Every year, thousands of people undergo mole removal procedures for cosmetic or medical reasons. While most procedures heal without complications, knowing the signs of infection after mole removal: what to watch for? can mean the difference between a smooth recovery and a serious medical emergency. Imagine waking up three days after your procedure to find your wound site red, swollen, and oozing—would you know whether this is normal healing or a dangerous infection requiring immediate attention?
Understanding the warning signs of infection after mole removal empowers patients to take swift action when something goes wrong. This comprehensive guide will walk you through everything you need to know about identifying, preventing, and responding to post-procedure infections, ensuring your recovery stays on track.

Mole removal is one of the most common minor surgical procedures performed worldwide. Whether you're having a mole removed for cosmetic reasons or medical evaluation, understanding the procedure helps you recognize when healing deviates from the normal path.
Different removal techniques carry varying infection risks:
Surgical Excision involves cutting out the entire mole and a small margin of surrounding skin, then closing the wound with stitches. This method creates a deeper wound that takes longer to heal, typically 1-3 weeks depending on location and size.
Shave Excision removes the mole at skin level using a small blade, leaving the wound to heal naturally without stitches. This technique generally heals faster (7-14 days) but may carry slightly higher infection risk due to the open wound nature.
Laser Removal uses concentrated light beams to break down mole cells, often used for smaller, non-cancerous moles. While minimally invasive, laser removal still creates a wound vulnerable to infection.
Cryotherapy freezes the mole tissue using liquid nitrogen, causing it to fall off over several days. The resulting blister and scab formation requires careful monitoring for infection signs.
Every surgical procedure that breaks the skin barrier creates an opportunity for bacteria to enter the body. The skin serves as our first line of defense against pathogens, and when this protective barrier is compromised, even temporarily, infection becomes possible[1].
Common sources of post-procedure infection include:
Studies show that infection rates after minor skin procedures range from 1-5% when proper sterile technique and post-operative care are followed[2]. However, this rate increases significantly with certain risk factors.
Understanding your personal risk profile helps you maintain appropriate vigilance during recovery. High-risk factors include:
Risk FactorImpact on Infection RiskPrevention StrategyDiabetes2-3x increased riskOptimize blood sugar control before procedureSmoking2x increased riskQuit smoking 2-4 weeks before procedureImmunosuppression3-5x increased riskConsider prophylactic antibioticsPoor circulation2x increased riskElevate affected area, promote blood flowObesity1.5-2x increased riskExtra attention to wound hygieneAdvanced age (>65)1.5x increased riskEnhanced monitoring and follow-upSteroid use2-3x increased riskDiscuss with physician before procedure
Location also matters significantly. Moles removed from areas with higher bacterial colonization (groin, armpits, feet) or areas prone to friction and moisture carry elevated infection risk compared to facial or arm removals.
The initial two days after mole removal represent a critical window for infection development. While some symptoms are part of normal healing, knowing the difference between expected post-procedure changes and early infection signs is crucial.
Expected Normal Healing (First 48 Hours):
✅ Mild to moderate pain that improves with over-the-counter pain medication
✅ Light pink to red coloration immediately around the wound edges
✅ Slight swelling within 1-2 cm of the removal site
✅ Clear to slightly pink fluid drainage (serous drainage)
✅ Mild warmth at the wound site
✅ Formation of a thin scab or crust over the wound
Early Warning Signs of Infection (First 48 Hours):
⚠️ Pain that worsens rather than improves after 24 hours
⚠️ Bright red coloration that extends beyond the immediate wound area
⚠️ Swelling that increases rather than stabilizes
⚠️ Cloudy, yellow, or greenish discharge
⚠️ Increasing warmth that spreads beyond the wound
⚠️ Wound edges that separate or gape open
⚠️ Foul odor from the wound site
Medical professionals use the "Red Flag Rule" to help patients identify concerning symptoms early. If you notice any of these red flags within the first 48 hours, contact your healthcare provider:
🚩 Expanding Redness: Redness that spreads more than 2-3 cm from the wound edge
🚩 Increasing Pain: Pain intensity that rises instead of decreasing
🚩 Fever Development: Body temperature above 100.4°F (38°C)
🚩 Pus Formation: Thick, opaque, colored discharge
🚩 Red Streaking: Lines extending from the wound toward the heart
Taking daily photos of your wound site provides invaluable documentation for tracking healing progress. Use these photography tips:
This documentation becomes especially valuable if you need to consult with your physician remotely or if symptoms develop gradually over several days.
