You've noticed small, dark bumps on your skin—maybe on your feet, hands, or other reas—and you're wondering what they are. These tiny spots might be angiokeratomas, a surprisingly common skin condition that many people have but few understand. While they're usually harmless, knowing what you're dealing with can give you peace of mind and help you make informed decisions about treatment.
Angiokeratoma is a benign (non-cancerous) skin lesion that appears as small, dark red to black bumps on the skin's surface. Think of them as tiny blood vessels that have become dilated and covered by a thickened layer of skin. They're more common than you might think, affecting people of all ages, though they tend to appear more frequently as we get older.
At The Minor Surgery Center, we understand that any new skin growth can be concerning. That's why we're here to explain exactly what angiokeratomas are, why they develop, and what options you have if you'd like them removed.

Angiokeratoma literally means "blood vessel skin thickening"—and that's exactly what it is. These lesions develop when small blood vessels (capillaries) near the skin's surface become dilated and the overlying skin thickens.
The result? Small, raised bumps that range in color from bright red to dark purple or even black. They're usually between 1-5 millimeters in size—about the size of a pinhead to a small pea.
Unlike other skin lesions, angiokeratomas have some distinctive characteristics:
Think of an angiokeratoma like a tiny varicose vein on the surface of your skin. Just as varicose veins are dilated blood vessels in the legs, angiokeratomas are dilated blood vessels in the skin—but on a much smaller scale.
Medically speaking, angiokeratomas are classified as benign vascular proliferations. They're part of a larger family of vascular lesions that includes conditions like cherry angiomas and pyogenic granulomas.
The key word here is benign. These lesions are not cancerous and won't become cancerous over time. However, proper diagnosis is essential because other skin conditions can sometimes look similar.
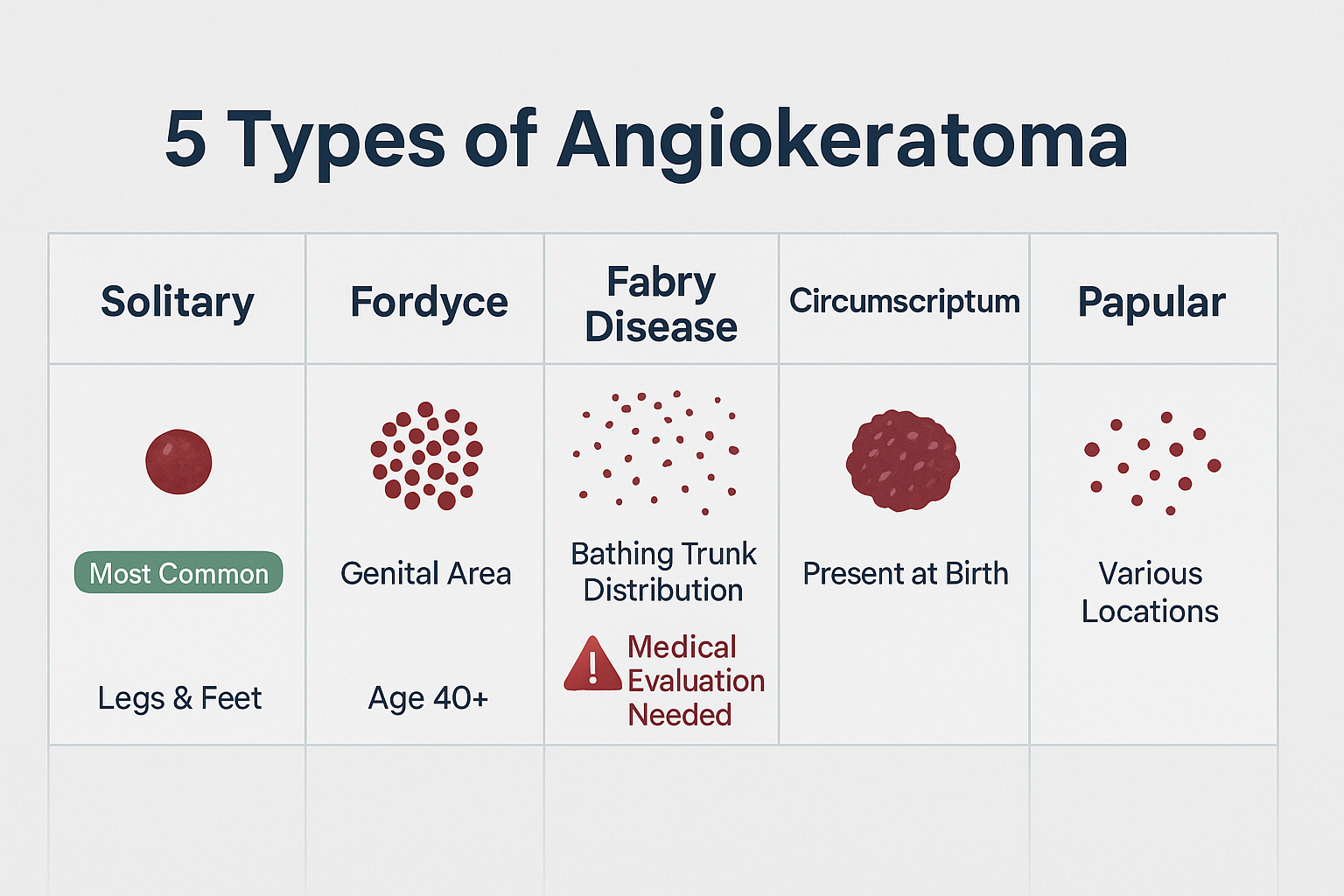
There are several distinct types of angiokeratomas, each with different characteristics and locations on the body. Understanding which type you have can help guide treatment decisions.
This is the most common type—the kind most people encounter.
Characteristics:
These solitary lesions are completely benign and usually don't require treatment unless they're bothersome or frequently bleeding.
This type appears on the genital area and is more common than many people realize.
