When a dermatologist removes a mole from your skin, you might wonder about the journey that tissue takes afterward. Understanding what happens to the tissue after my mole is removed can ease anxiety and help patients appreciate the careful medical process that ensures their safety and health. The removed tissue doesn't simply disappear—it embarks on a critical journey through laboratory analysis while the remaining tissue at the removal site begins a fascinating healing process.
This comprehensive guide explains both pathways: the laboratory analysis of the excised mole tissue and the natural healing process occurring at the wound site. Whether you're preparing for mole removal or recovering from the procedure, this article provides essential insights into the medical processes that protect your health.

When a healthcare provider removes a mole, the excised tissue doesn't get discarded. Instead, it's carefully preserved and sent to a specialized pathology laboratory for detailed examination. This standard medical practice serves a critical purpose: ruling out skin cancer and confirming the exact nature of the growth [1].
Even when a mole appears completely benign to the naked eye, microscopic analysis can reveal cellular changes invisible during visual examination. This histopathological biopsy represents an essential safety measure that protects patients from undetected skin cancer.
The tissue analysis process helps identify:
Understanding the different types of skin lesions helps patients appreciate why laboratory analysis is so important.
The journey of mole tissue through the laboratory follows a precise, standardized protocol:
Immediately after removal, the tissue specimen is placed in a special preservative solution called formalin. This chemical fixative prevents tissue decomposition and maintains cellular structure exactly as it appeared at the time of removal. The container is labeled with the patient's identifying information and details about the removal site.
Once the specimen arrives at the pathology laboratory, trained technicians log it into their system and begin processing. The tissue undergoes dehydration through a series of alcohol baths, then gets embedded in paraffin wax to create a solid block that can be sliced into extremely thin sections.
A specialized instrument called a microtome cuts the paraffin-embedded tissue into sections just 3-5 micrometers thick—thinner than a human hair. These ultra-thin slices are placed on glass slides for microscopic examination.
The tissue sections receive special stains, typically hematoxylin and eosin (H&E), which color different cellular components. Hematoxylin stains cell nuclei blue-purple, while eosin colors the cytoplasm and connective tissue pink. This contrast makes cellular details visible under the microscope.
A board-certified pathologist examines the stained tissue slides under high-powered microscopy. They evaluate:
The pathologist prepares a detailed report describing their findings and providing a definitive diagnosis. This report typically reaches the ordering physician within 5-10 business days, though urgent cases may receive expedited processing.
The pathology report contains technical medical terminology, but it essentially answers critical questions:
Report ElementWhat It Tells YouDiagnosisThe exact type of lesion (benign nevus, dysplastic nevus, melanoma, etc.)MarginsWhether the entire growth was removed with clear edgesDepthHow deeply any abnormal cells extended into the skinCell CharacteristicsSpecific features that determine risk levelRecommendationsWhether additional treatment or monitoring is needed
For patients concerned about atypical moles or potential melanoma, the pathology report provides definitive answers and guides future care decisions.
Sometimes the pathology report reveals findings that require follow-up:
Patients receiving concerning pathology results should consult with their healthcare provider or visit a specialized skin cancer clinic for expert guidance.