The 3-7 day post-procedure window represents the peak period for infection manifestation. By this time, initial inflammation should be subsiding, and healing should progress steadily. Any deviation from this pattern warrants careful attention.
Day 3-4 Infection Indicators:
During this period, normal healing shows steady improvement with decreasing redness, swelling, and pain. Infection signs that may emerge include:
Day 5-7 Infection Progression:
If infection goes untreated, symptoms typically worsen during this period:
Not all wound drainage indicates infection. Understanding different discharge types helps you assess severity:
Discharge TypeColorConsistencySignificanceAction RequiredSerousClear to pale yellowThin, wateryNormal healingContinue routine careSerosanguineousPink, light redThin with blood tingeNormal early healingContinue routine careSanguineousBright redThin, bloodyMay indicate traumaApply pressure, monitorPurulentYellow, green, brownThick, opaqueBacterial infectionContact provider immediatelySeropurulentCloudy yellow-pinkModerately thickEarly infectionContact provider within 24 hours
The volume of discharge also matters. A small amount of serous drainage is expected, but soaking through multiple bandages daily suggests either excessive inflammation or infection.
Pain assessment provides crucial infection clues. Normal post-procedure pain follows a predictable pattern:
Normal Pain Trajectory:
Infection Pain Patterns:
If you're experiencing abnormal pain patterns, especially when combined with other infection signs, seeking medical evaluation is essential. For those in the Greater Toronto Area, specialized clinics in Barrie offer expert mole removal and post-operative care.
Certain infection symptoms represent medical emergencies that require immediate professional intervention. Delaying treatment when these signs appear can lead to serious complications including sepsis, tissue necrosis, or chronic wound problems.
🚨 Call 911 or Go to Emergency Department If You Experience:
Sepsis Warning Signs: Sepsis is a life-threatening condition where infection spreads throughout the bloodstream, triggering a systemic inflammatory response. Recognize it with the acronym SEPSIS:
Necrotizing Infection Signs: Rare but devastating, necrotizing soft tissue infections destroy skin, fat, and muscle tissue rapidly. Warning signs include:
Spreading Lymphangitis: Red streaks extending from the wound toward the torso indicate bacterial spread through lymphatic vessels. This requires immediate antibiotic intervention to prevent systemic infection.
Fever represents your body's immune response to infection, but not all post-procedure fevers indicate serious problems. Understanding fever patterns helps determine urgency:
Low-Grade Fever (99.5-100.4°F / 37.5-38°C):
Moderate Fever (100.5-102°F / 38.1-38.9°C):
High Fever (>102°F / >38.9°C):
Fever with Rigors (uncontrollable shaking chills):
Failing to address infection signs promptly can lead to serious complications:
Abscess Formation and Chronic Infection: Untreated bacterial infections often wall off into abscess cavities filled with pus. These require surgical drainage (incision and drainage procedure) and cannot be cleared with antibiotics alone. Chronic abscesses may require multiple drainage procedures and prolonged antibiotic courses.
Cellulitis and Deep Tissue Involvement: Surface infections can spread into deeper skin layers (dermis and subcutaneous tissue), causing extensive cellulitis. Severe cases may require hospitalization for intravenous antibiotics, especially if skin cancer screening revealed concerning pathology requiring additional procedures.
Scarring and Cosmetic Complications: Infected wounds heal poorly, often resulting in:
Systemic Infection: Bacteria entering the bloodstream can seed distant organs, causing:
The mortality rate for severe sepsis ranges from 10-20%, while septic shock carries mortality rates of 40-50%[4]. These statistics underscore the critical importance of recognizing and treating infection signs early.