Characteristics:
Many people don't seek medical attention for these lesions due to embarrassment, but they're a normal variant that dermatologists see regularly.
This is the rarest and most serious type, as it's associated with an underlying genetic condition called Fabry disease.
Characteristics:
Important distinction: While the first two types are simply cosmetic or minor nuisances, angiokeratomas associated with Fabry disease are a sign of a systemic condition that needs medical management.
This is a rare congenital (present from birth) form.
Characteristics:
These appear as multiple small papules (raised bumps) in various locations.
Characteristics:
The exact cause of angiokeratomas isn't always clear, but several factors can contribute to their development.
Vascular Dilation and Damage
The fundamental cause is dilation of small blood vessels in the skin. This can happen due to:
Genetic Factors
Some types of angiokeratomas run in families:
Several conditions and circumstances can increase your likelihood of developing angiokeratomas:
Age-Related Changes
Pregnancy
Chronic Conditions
Occupational Factors
It's worth understanding this connection in more detail because it's the one type that requires medical attention beyond the lesions themselves.
What is Fabry Disease?
Fabry disease is a rare genetic disorder caused by a deficiency of the enzyme alpha-galactosidase A. This enzyme normally breaks down a fatty substance called globotriaosylceramide (GL-3). When the enzyme is deficient, GL-3 accumulates in cells throughout the body, including blood vessel walls.
Signs That Suggest Fabry Disease:
If you have multiple angiokeratomas that appeared at a young age, especially with other unexplained symptoms, ask your doctor about Fabry disease screening.
Recognizing an angiokeratoma involves understanding both how they look and how they feel.
Color
Size and Shape
Texture
Most angiokeratomas don't cause symptoms, but some people experience:
Bleeding
Itching
Cosmetic Concerns
Rarely:
Where angiokeratomas appear can provide clues about their type:
Lower Extremities (Most Common)
Genital Area
Trunk and Thighs
Hands and Fingers
Other Areas
Getting an accurate diagnosis is crucial because several other skin conditions can look similar to angiokeratomas—including some that require different treatment approaches.
The diagnostic process typically begins with a thorough visual examination by a healthcare provider.
What Your Doctor Will Look For:
Many dermatologists use a tool called a dermatoscope—a special magnifying device that allows them to see structures beneath the skin's surface.