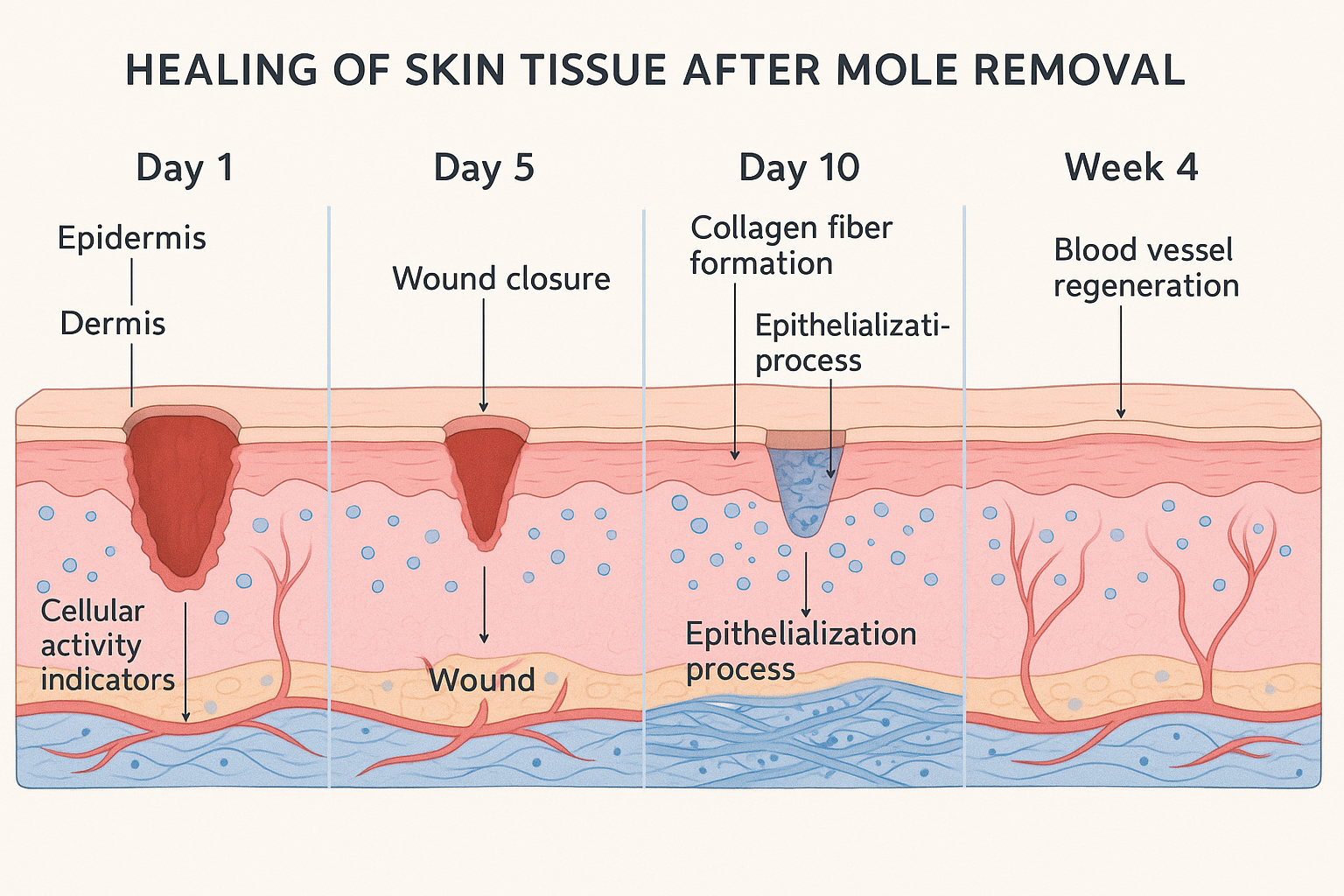
While the excised tissue travels to the laboratory, the tissue remaining at the removal site begins an equally important journey: the natural wound healing process. Understanding this biological response helps patients recognize normal healing versus complications requiring medical attention.
The moment a mole is removed, your body recognizes the disruption and immediately initiates protective mechanisms:
Blood Clotting 🩸
Within seconds, platelets rush to the wound site and begin forming a clot. This natural bandage stops bleeding and creates a protective barrier against infection. The clot eventually forms a scab that shields the healing tissue beneath.
Inflammation Phase
During the first few days after removal, the wound area may experience:
These symptoms represent the body's inflammatory response—a normal and necessary part of healing. White blood cells flood the area to prevent infection and begin cleaning cellular debris from the wound.
The healing process follows a predictable timeline, though individual variation occurs based on factors like removal method, location, and personal healing capacity.
