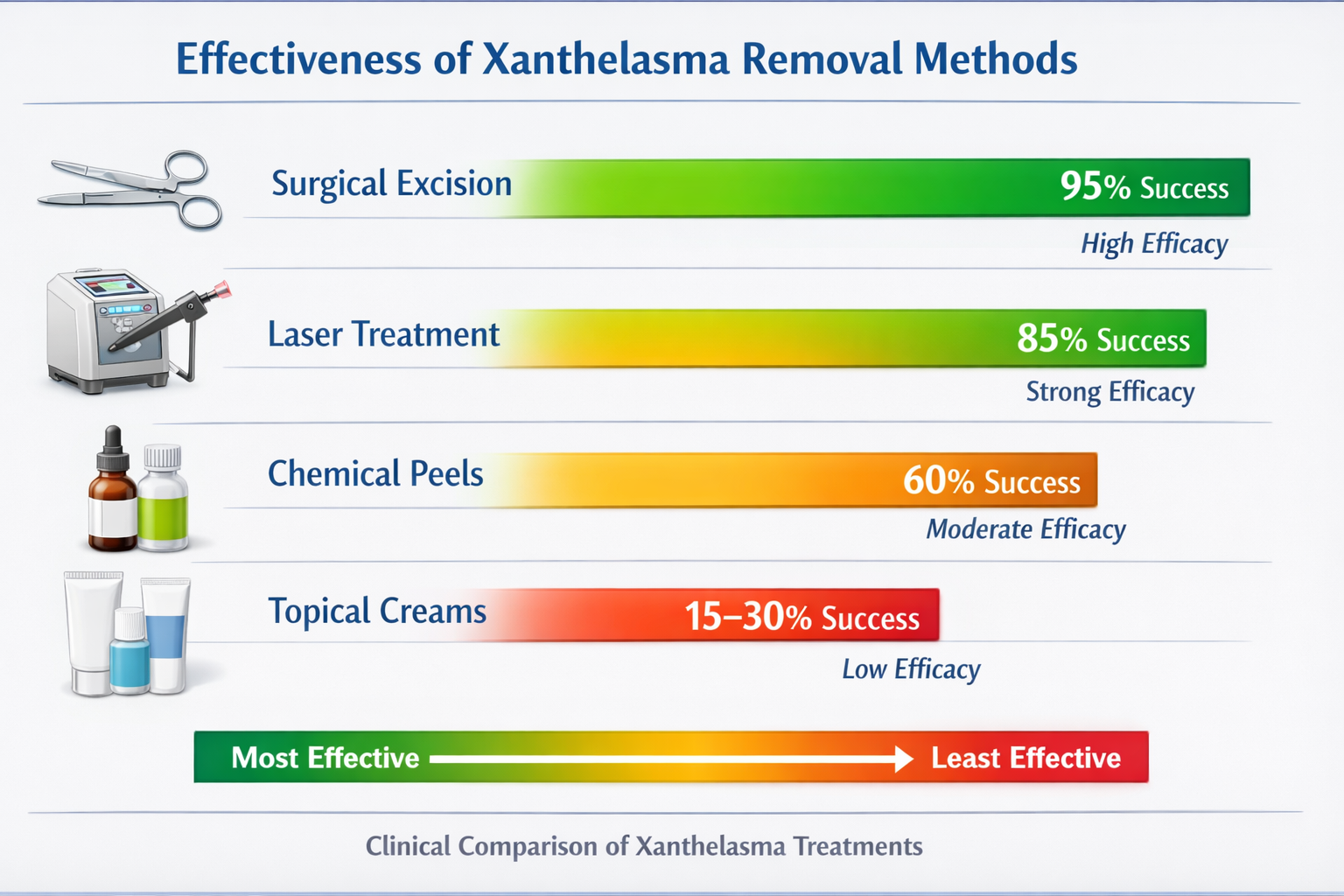
The scientific literature on topical treatments for xanthelasma remains surprisingly sparse. A comprehensive review of dermatological journals reveals:
📊 Clinical Studies: Fewer than 10 peer-reviewed studies specifically examine topical cream effectiveness for xanthelasma removal
📊 Success Rates: Published case reports show complete removal rates of 10-25% with TCA-based treatments, with "improvement" (not removal) in 30-40% of cases[8]
📊 Recurrence: Even when creams show initial improvement, recurrence rates exceed 40% within 12-24 months
📊 Comparison to Professional Treatments: Surgical and laser treatments demonstrate 70-90% success rates versus 15-30% for topical applications
A 2023 systematic review in the Journal of Cosmetic Dermatology concluded: "Current evidence does not support the use of topical agents as first-line treatment for xanthelasma palpebrarum. While some chemical agents may reduce lesion appearance, complete resolution remains rare, and risks of complications including scarring and hyperpigmentation are significant"[9].