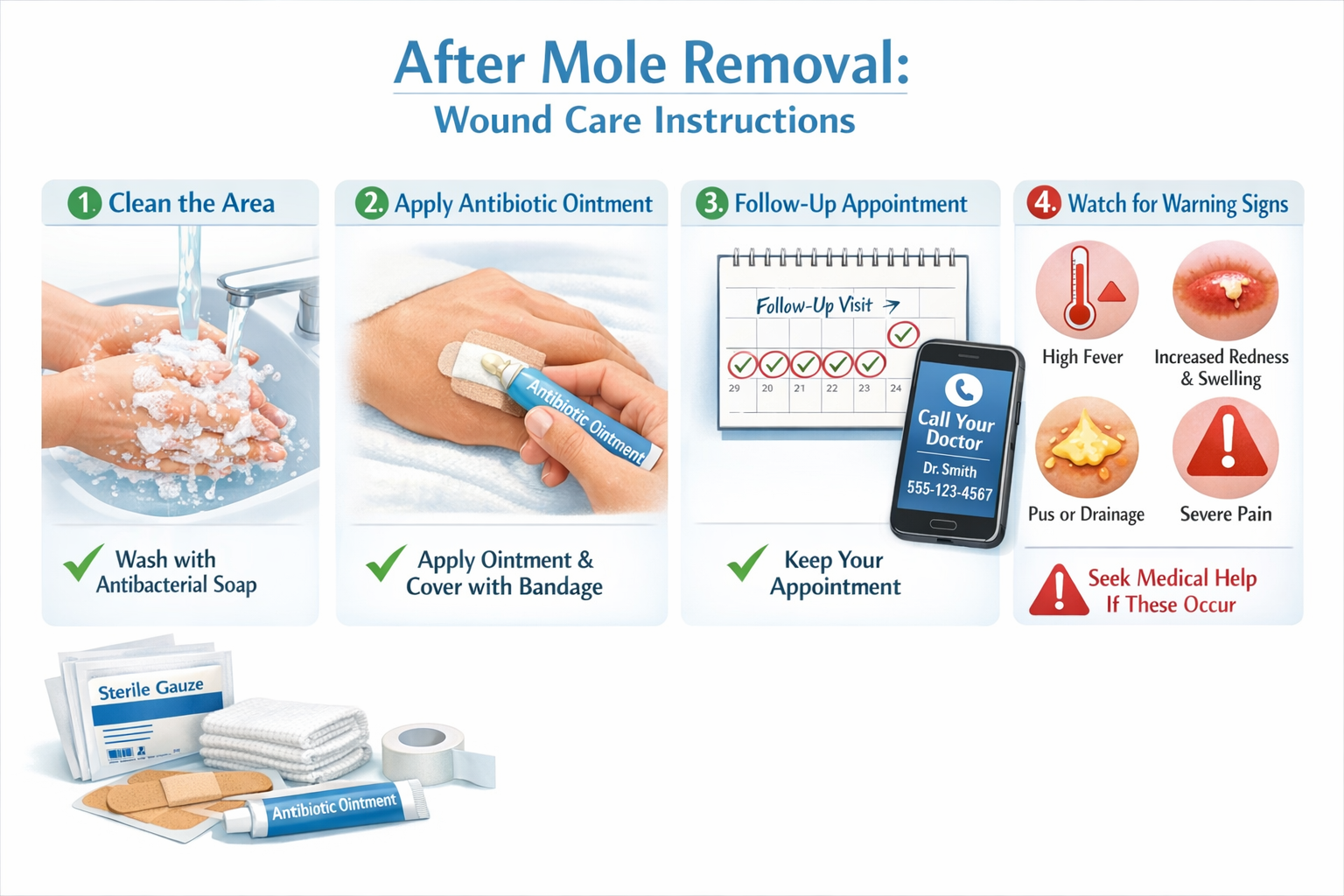
Prevention remains the most effective strategy against post-procedure infections. Following evidence-based wound care protocols reduces infection risk by up to 70%[5]. Understanding and implementing proper care techniques protects your healing wound.
The immediate post-procedure period sets the foundation for successful healing. Your healthcare provider will apply an initial dressing during the procedure, but understanding proper care from the moment you leave the clinic is essential.
Immediate Post-Procedure Instructions:
Keep the Initial Dressing Intact: Unless instructed otherwise, leave the original dressing in place for 24 hours. This protective barrier shields the wound from environmental bacteria during the most vulnerable period.
Avoid Water Exposure: Keep the wound completely dry for the first 24 hours. This means:
Minimize Physical Activity: Restrict movement that could stress the wound site:
Ice Application (If Recommended): Some providers recommend ice packs to reduce swelling:
Pain Management: Take prescribed or recommended pain medication as directed:
After the initial 24-hour period, you'll transition to active wound care. This phase requires diligent attention to cleaning, dressing changes, and monitoring.
Proper Wound Cleaning Technique:
Dressing Change Frequency: Most wounds require dressing changes once or twice daily, or whenever the dressing becomes wet or soiled. Your healthcare provider will give specific instructions based on your procedure type and wound characteristics.