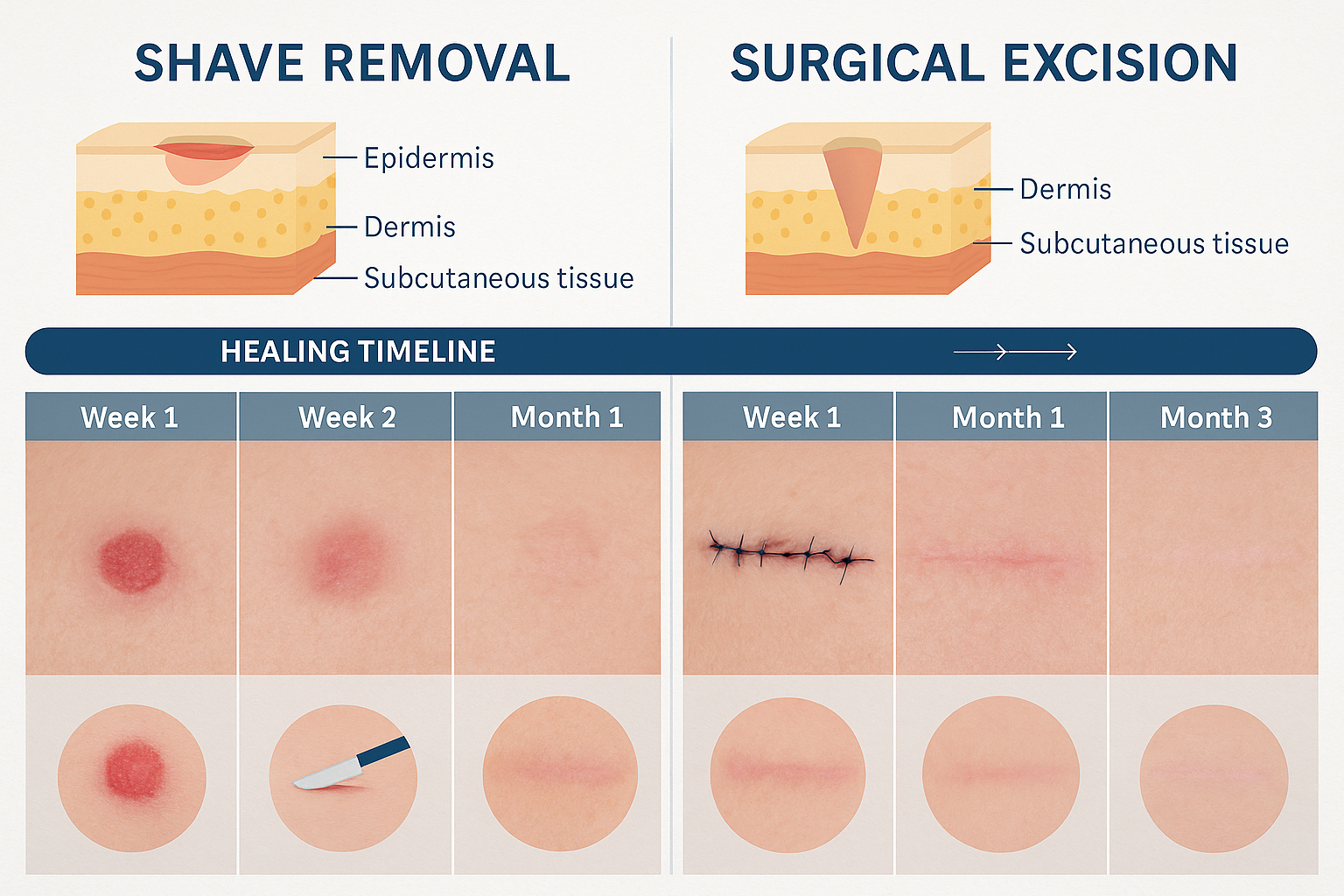
The timeline varies by removal method:
The removal technique significantly impacts what happens to the tissue after your mole is removed. Different methods create different wound types with varying healing characteristics.
Shave removal involves using a surgical blade to cut the mole flush with or slightly below the skin surface. This technique:
The limited tissue trauma means the body's healing response is less extensive, resulting in faster recovery and less prominent scarring.
Surgical excision cuts deeper into the skin to remove the entire mole plus a margin of surrounding tissue. This approach:
The deeper tissue disruption triggers a more robust healing response with more extensive collagen deposition and scar formation.