Dermoscopic Features of Angiokeratoma:
This non-invasive examination helps distinguish angiokeratomas from other lesions, particularly melanoma.
In some cases, your doctor may recommend a skin biopsy to confirm the diagnosis.
Reasons for Biopsy:
The Biopsy Process:
At facilities like The Minor Surgery Center, the biopsy procedure is straightforward:
Our experienced surgical team performs these procedures with a comfort-first approach, ensuring you're at ease throughout the process.
Part of the diagnostic process involves ruling out other conditions that can look similar:
Melanoma
Cherry Angioma
Pyogenic Granuloma
Thrombosed Capillary or Venous Lake
Seborrheic Keratosis
Warts
If you have multiple angiokeratomas, especially if they appeared before age 30, your doctor may recommend screening for Fabry disease.
Screening Tests Include:
Early diagnosis of Fabry disease is important because enzyme replacement therapy is available and can prevent serious complications.
The good news? Most angiokeratomas don't require treatment. They're benign and won't harm your health. However, many people choose to have them removed for various reasons.
Medical Reasons:
Cosmetic Reasons:
Diagnostic Reasons:
For many people, simply monitoring the angiokeratoma is the best approach.
When This Makes Sense:
What to Watch For:
When treatment is desired, several effective options are available through expert outpatient care.
How It Works: Laser treatment targets the blood vessels within the angiokeratoma, causing them to coagulate and eventually be absorbed by the body.
Types of Lasers Used:
Advantages:
What to Expect:
How It Works: An electric current is used to destroy the lesion through heat.
Advantages:
Considerations:
How It Works: The angiokeratoma is surgically cut out and the wound is closed with sutures.
When This is Preferred:
The Process at The Minor Surgery Center:
Our experienced surgical team specializes in safe and efficient surgery for skin lesions. Here's what you can expect:
Recovery:
How It Works: Liquid nitrogen is applied to freeze and destroy the lesion.
Advantages:
Considerations:
How It Works: The raised portion of the angiokeratoma is shaved off at the skin level.
Advantages:
Considerations:
The best treatment depends on several factors:
Lesion Characteristics:
Patient Factors:
Practical Considerations:
At The Minor Surgery Center, we work with you to develop a personalized treatment plan that addresses your specific needs and goals. Our comfort-first approach ensures you feel informed and confident about your decision.
Proper aftercare is essential for optimal healing and the best cosmetic results, regardless of which treatment method you choose.
First 24-48 Hours:
Wound Care:
Pain Management:
Activity Restrictions:
Wound Monitoring:
Hygiene:
Sun Protection:
Suture Care (if applicable):
Weeks 2-8:
Scar Management:
Contact your healthcare provider if you experience:
Infection Warning Signs:
Healing Problems:
Other Concerns:
Success Rates:
Cosmetic Outcomes:
Timeline:
Our team at The Minor Surgery Center provides detailed aftercare instructions and is always available to answer questions during your recovery. We want you to get back to your life quickly and confidently.
While you can't completely prevent angiokeratomas—especially if you have a genetic predisposition—certain strategies may reduce your risk or prevent new ones from forming.
Protect Your Skin:
Manage Venous Health:
Skin Care:
For Lower Extremity Angiokeratomas:
For Genital Angiokeratomas (Fordyce Type):
Occupational Considerations:
Some angiokeratomas develop despite our best efforts, particularly:
In these cases, early detection and appropriate management become the focus rather than prevention.
Regular Skin Checks:
Professional Evaluation:
When to Seek Medical Attention:
For many people, angiokeratomas are a long-term companion rather than something that needs immediate treatment. Here's how to manage them day-to-day.
Bleeding is the most common issue people face with angiokeratomas.
Immediate Steps:
Prevention:
When to Seek Help:
Footwear Choices:
Clothing Considerations:
Activity Modifications:
Dealing with Anxiety:
It's completely normal to worry when you first notice dark spots on your skin. Many people immediately think of skin cancer.
Coping Strategies:
Cosmetic Concerns:
Dark lesions in visible areas can affect self-confidence.