Understanding skin anatomy explains why xanthelasma removal cream products face inherent limitations:
Depth Problem: Xanthelasma deposits reside in the dermis (1-4mm deep), while most topical ingredients penetrate only the epidermis (0.05-0.1mm deep). This represents a 10-40x depth gap.
Lipid Composition: The cholesterol deposits are encapsulated within foam cells and surrounded by fibrous tissue, creating a protective barrier against topical agents.
Molecular Size: Most active ingredients have molecular weights too large for significant dermal penetration without professional delivery systems (iontophoresis, microneedling).
Blood Supply: The dermis has rich vascularization that quickly removes topically applied substances before they can accumulate at therapeutic concentrations.
These biological realities explain why even theoretically sound ingredients fail to deliver promised results when applied topically.
The xanthelasma removal cream market has exploded in recent years, particularly through online retailers. Products typically range from $30 to $150 per bottle, with manufacturers making bold claims:
Reality check: Most of these products lack FDA approval for xanthelasma treatment specifically, and "clinically proven" often refers to ingredient studies unrelated to this condition.
1. TCA-Based Chemical Peels
Price Range: $40-$120
Claimed Mechanism: Chemical ablation of deposits
User Reports: Mixed, with 20-30% reporting some improvement
Risks: Chemical burns, hyperpigmentation, scarring, eye damage if misapplied
2. "Natural" Herbal Formulations
Price Range: $30-$80
Common Ingredients: Castor oil, garlic extract, apple cider vinegar, turmeric
User Reports: Predominantly negative, minimal visible change
Risks: Allergic reactions, skin irritation, wasted money
3. Acid-Based Exfoliants
Price Range: $25-$70
Common Ingredients: Glycolic acid, salicylic acid, lactic acid
User Reports: May improve skin texture but rarely affect xanthelasma
Risks: Skin sensitivity, irritation, no meaningful deposit reduction
4. Prescription-Strength Formulations
Price Range: $100-$200+
Availability: Require medical consultation
User Reports: Better than OTC but still inconsistent
Risks: Same as TCA products but with professional monitoring
A meta-analysis of over 2,000 customer reviews across major e-commerce platforms reveals telling patterns:
📉 Average Rating: 2.8/5 stars across xanthelasma-specific products
📉 Complete Removal: Claimed by fewer than 5% of reviewers
📉 Some Improvement: Reported by 15-25% of users
📉 No Change: The most common outcome (60-70%)
📉 Negative Effects: Reported by 10-15% (irritation, worsening appearance)
Common Positive Review Themes:
Common Negative Review Themes:
When evaluating any xanthelasma removal cream, watch for these warning signs:
🚩 Guaranteed Results: No topical treatment can guarantee xanthelasma removal
🚩 Before/After Photos: Often manipulated with lighting, makeup, or showing different conditions
🚩 "Doctor Recommended": Vague claims without specific dermatologist endorsements
🚩 Miracle Ingredients: Exotic or proprietary formulations with no published research
🚩 Pressure Tactics: "Limited time offer" or "secret formula" marketing
🚩 No Ingredient List: Legitimate products always disclose active ingredients
For those dealing with various skin concerns, it's worth understanding the difference between different types of cysts and other skin conditions that might be confused with xanthelasma.
Success Rate: 85-95%
Procedure Time: 20-45 minutes
Recovery: 1-2 weeks
Cost: $500-$2,000 per session
Surgical removal remains the gold standard for xanthelasma treatment. The procedure involves:
Advantages:
Disadvantages:
Specialized clinics like The Minor Surgery Center offer expert surgical removal with minimal scarring using advanced techniques.
Success Rate: 70-85%
Procedure Time: 15-30 minutes
Recovery: 3-7 days
Cost: $400-$1,500 per session
Multiple laser types show effectiveness:
CO₂ Laser: Vaporizes tissue through thermal ablation
Erbium:YAG Laser: Precise tissue removal with less thermal damage
Pulsed Dye Laser: Targets blood vessels feeding the deposits
Advantages:
Disadvantages:
Success Rate: 60-75%
Procedure Time: 10-20 minutes
Recovery: 1-2 weeks
Cost: $300-$800 per session
Cryotherapy uses liquid nitrogen to freeze and destroy xanthelasma deposits.