Laser removal works differently than cutting techniques. The laser energy:
The tissue response involves gradual pigment fading rather than wound closure, resulting in a different healing experience.
Understanding normal healing helps patients distinguish expected changes from complications requiring medical attention.
Normal Healing Signs ✅
Warning Signs Requiring Medical Attention ⚠️
Patients experiencing concerning symptoms should contact their healthcare provider promptly or visit The Minor Surgery Center for evaluation.
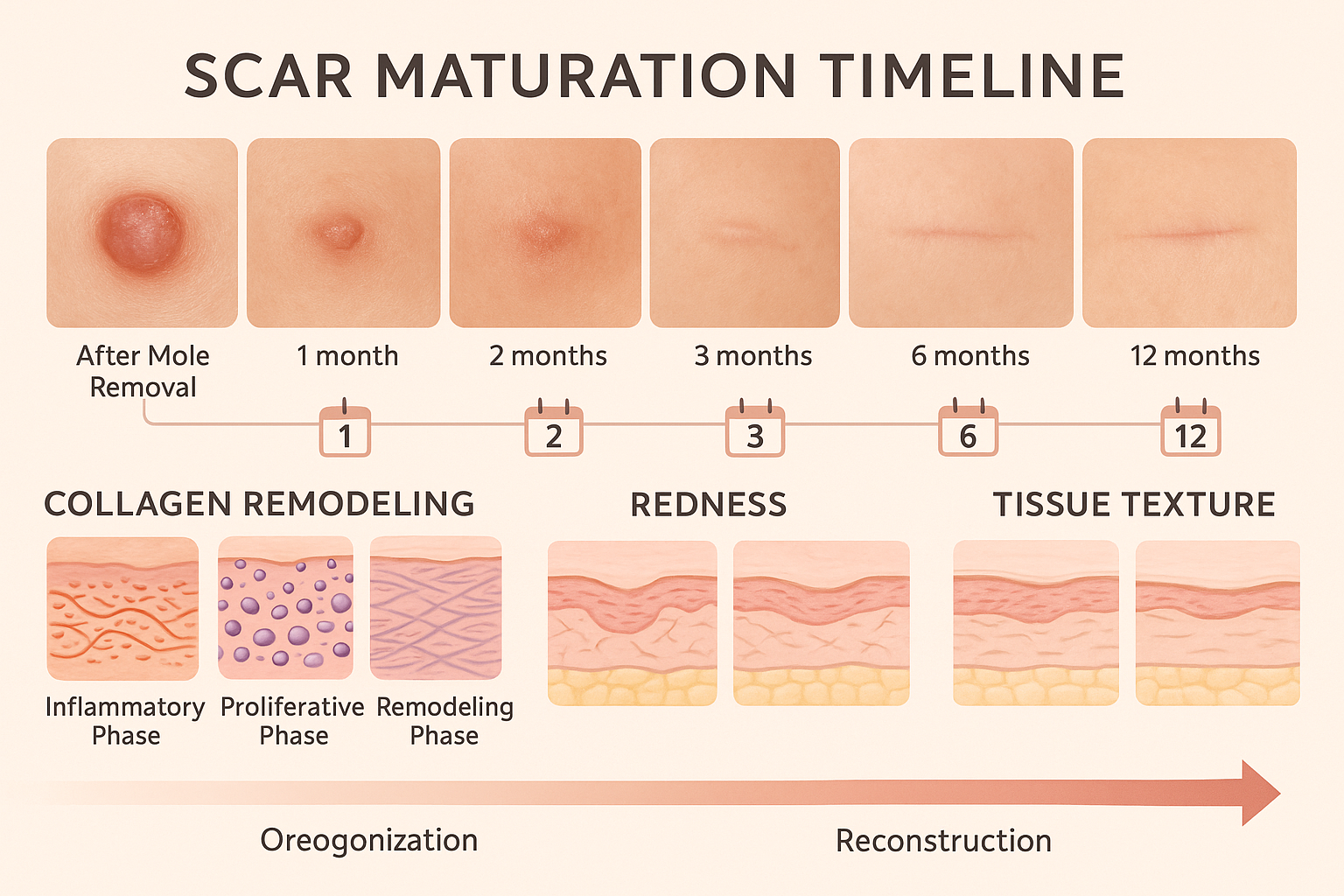
When tissue trauma extends into the deeper layers of skin (the dermis), the body cannot regenerate identical replacement tissue. Instead, it creates scar tissue—a specialized type of connective tissue that permanently marks the site of injury [11].