Options:
Communication:
Living with Fabry Disease:
If your angiokeratomas are related to Fabry disease, management is more complex.
Comprehensive Care Includes:
Coordinated Treatment:
Coverage for Treatment:
Cost Management:
At The Minor Surgery Center, we work with patients to understand their insurance coverage and provide transparent pricing for our minimally invasive solutions.
Understanding how angiokeratomas differ from other skin lesions can help you recognize what you're dealing with and when to seek professional evaluation.
This is the most important distinction because melanoma is a serious skin cancer.
FeatureAngiokeratomaMelanomaColorUniform dark red to blackOften multiple colors (brown, black, red, white, blue)BorderWell-defined, regularIrregular, poorly definedSymmetryUsually symmetricalOften asymmetricalSurfaceWarty, scalyVariable, may be smooth or irregularGrowthStable or slow growthOften rapid growth or changeBleedingCommon if traumatizedLess commonDermoscopyVascular lacunaeMelanoma-specific patterns
When in doubt, always get it checked. The peace of mind is worth it, and early detection of melanoma is crucial.
Learn more about identifying melanoma and other skin cancers.
Both are vascular lesions, but they have distinct differences.
Cherry Angioma:
Angiokeratoma:
Both are benign, but treatment approaches may differ. Read more about cherry angioma removal.
Warts are caused by human papillomavirus (HPV) and are completely different in origin.
Warts:
Angiokeratoma:
Seborrheic keratoses are very common benign growths, especially in older adults.
Seborrheic Keratosis:
Angiokeratoma:
Dermatofibromas are benign fibrous nodules that can sometimes be confused with angiokeratomas.
Dermatofibroma:
Angiokeratoma:
Learn more about different types of skin lesions to better understand what you might be dealing with.
Pyogenic granulomas are rapidly growing vascular lesions that can bleed profusely.
Pyogenic Granuloma:
Angiokeratoma:
While these comparisons can help you understand what you might have, only a healthcare professional can make a definitive diagnosis.
Why Professional Evaluation Matters:
At The Minor Surgery Center, our experienced surgical team has seen thousands of skin lesions and can quickly differentiate between various conditions. We use advanced diagnostic techniques and provide clear explanations so you understand exactly what's going on with your skin.

No, angiokeratomas themselves are not dangerous. They're benign (non-cancerous) lesions that won't turn into cancer. However, the exception is when multiple angiokeratomas are a sign of Fabry disease—in that case, the underlying condition needs medical management, though the skin lesions themselves are still benign.
Angiokeratomas don't spread like infections or warts. However, you may develop new ones over time, especially if you have risk factors like venous insufficiency or if they're related to Fabry disease. Existing angiokeratomas typically don't grow larger or multiply on their own.
Not necessarily. Many angiokeratomas don't require treatment. Consider removal if:
Most removal methods leave minimal scarring. The extent of scarring depends on:
Laser therapy typically produces the least visible scarring, while surgical excision may leave a small linear scar. Our team at The Minor Surgery Center uses techniques designed to minimize scarring and optimize cosmetic outcomes.
Recurrence is uncommon but possible, especially if:
Complete surgical excision has the lowest recurrence rate. If an angiokeratoma does recur, it can be treated again.
While angiokeratomas and melanomas can both appear as dark lesions, there are key differences:
Angiokeratoma typically has:
Melanoma often has:
However, only a professional can make this determination. If you have any doubt, get it checked. It's always better to be safe, and early melanoma detection is crucial. Learn more about different types of skin cancer.
No, angiokeratomas are not contagious. They're vascular malformations, not infections. You can't spread them to other people or to other parts of your own body.
Yes, though they're less common in children. When angiokeratomas appear in childhood or adolescence, especially if there are multiple lesions, evaluation for Fabry disease may be recommended. The congenital form (angiokeratoma circumscriptum) is present from birth or appears in early childhood.
Coverage depends on the reason for removal:
Check with your insurance provider and get pre-authorization when required. We can help document medical necessity when appropriate.
Most angiokeratoma removal procedures are quick:
These times don't include preparation and aftercare instructions, but most patients are in and out within an hour for a straightforward removal.