As healing progresses, care requirements typically decrease, but vigilance remains important.
When to Stop Covering the Wound: Once the wound has sealed (no drainage, intact scab or closed incision), you may transition to leaving it uncovered. This usually occurs around day 7-14 but varies by individual. Benefits of air exposure include:
Suture Removal Timeline: If your mole removal involved stitches, removal timing depends on location:
Never attempt to remove sutures yourself unless specifically instructed. Premature removal risks wound dehiscence, while delayed removal can cause stitch marks or infection.
Scar Management: Once the wound has completely healed (typically 2-3 weeks), begin scar prevention:
For comprehensive information about various skin lesions and their removal, educational resources can help you understand what to expect during healing.
Certain lifestyle adjustments accelerate healing and reduce infection risk:
Nutrition for Wound Healing:
Sleep and Stress Management:
Smoking Cessation: If you smoke, quitting dramatically improves healing:
Alcohol Limitation: Excessive alcohol consumption:
Certain patient populations face elevated infection risks and require modified care approaches. If you fall into any high-risk category, discuss enhanced precautions with your healthcare provider before undergoing mole removal.
Diabetes significantly impacts wound healing through multiple mechanisms:
Impaired Immune Function: Elevated blood glucose levels reduce white blood cell effectiveness, decreasing the body's ability to fight bacteria. Studies show diabetics have 2-3 times higher infection rates after minor surgical procedures[6].
Reduced Blood Flow: Diabetes damages small blood vessels (microvascular disease), limiting oxygen and nutrient delivery to healing tissues. Poor perfusion slows healing and increases infection susceptibility.
Neuropathy Effects: Diabetic nerve damage may prevent patients from feeling pain that would normally signal infection, leading to delayed recognition and treatment.
Enhanced Precautions for Diabetic Patients:
Patients with weakened immune systems face the highest infection risks. Immunocompromising conditions include:
Modified Care Protocols:
Aging affects wound healing through several pathways:
Physiological Changes:
Social Factors:
Adapted Care Strategies:
Several medication classes affect wound healing and infection risk:
Anticoagulants and Antiplatelet Agents:
Corticosteroids:
Immunosuppressants:
Chemotherapy Agents:
If you're on any of these medications, never adjust doses without physician guidance. The risks of stopping certain medications may outweigh infection concerns, requiring individualized risk-benefit analysis.
Knowing when to reach out for professional guidance prevents both unnecessary anxiety and dangerous delays in treatment. Understanding the difference between routine follow-up questions and urgent concerns helps you communicate effectively with your healthcare team.
Routine Questions (Can Wait for Regular Office Hours):
Same-Day Contact Needed (Call Within Business Hours):
Urgent Contact Needed (Call Immediately, Even After Hours):
Emergency Department Visit (Do Not Wait):
When contacting your healthcare provider about potential infection, prepare this information:
Essential Details to Share:
Photos to Provide: Take clear, well-lit photos of the wound site from multiple angles. Include a ruler or coin for size reference. Many healthcare providers now accept secure photo uploads through patient portals, enabling remote assessment.
If your healthcare provider determines an in-person evaluation is needed, here's what typically occurs:
Physical Examination:
Diagnostic Testing (If Indicated):
Treatment Options:
For patients seeking specialized care, expert clinics provide comprehensive mole removal services with robust post-operative support and infection management protocols.
When infection occurs despite preventive measures, antibiotic therapy becomes necessary. Understanding antibiotic treatment helps ensure optimal outcomes and prevents complications like antibiotic resistance.
Healthcare providers select antibiotics based on likely bacterial pathogens, infection severity, and patient factors. Common choices include:
First-Line Oral Antibiotics:
Cephalexin (Keflex):
Dicloxacillin:
Trimethoprim-Sulfamethoxazole (Bactrim):
Doxycycline:
Clindamycin:
Why Full Completion Matters: Stopping antibiotics early, even when symptoms improve, allows surviving bacteria to multiply and potentially develop resistance. Studies show that incomplete antibiotic courses contribute significantly to antibiotic-resistant infections[7].
Adherence Strategies:
Managing Side Effects: Most antibiotic side effects are mild and manageable:
Occasionally, initial antibiotic therapy fails to resolve infection. Warning signs include:
Reasons for Treatment Failure:
Next Steps: Contact your healthcare provider if symptoms don't improve within 48-72 hours. You may need:
While infection monitoring focuses on wound healing, understanding your pathology report provides crucial information about the removed mole and may influence your follow-up care strategy.