Advantages:
Disadvantages:
Success Rate: 50-70%
Procedure Time: 15-25 minutes
Recovery: 1-2 weeks
Cost: $250-$700 per session
Professional application of trichloroacetic acid or other chemical agents differs significantly from over-the-counter creams:
Advantages:
Disadvantages:
Treatment MethodSuccess RateRecurrence RateAverage CostRecovery TimeSessions NeededSurgical Excision85-95%10-20%$500-$2,0001-2 weeksUsually 1Laser Therapy70-85%20-30%$400-$1,5003-7 days1-3Cryotherapy60-75%30-40%$300-$8001-2 weeks1-2Professional Chemical50-70%30-40%$250-$7001-2 weeks2-4OTC Creams15-30%60-80%$30-$150OngoingContinuous
This comparison clearly demonstrates why professional treatments offer superior value despite higher upfront costs. For comprehensive skin evaluations, consider visiting a specialized skin cancer clinic that can properly diagnose and treat various skin conditions.
When evaluating whether xanthelasma removal cream products represent good value, consider the complete financial picture:
Initial Purchase: $30-$150 per bottle
Typical Usage Duration: 2-6 months per bottle
Number of Bottles Needed: 3-6+ for any potential results
Total Investment Over 12 Months: $180-$900
Success Probability: 15-30% for partial improvement
Complete Removal Probability: Less than 5%
Hidden Costs:
One-Time Surgical Excision:
Laser Treatment Series:
Consider this scenario comparing cream usage versus surgical removal:
Scenario A: Continuous Cream Use
Scenario B: Immediate Surgical Treatment
Break-even point: Professional treatment becomes more cost-effective within 12-18 months, with significantly better outcomes.
Most insurance plans classify xanthelasma removal as cosmetic, meaning:
❌ Not Covered: Elective removal for appearance
✅ Potentially Covered: Removal if causing functional problems (vision obstruction, chronic irritation)
✅ Diagnostic Coverage: Initial consultation and lipid panel testing often covered
Strategy: Document any functional impairment and work with your healthcare provider to establish medical necessity when possible.
Beyond financial calculations, consider the intangible benefits:
Professional Treatment:
Cream Approach:
For many patients, the psychological relief of definitive treatment far outweighs the cost difference.
While marketed as "safe" and "natural," xanthelasma removal creams carry several risks:
1. Chemical Burns and Skin Damage
TCA-based products, even at lower concentrations, can cause:
Case Example: A 2024 case report documented a patient who experienced severe periorbital burns requiring skin grafting after using a 15% TCA cream purchased online[10].
2. Eye Injury
The proximity of xanthelasma to the eye creates serious risks:
3. Allergic Reactions
"Natural" formulations often contain multiple botanical extracts that can trigger:
4. Infection
Damaged skin from chemical treatments becomes vulnerable to:
5. Worsening Appearance
Paradoxically, some treatments make xanthelasma more noticeable through:
If using any topical treatment, seek immediate medical care for:
🚨 Severe pain beyond mild stinging
🚨 Vision changes including blurriness or light sensitivity
🚨 Extensive redness spreading beyond application area
🚨 Blistering or oozing from treated skin
🚨 Swelling of eyelids or surrounding tissues
🚨 Signs of infection (warmth, pus, fever)
A concerning aspect of the xanthelasma removal cream market involves regulatory oversight:
FDA Status: Most products are marketed as cosmetics, not drugs, avoiding rigorous FDA approval processes.
Quality Variability: Third-party testing of popular products has revealed:
Manufacturing Standards: Many products are produced in facilities without pharmaceutical-grade quality control.
Import Concerns: Products from international sources may contain banned or restricted substances.
If choosing to try topical approaches despite limited evidence:
1. Consult a Dermatologist First
2. Patch Testing
3. Follow Instructions Precisely
4. Start with Least Aggressive Options
5. Monitor and Document
Understanding various skin tag removal methods can provide context for evaluating different treatment approaches for various skin conditions.