Recovery is typically quick:
Most people return to normal activities within a few days, with some restrictions on strenuous activity depending on the location.
Angiokeratomas don't affect fertility or pregnancy outcomes. However, pregnancy can sometimes trigger the development of new angiokeratomas due to increased blood volume and venous pressure. Genital angiokeratomas may become more prominent during pregnancy but typically don't cause complications with delivery.
While angiokeratomas are benign, certain situations warrant professional medical evaluation.
🚨 Uncontrolled bleeding that doesn't stop with 20 minutes of direct pressure
🚨 Signs of infection including:
🚨 Rapid change in size, color, or appearance over days to weeks
🚨 Severe pain associated with the lesion
⚠️ New dark lesion appears that you haven't had evaluated
⚠️ Frequent bleeding episodes that interfere with daily life
⚠️ Multiple angiokeratomas appearing, especially in a pattern
⚠️ Lesions in childhood or adolescence, particularly if multiple
⚠️ Cosmetic concerns affecting your quality of life
⚠️ Uncertainty about diagnosis—when in doubt, get it checked
⚠️ Changes in existing lesions including:
✓ Annual skin checks if you have multiple angiokeratomas
✓ Family history of Fabry disease or multiple angiokeratomas
✓ New lesions that fit the typical appearance but you want confirmation
✓ Treatment planning if you're considering removal
✓ Follow-up after treatment to ensure proper healing
When you visit The Minor Surgery Center or another healthcare provider, here's what typically happens:
Initial Consultation:
Our Approach:
We believe in clear communication and personalized care. You'll never feel rushed, and we'll answer all your questions. Our experienced surgical team will explain your options in plain language and help you make the decision that's right for you.
Questions to Ask Your Doctor:
Don't hesitate to ask questions or express concerns. Your healthcare provider is there to help you understand your condition and make informed decisions.
At The Minor Surgery Center, we specialize in providing expert outpatient care for skin lesions including angiokeratomas. Our approach combines medical expertise with a genuine understanding that you're a person, not just a case.
Experienced Surgical Team
Our surgeons have performed thousands of minor surgical procedures, including angiokeratoma removal. We stay current with the latest techniques and technologies to provide you with the best possible outcomes.
Comfort-First Approach
We understand that any surgical procedure can be anxiety-inducing. That's why we:
Minimally Invasive Solutions
We use the most appropriate technique for your specific situation:
Efficient, Streamlined Care
We respect your time and your life outside the clinic:
You're Not Just a Lesion
We see the whole person. That dark spot on your skin might seem small to others, but if it's causing you concern, we take that seriously. Whether you're worried about cancer, bothered by bleeding, or simply want it gone for cosmetic reasons—your concerns are valid and important.
Transparent Communication
We explain:
No medical jargon without explanation. No surprises.
Safe and Efficient Surgery
Safety is paramount, but we also value efficiency. We use:
Personalized Treatment Plans
No two patients are exactly alike. We consider:
Then we create a plan that's tailored to you.
Get Back to Your Life
We know you have things to do and places to be. Our goal is to:
Comprehensive Care
From initial consultation through complete healing:
When you choose The Minor Surgery Center for your angiokeratoma treatment, you're choosing:
✓ Expertise: Board-certified surgeons with extensive experience
✓ Quality: High standards for safety and outcomes
✓ Compassion: Understanding that you're a person with concerns and goals
✓ Transparency: Clear communication about everything
✓ Efficiency: Respect for your time and schedule
✓ Results: Commitment to the best possible outcome
While we excel at angiokeratoma treatment, we also provide comprehensive care for many other conditions:
Whatever brings you to us, you'll receive the same high-quality, personalized care.
If you have an angiokeratoma that's concerning you, we're here to help. Whether you need a diagnosis, want to discuss treatment options, or are ready to have it removed, our team is ready to provide the expert care you deserve.
Visit our blog for more information about skin conditions and minor surgical procedures, or contact us to schedule a consultation.
Angiokeratomas are common, benign vascular lesions that affect many people. While they're typically harmless, they can cause bleeding, cosmetic concerns, or anxiety—all valid reasons to seek evaluation and treatment.