After mole removal, the tissue is sent to a pathology laboratory where a pathologist examines it under a microscope. The report typically arrives 7-14 days after the procedure and includes:
Specimen Description: Details about the tissue received (size, color, characteristics)
Microscopic Findings: What the pathologist observed at cellular level
Diagnosis: The final determination of what the mole represents
Common Pathology Diagnoses:
Benign Nevus (Mole): Normal, non-cancerous mole requiring no further treatment
Dysplastic Nevus: Atypical mole with abnormal features that may require closer monitoring
Melanoma: Skin cancer requiring additional treatment and oncology referral
Basal Cell Carcinoma: Common skin cancer usually requiring margin evaluation
Squamous Cell Carcinoma: Skin cancer requiring assessment of invasion depth and margins
Margin Status: Critical information indicating whether the entire abnormal tissue was removed:
Certain pathology findings may influence infection monitoring:
Melanoma or Other Cancers: If skin cancer is diagnosed, additional surgical procedures may be needed. Multiple procedures increase cumulative infection risk and require extended vigilance.
Positive Margins: Requiring re-excision means a second wound in the same area, potentially while the first wound is still healing. This complicates wound care and increases infection vulnerability.
Immunosuppressive Treatments: If pathology reveals cancer requiring chemotherapy, radiation, or immunotherapy, these treatments will significantly impact wound healing and infection risk for any future procedures.
Your pathology results determine necessary follow-up:
Benign Results:
Atypical/Dysplastic Nevi:
Skin Cancer Diagnoses:
Understanding your pathology results empowers you to participate actively in your ongoing care and make informed decisions about future monitoring and treatment.
Once infection risk has passed and initial healing is complete (typically 2-3 weeks), attention shifts to long-term wound site monitoring and scar optimization.
Scars undergo predictable changes over 12-18 months:
Weeks 2-6 (Proliferative Phase):
Months 2-6 (Early Remodeling):
Months 6-18 (Mature Remodeling):
Factors Affecting Scar Appearance:
Sun Protection: UV exposure darkens scars and prevents normal fading:
Silicone Therapy: Gold standard for scar prevention and treatment:
Massage Therapy: Gentle scar massage after complete healing:
Topical Treatments:
Advanced Treatments (if needed for problematic scars):
Most scars improve satisfactorily with time and basic care, but certain situations warrant professional evaluation:
Hypertrophic Scars: Raised, red scars that remain within the original wound boundaries but don't flatten over time. Treatment options include steroid injections, pressure therapy, or laser treatment.
Keloid Scars: Raised scars that grow beyond the original wound boundaries, more common in darker skin types and certain body areas (chest, shoulders, earlobes). Require specialized treatment to prevent recurrence.
Contracture Scars: Scars that tighten and restrict movement, particularly problematic near joints. May require surgical release and physical therapy.
Hyperpigmentation: Darkened scars that don't fade appropriately. Treatments include hydroquinone, laser therapy, or chemical peels.
Scar Pain or Sensitivity: Persistent tenderness, pain, or abnormal sensations at the scar site may indicate nerve entrapment or neuroma formation requiring evaluation.
If your mole was removed due to abnormal features or cancer diagnosis, long-term monitoring of the removal site is essential:
Self-Examination Schedule:
Warning Signs at Removal Site:
Professional Surveillance:
For comprehensive information about various types of cysts and lesions that may require removal and monitoring, educational resources help patients understand what to watch for during long-term follow-up.
Infection rates after mole removal procedures range from 1-5% when proper sterile technique and post-operative care are followed[2]. The rate varies based on removal method, location, patient risk factors, and adherence to wound care instructions. Shave excisions may have slightly higher infection rates than surgical excisions due to the open wound nature, while laser removal typically has lower rates.
Showering guidelines depend on your specific procedure and provider instructions. Generally:
Always follow your healthcare provider's specific instructions, as recommendations may vary based on wound size, location, and closure method.
An infected mole removal site typically displays:
In contrast, normal healing shows light pink coloration immediately around the wound, clear to slightly pink drainage, mild swelling that decreases over time, and gradual improvement in all symptoms.
Any pus formation warrants attention, as pus indicates bacterial infection. However, the amount and associated symptoms determine urgency:
Small amount of pus with no other symptoms: Contact your healthcare provider within 24 hours for evaluation. This may represent early, localized infection treatable with oral antibiotics.