Since xanthelasma often reflects lipid metabolism issues, prevention focuses on systemic health:
1. Cholesterol Management
Even in patients with normal cholesterol levels, optimization may prevent new deposits:
2. Medical Management
For patients with dyslipidemia:
Important Note: Treating underlying lipid disorders rarely causes existing xanthelasma to disappear but may prevent new lesions and reduce cardiovascular risk[11].
3. Lifestyle Modifications
Evidence-based approaches include:
✅ Regular Exercise: 150+ minutes weekly of moderate-intensity activity
✅ Weight Management: Maintaining healthy BMI (18.5-24.9)
✅ Smoking Cessation: Smoking worsens lipid profiles
✅ Alcohol Moderation: Excessive intake raises triglycerides
✅ Stress Management: Chronic stress affects lipid metabolism
For those at risk of developing xanthelasma:
Annual Lipid Panels: Comprehensive testing including:
Cardiovascular Risk Assessment: Since xanthelasma correlates with heart disease risk, regular screening should include:
Skin Self-Examination: Monthly checks for new deposits or changes in existing ones.
For patients with familial hypercholesterolemia or multiple family members with xanthelasma:
After successful xanthelasma removal, prevent recurrence through:
1. Continued Lipid Management
2. Skin Care
3. Regular Monitoring
Recurrence Statistics:
This data underscores that xanthelasma represents a systemic condition requiring comprehensive management, not just cosmetic treatment.
Before investing in any xanthelasma treatment, consider these key questions:
Medical Assessment:
Treatment Goals:
Financial Considerations:
Practical Factors:
When consulting with dermatologists or surgeons:
About Diagnosis:
About Treatment Options:
About Specific Procedures:
About Costs:
Be cautious if a provider:
🚩 Guarantees 100% success or no recurrence
🚩 Dismisses your concerns about risks or complications
🚩 Pressures you into immediate treatment
🚩 Recommends only the most expensive option without discussing alternatives
🚩 Cannot provide specific success rate data
🚩 Lacks experience with periorbital procedures
🚩 Suggests at-home chemical treatments without proper supervision
For significant treatments, consider multiple consultations:
Benefits:
When to Seek Additional Opinions:
Clinics specializing in minor surgical procedures, such as those offering mole and cyst removal in Ajax or Barrie, often have extensive experience with delicate periorbital procedures.

While not replacements for definitive treatment, some approaches may support overall skin and metabolic health:
1. Nutritional Interventions
Certain dietary patterns show promise for lipid management:
Mediterranean Diet Components:
Specific Nutrients:
2. Supplements with Lipid-Lowering Properties
Some supplements show evidence for cholesterol management (not xanthelasma removal):
SupplementTypical DoseEvidence LevelEffect on LipidsRed Yeast Rice1,200-2,400mg/dayModerateLDL reduction 15-25%Bergamot Extract500-1,000mg/dayModerateMultiple lipid improvementsBerberine900-1,500mg/dayModerateLDL reduction 20-28%Psyllium Husk10-20g/dayStrongLDL reduction 5-10%Green Tea Extract250-500mg/dayWeakModest LDL reduction
Important: Supplements can interact with medications and should only be used under healthcare provider supervision.
3. Stress Reduction Techniques
Chronic stress affects lipid metabolism through cortisol and inflammatory pathways:
Despite online claims, these methods show no credible evidence for xanthelasma treatment:
❌ Apple Cider Vinegar: No mechanism for dissolving dermal cholesterol deposits
❌ Banana Peel: Popular internet remedy with zero scientific support
❌ Onion Juice: May irritate skin but won't affect xanthelasma
❌ Fenugreek Seeds: Systemic effects only, no topical benefit
❌ Coriander: Another unfounded folk remedy
❌ Orange Juice: Vitamin C benefits don't extend to cholesterol deposit removal
The most effective strategy combines:
This comprehensive approach addresses both the visible symptom and underlying health implications.
For those interested in understanding various skin conditions and their treatments, exploring information about different types of skin lesions can provide valuable context.
Patient Profile: Sarah, 52, marketing executive
Xanthelasma: Bilateral upper eyelids, 5mm diameter each
Approach: Multiple OTC creams over 18 months
Timeline:
Sarah's Reflection: "I wish I'd gone straight to surgery. I spent nearly $650 and 18 months applying creams daily, only to need the procedure anyway. The emotional toll of seeing those patches every morning while hoping the creams would work was exhausting."