Scar formation represents the body's efficient solution to structural damage. When the dermis is disrupted:
Superficial injuries that only affect the epidermis (top skin layer) can heal without scarring because epidermal cells can regenerate perfectly. However, mole removal typically extends into the dermis, making some degree of scarring inevitable.
Scar tissue doesn't form instantly—it develops and changes over approximately one year following tissue removal [9]. This maturation process involves several phases:
"Scar tissue continues to develop and mature for approximately one year post-removal, with the scar fully formed by the one-year mark." [9]
Multiple factors influence how noticeable a scar becomes after mole removal:
Patient Factors:
Procedural Factors:
Aftercare Factors:
While some scarring is inevitable after mole removal extending into the dermis, several strategies can optimize the final appearance:
During the Healing Phase:
Long-Term Scar Management:
Patients concerned about scarring should discuss their concerns with their provider before the procedure. Choosing an experienced practitioner at facilities like The Minor Surgery Center in Barrie can help ensure optimal cosmetic outcomes.
The method used to remove a mole fundamentally determines what happens to the tissue after your mole is removed. Each technique creates a different type of wound with unique healing characteristics.
Removal MethodTissue DepthHealing TimeScarringStitches RequiredBest ForShave RemovalSuperficial (epidermis to upper dermis)2-3 weeksMinimal, often just color changeNoRaised moles, cosmetic removalSurgical ExcisionDeep (through dermis, possibly into fat)4-6 weeksLinear scar, more visibleYesSuspicious moles, complete removal neededLaser RemovalVariable (targets pigment)2-4 weeksMinimalNoFlat pigmented moles, cosmetic concernsCryotherapySuperficial to moderate2-3 weeksPossible lighteningNoBenign lesions, pre-cancerous spots
What Happens During the Procedure: The physician uses a small surgical blade to shave the mole flush with or slightly below the surrounding skin surface. Only the raised portion is removed, leaving the base of the mole cells in the dermis.
Tissue Response:
Advantages for Tissue Healing:
Limitations:
What Happens During the Procedure: The surgeon cuts around and beneath the mole, removing it entirely along with a margin of normal tissue. The wound edges are brought together with stitches.
Tissue Response:
Advantages for Tissue Healing:
Limitations:
What Happens During the Procedure: Concentrated light energy targets the pigment within mole cells, breaking them apart without cutting tissue.
Tissue Response:
Advantages for Tissue Healing:
Limitations:
Understanding these differences helps patients make informed decisions about which removal method best suits their needs and expectations for healing. For those exploring options, consulting with specialists who offer various techniques, such as those at The Minor Surgery Center, ensures personalized treatment planning.
While the body's healing mechanisms are largely automatic, patients can take specific actions to support optimal tissue recovery and minimize complications.
Wound Protection 🛡️
Managing Discomfort
Wound Cleaning
Activity Modifications
Monitoring for Complications
Check the wound daily for signs of infection or healing problems:
Scar Care Begins
Once the surface has closed and any scabs have fallen off:
Sun Protection ☀️
UV exposure can darken healing tissue and make scars more visible:
Scar Maturation Support
When to Consider Scar Treatment
If the scar remains prominently red, raised, or bothersome after several months, discuss options with your provider:
Proper nutrition supports tissue healing from the inside:
Protein: Essential for collagen production and tissue repair
Vitamin C: Critical for collagen synthesis
Zinc: Supports immune function and wound healing
Vitamin A: Promotes epithelial cell growth
Hydration: Adequate water intake supports all cellular processes
Healing varies by location due to differences in skin thickness, movement, and tension:
Face and Neck
Trunk (Chest, Back, Shoulders)
Extremities (Arms, Legs)
Understanding what happens to the tissue after your mole is removed at each healing stage empowers patients to actively support their recovery and recognize when professional intervention is needed.