Pus with fever, spreading redness, or increasing pain: Contact your provider immediately or seek same-day evaluation. These combinations suggest more significant infection requiring prompt treatment.
Large amount of pus or foul-smelling discharge: Seek urgent medical evaluation, as this may indicate abscess formation requiring drainage.
Never attempt to squeeze or drain pus yourself, as this can introduce additional bacteria and worsen the infection.
Over-the-counter antibiotic ointments like bacitracin or polysporin are commonly recommended for wound care after mole removal and can help prevent infection. However:
Prevention vs. Treatment: These ointments help prevent infection when applied to clean wounds but cannot treat established infections. If infection signs develop, prescription oral antibiotics are necessary.
Application Guidelines:
When NOT to use:
Always follow your healthcare provider's specific instructions, as some wounds heal better with minimal ointment application.
Healing timelines vary based on removal method, location, and individual factors:
Shave Excision:
Surgical Excision with Sutures:
Laser Removal:
Factors Affecting Healing Speed:
Accidental trauma to a healing mole removal site requires assessment and appropriate response:
Minor Bumps (No Bleeding or Opening):
Trauma Causing Bleeding:
Trauma Causing Wound Opening:
Suture Disruption:
Prevention strategies include:
Understanding the signs of infection after mole removal: what to watch for? transforms you from a passive patient into an active participant in your healing process. While the vast majority of mole removals heal without complications, your ability to recognize early warning signs and respond appropriately can prevent minor issues from becoming serious medical problems.
Before Your Procedure:
During the First Week:
Throughout Your Recovery:
Long-Term:
Remember that healthcare providers expect and welcome questions about your recovery. It's always better to contact your provider about a concern that turns out to be normal healing than to delay treatment for a developing infection. Trust your instincts—if something doesn't feel right, seek guidance.
For patients in Ontario seeking expert mole removal services with comprehensive post-operative support, specialized clinics offer professional care and infection management. Access to experienced providers who prioritize patient education and follow-up care significantly reduces complication risks and ensures optimal outcomes.
While your healthcare team provides expertise and treatment, you remain the most important member of your care team. Your daily wound monitoring, adherence to care instructions, and prompt reporting of concerns directly impact your recovery success. By understanding what to watch for and when to act, you've taken an important step toward ensuring your mole removal heals properly and completely.
The knowledge you've gained about infection signs, prevention strategies, and appropriate responses empowers you to navigate your recovery with confidence. Whether your mole removal was performed for cosmetic reasons or medical necessity, protecting your healing wound from infection ensures the best possible outcome—a well-healed site with minimal scarring and no complications.
Stay vigilant, follow your care instructions, and don't hesitate to reach out to your healthcare provider whenever questions or concerns arise. Your proactive approach to monitoring and care is the foundation of successful healing after mole removal.
[1] Bowler, P. G., Duerden, B. I., & Armstrong, D. G. (2001). Wound microbiology and associated approaches to wound management. Clinical Microbiology Reviews, 14(2), 244-269.
[2] Heal, C., Buettner, P., & Browning, S. (2009). Risk factors for wound infection after minor surgery in general practice. Medical Journal of Australia, 191(3), 143-147.
[3] Phoenix, G., Das, S., & Joshi, M. (2012). Diagnosis and management of cellulitis. British Medical Journal, 345, e4955.
[4] Angus, D. C., & van der Poll, T. (2013). Severe sepsis and septic shock. New England Journal of Medicine, 369(9), 840-851.
[5] Dumville, J. C., McFarlane, E., Edwards, P., Lipp, A., & Holmes, A. (2015). Preoperative skin antiseptics for preventing surgical wound infections after clean surgery. Cochrane Database of Systematic Reviews, (4), CD003949.
[6] Jeon, C. Y., Furuya, E. Y., Berman, M. F., & Larson, E. L. (2012). The role of pre-operative and post-operative glucose control in surgical-site infections and mortality. PLoS One, 7(9), e45616.
[7] Llor, C., & Bjerrum, L. (2014). Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Therapeutic Advances in Drug Safety, 5(6), 229-241.
[8] Mustoe, T. A., Cooter, R. D., Gold, M. H., et al. (2002). International clinical recommendations on scar management. Plastic and Reconstructive Surgery, 110(2), 560-571.