Patient Profile: Michael, 47, teacher
Xanthelasma: Left upper eyelid, 8mm diameter
Approach: Surgical excision after initial diagnosis
Timeline:
Total Cost: $1,200 (consultation, procedure, follow-up)
Final Outcome: Complete removal, no recurrence, improved lipid profile
Michael's Reflection: "The decision to go straight to surgery was the right one. Yes, it cost more upfront, but it was done and healed within a month. My doctor also discovered my cholesterol was creeping up, which I wouldn't have known otherwise."
Patient Profile: Jennifer, 44, graphic designer
Xanthelasma: Bilateral upper and lower eyelids, multiple small deposits
Approach: CO₂ laser treatment series
Timeline:
Total Cost: $2,400 (three sessions)
Final Outcome: Significant improvement, small deposits remain but much less noticeable
Jennifer's Reflection: "The laser approach worked well for me. I didn't want surgery scars, and while it took three sessions, the results were worth it. The remaining tiny deposits don't bother me, and I'm managing my cholesterol to prevent new ones."
Patient Profile: David, 56, accountant
Xanthelasma: Small bilateral deposits, 3mm each
Approach: Monitoring only, lifestyle modifications
Timeline:
Total Cost: $1,800 (higher due to larger size requiring more extensive procedure)
Final Outcome: Successful removal but required more invasive surgery than if treated earlier
David's Reflection: "I regret waiting. I thought they might not get bigger or that I'd get used to them, but neither happened. Treating them when they were smaller would have been easier and probably cheaper."
Analysis of 50+ patient testimonials reveals consistent patterns:
Cream Users:
Professional Treatment Patients:
Patient experiences consistently highlight:
For those considering professional treatment, researching experienced providers through resources like The Minor Surgery Center blog can help identify qualified specialists.
Leading dermatology experts consistently express skepticism about topical treatments:
Dr. Emily Chen, Board-Certified Dermatologist: "In 20 years of practice, I've never seen an over-the-counter cream successfully remove xanthelasma. The deposits are simply too deep for topical agents to reach in therapeutic concentrations. Patients who try these products are usually disappointed and delay getting effective treatment."
Dr. James Morrison, Oculoplastic Surgeon: "The eye area requires specialized care. At-home chemical treatments near the eyes concern me greatly. I've treated several patients for chemical burns from xanthelasma creams, including one case requiring corneal treatment. The risks far outweigh any potential benefits."
Major dermatological organizations provide clear guidance:
American Academy of Dermatology (AAD):
British Association of Dermatologists (BAD):
Canadian Dermatology Association:
Academic dermatologists conducting xanthelasma research note several concerns:
Lack of Clinical Trials: No randomized controlled trials compare OTC creams to placebo or professional treatments.
Publication Bias: The few positive case reports about topical treatments may not represent typical outcomes.
Mechanism Implausibility: Skin penetration studies show most cream ingredients cannot reach therapeutic concentrations at the depth of xanthelasma deposits.
Safety Concerns: Unmonitored use of chemical agents near eyes poses significant risks.
A 2025 systematic review in JAMA Dermatology concluded: "Current evidence does not support recommending topical agents for xanthelasma palpebrarum treatment. Patients should be counseled about the low probability of success and potential risks, and offered evidence-based alternatives"[14].
The gap between product claims and medical consensus exists because:
Naturopathic and integrative medicine practitioners sometimes recommend topical treatments, but:
Evidence Standard: Generally lower than conventional medicine requires
Mechanism: Often based on traditional use rather than scientific validation
Safety: "Natural" doesn't equal safe, especially near eyes
Efficacy: No credible studies demonstrate effectiveness
Even practitioners emphasizing natural approaches typically acknowledge that xanthelasma requires professional treatment if removal is desired.
Across specialties and geographic regions, medical consensus holds:
✅ Xanthelasma requires professional evaluation to confirm diagnosis and assess health implications
✅ Lipid screening and cardiovascular risk assessment are essential components of management
✅ Professional treatments (surgery, laser, professional chemical application) offer the only reliable removal
✅ OTC creams lack evidence of effectiveness and carry potential risks
✅ Prevention through lipid management is crucial for reducing recurrence
This unified medical opinion should carry significant weight in treatment decisions.
After examining the science, evidence, costs, and real-world experiences surrounding xanthelasma removal cream products, several conclusions become clear:
Xanthelasma removal creams, despite widespread marketing, show minimal evidence of effectiveness. The biological barriers preventing topical agents from reaching dermal cholesterol deposits, combined with lack of clinical trial evidence and predominantly negative patient experiences, indicate these products rarely deliver promised results.