The tissue remains in the pathology laboratory permanently. After examination, the tissue slides and paraffin blocks are archived and stored for many years (typically 10-20 years or more) for future reference if needed. This allows for second opinions or additional testing if questions arise later.
While legally the tissue belongs to the patient, practical considerations make this unusual. The tissue has been chemically preserved, embedded in wax, and sliced into microscopic sections—it's no longer in its original form. Most patients don't request tissue return, but you can discuss this with your healthcare provider if you have specific concerns.
This depends on the removal method:
If a mole does recur after removal, inform your healthcare provider, as this may warrant re-evaluation.
During weeks 2-4 after removal, the body actively builds new tissue and deposits collagen [13]. This creates a temporarily rough or textured feeling. As scar maturation continues over the following months, this texture typically softens and smooths.
Yes. The wound area typically remains red for weeks to months after the surface has healed [3]. This redness represents active scar maturation with abundant blood vessels supporting tissue remodeling. The color gradually fades over the first year. However, increasing redness or redness accompanied by warmth, swelling, or pain may indicate infection and requires medical evaluation.
While you can't dramatically accelerate healing, you can optimize it:
The body's healing timeline is largely predetermined by biological processes, but proper care ensures the best possible outcome within that timeframe.
If the pathology reveals atypical cells, dysplasia, or cancer, your healthcare provider will discuss next steps, which may include:
For concerning findings related to melanoma or other types of skin cancer, seeking care at a specialized facility ensures comprehensive management.
What happens to the tissue after your mole is removed involves two simultaneous journeys: the excised tissue travels to a pathology laboratory for microscopic analysis that rules out skin cancer and confirms diagnosis, while the tissue remaining at the wound site undergoes a remarkable natural healing process spanning weeks to months.
The laboratory analysis provides critical safety information, examining cellular details invisible to the naked eye and ensuring that what appeared benign truly is. This standard medical practice protects patients and guides appropriate follow-up care. Meanwhile, at the removal site, the body orchestrates a complex healing response—blood clotting, inflammation, epithelialization, and scar formation—that closes the wound and creates permanent tissue repair.
Key points to remember:
✅ Removed tissue undergoes professional pathology analysis to ensure accurate diagnosis and rule out cancer
✅ Healing timelines vary by removal method: shave removal heals in 2-3 weeks, while surgical excision requires 4-6 weeks for surface closure
✅ Scar maturation continues for approximately one year, with gradual fading and softening throughout this period
✅ Normal healing includes redness, texture changes, and mild discomfort—but increasing symptoms warrant medical attention
✅ Patient actions matter: proper wound care, sun protection, and healthy lifestyle choices support optimal healing
If you're considering mole removal:
If you've recently had a mole removed:
If you're awaiting pathology results:
For those seeking expert mole removal with comprehensive pathology services and attentive aftercare, The Minor Surgery Center offers specialized care focused on both medical accuracy and optimal cosmetic outcomes. Understanding what happens to the tissue after your mole is removed empowers you to participate actively in your care, recognize normal healing, and achieve the best possible results from your procedure.
The journey of tissue after mole removal—both the excised specimen and the healing wound—represents modern medicine's commitment to thorough diagnosis and natural healing processes working in harmony to protect your health and restore your skin.
[1] Medical literature on mole removal procedures and tissue handling protocols
[2] Dermatological pathology standards and practices
[3] Wound healing timeline studies and clinical observations
[4] Histopathological examination procedures
[5] Laser mole removal mechanisms and tissue response
[6] Post-procedural symptom expectations
[7] Epithelialization and wound closure research
[8] Tissue preservation and laboratory protocols
[9] Scar maturation timeline studies
[10] Collagen remodeling during healing
[11] Scar tissue formation mechanisms
[12] Comparative healing studies by removal method
[13] Clinical observations of healing progression
[14] Dermatological surgery best practices
[15] Pathology reporting standards
[16] Wound care recommendations
[17] Healing timeline variations by procedure type