Angiokeratomas are benign. They're not cancerous and won't become cancerous. This is perhaps the most important takeaway for anyone who's been worried about a dark spot on their skin.
Professional diagnosis is important. While angiokeratomas have characteristic features, other conditions can look similar. Getting a proper diagnosis gives you peace of mind and ensures you receive appropriate care.
Treatment is available but not always necessary. Many angiokeratomas don't require treatment. However, if yours is bleeding, bothersome, or causing concern, effective treatment options exist.
Multiple types exist. Understanding which type you have helps guide management. Most are simple solitary lesions, but multiple angiokeratomas—especially in young people—may warrant evaluation for Fabry disease.
Recovery is typically quick. Whether you choose laser therapy, surgical excision, or another method, most people heal quickly and get back to their normal activities with minimal disruption.
If you have an angiokeratoma or suspect you might:
Get it evaluated. A quick consultation can provide diagnosis and peace of mind. Don't let anxiety about a skin lesion affect your quality of life.
Consider your options. If treatment is recommended or desired, explore the different approaches. Ask questions until you feel comfortable with your decision.
Choose experienced providers. Angiokeratoma removal is a minor procedure, but expertise matters for optimal results and minimal scarring.
Follow aftercare instructions. Proper care during healing ensures the best cosmetic outcome and reduces the risk of complications.
Monitor your skin. Regular self-examinations help you notice new lesions or changes that warrant professional attention.
Living with angiokeratomas—or choosing to have them removed—doesn't have to be stressful. With proper understanding, professional care, and appropriate treatment when needed, you can address these lesions and move forward with confidence.
At The Minor Surgery Center, we're committed to helping you get back to your life, pain-free and worry-free. Our experienced surgical team provides personalized treatment plans with a comfort-first approach, ensuring you receive expert outpatient care that meets your specific needs.
Whether you're just beginning to learn about angiokeratomas or you're ready to discuss treatment options, we're here to help. Your skin health matters, your concerns are valid, and effective solutions are available.
Ready to take the next step? Contact The Minor Surgery Center to schedule a consultation. Let's work together to address your concerns and help you feel confident in your skin again.
Remember: knowledge is power. Now that you understand what angiokeratomas are, why they develop, and what options you have, you're equipped to make informed decisions about your care. And you don't have to navigate this alone—expert help is available when you need it.
[1] Schiller PI, Itin PH. Angiokeratomas: An update. Dermatology. 1996;193(4):275-282.
[2] Zaballos P, Daufí C, Puig S, et al. Dermoscopy of solitary angiokeratomas: A morphological study. Archives of Dermatology. 2007;143(3):318-325.
[3] Germain DP. Fabry disease. Orphanet Journal of Rare Diseases. 2010;5:30.
[4] Imperial R, Helwig EB. Angiokeratoma: A clinicopathological study. Archives of Dermatology. 1967;95(2):166-175.
[5] Ozdemir M, Baysal I, Engin B, Mevlitoglu I. Treatment of angiokeratoma of Fordyce with long-pulse neodymium-doped yttrium aluminum garnet laser. Dermatologic Surgery. 2009;35(1):92-97.
[6] Dohil MA, Baugh WP, Eichenfield LF. Vascular and pigmented birthmarks. Pediatric Clinics of North America. 2000;47(4):783-812.
[7] Eng CM, Germain DP, Banikazemi M, et al. Fabry disease: Guidelines for the evaluation and management of multi-organ system involvement. Genetics in Medicine. 2006;8(9):539-548.
[8] Borghi A, Corazza M, Minghetti S, Virgili A. Angiokeratoma circumscriptum: Successful treatment with argon laser. Dermatologic Therapy. 2010;23(3):308-311.
[9] Tsuji T, Sawabe M. Solitary angiokeratoma on the lower lip successfully treated with cryosurgery. Journal of Dermatology. 1994;21(7):499-501.
[10] Mehregan AH, Mehregan DA, Mehregan DR. Angiokeratomas: Clinical and histopathologic characteristics. Dermatology. 2002;204(1):31-37.