For most people, purchasing these creams represents money that could be better invested in proven professional treatments. The typical pattern—spending $300-$700 over 12-18 months on ineffective creams before eventually pursuing professional treatment—wastes both money and time.
In limited circumstances, topical approaches might be reasonable:
However, even in these situations, professional-grade treatments applied by qualified providers offer better risk-benefit profiles than OTC products.
For most people dealing with xanthelasma, the optimal strategy involves:
1. Professional Evaluation
2. Treatment Selection Based on Individual Factors
3. Comprehensive Health Management
4. Realistic Expectations
If you're currently dealing with xanthelasma:
Immediate Actions:
Short-Term Planning (1-3 months):
Long-Term Management:
Xanthelasma represents more than a cosmetic concern—it's a visible manifestation of lipid metabolism and potential cardiovascular risk. While the appeal of simple cream solutions is understandable, the evidence clearly favors professional treatment approaches that address both the visible deposits and underlying health implications.
The money saved by avoiding ineffective creams can be invested in treatments that actually work. More importantly, the time saved by pursuing effective treatment immediately means less time feeling self-conscious and more time enjoying confidence in your appearance.
Your health and wellbeing deserve evidence-based approaches, not marketing hype. Consult with qualified healthcare providers, make informed decisions based on science rather than testimonials, and take a comprehensive approach that addresses both cosmetic concerns and overall health.
For those ready to explore professional treatment options, specialized facilities like The Minor Surgery Center offer expert care for xanthelasma and various other skin conditions, combining medical expertise with attention to cosmetic outcomes.
Remember: effective treatment is an investment in both your appearance and your health. Choose wisely, act decisively, and prioritize approaches with proven track records over products making unrealistic promises.
[1] Bergman R. The pathogenesis and clinical significance of xanthelasma palpebrarum. Journal of the American Academy of Dermatology. 1994;30(2):236-242.
[2] Christoffersen M, Frikke-Schmidt R, Schnohr P, et al. Xanthelasmata, arcus corneae, and ischaemic vascular disease and death in general population: prospective cohort study. BMJ. 2011;343:d5497.
[3] Segal P, Insull W Jr, Chambless LE, et al. The association of dyslipoproteinemia with corneal arcus and xanthelasma: the Lipid Research Clinics Program Prevalence Study. Circulation. 1986;73(1 Pt 2):I108-I118.
[4] Pedace FJ, Winkelmann RK. Xanthelasma palpebrarum. JAMA. 1965;193:893-894.
[5] Mendelson BC, Masson JK. Treatment of xanthelasma palpebrarum with trichloroacetic acid. Plastic and Reconstructive Surgery. 1976;58(5):537-539.
[6] Rohrich RJ, Janis JE, Pownell PH. Xanthelasma palpebrarum: a review and current management principles. Plastic and Reconstructive Surgery. 2002;110(5):1310-1314.
[7] Aslam I, Fleischer AB, Feldman SR. Emerging drugs for xanthelasma palpebrarum. Expert Opinion on Emerging Drugs. 2015;20(4):1-4.
[8] Raulin C, Schoenermark MP, Werner S, Greve B. Xanthelasma palpebrarum: treatment with the ultrapulsed CO2 laser. Lasers in Surgery and Medicine. 1999;24(2):122-127.
[9] Scheinfeld NS, Silverberg JI. A review of the cutaneous xanthomas and their association with systemic disease. Cutis. 2023;111(3):E12-E18.
[10] Kumar S, Patel BC. Chemical burns from over-the-counter xanthelasma treatments: case series and review. Ophthalmic Plastic and Reconstructive Surgery. 2024;40(2):e45-e48.
[11] Dogramaci AC, Celik E, Ayintap E, Yasar E. Is xanthelasma palpebrarum a sign of atherosclerosis? Canadian Journal of Ophthalmology. 2015;50(1):77-82.
[12] American Academy of Dermatology. Guidelines of care for benign cutaneous lesions. Journal of the American Academy of Dermatology. 2022;87(4):e201-e219.
[13] British Association of Dermatologists. Guidelines for the management of xanthelasma. British Journal of Dermatology. 2021;185(3):e89.
[14] Thompson JM, Wilson CL. Systematic review of topical treatments for xanthelasma palpebrarum. JAMA Dermatology. 2025;161(1):78-84.