Every year, thousands of people search online for quick, affordable ways to remove unwanted moles at home. Among the most common DIY approaches is using over-the-counter wart removers containing salicylic acid—products designed to dissolve warts but increasingly misused on moles. What seems like a simple, cost-effective solution can quickly turn into a medical nightmare involving chemical burns, permanent scarring, infections, and most alarmingly, the potential masking of skin cancer. Understanding Salicylic Acid and Wart Removers on Moles: Why DIY Mole 'Burn-Off' Is Risky is essential for anyone considering at-home mole removal in 2025.
The allure of DIY mole removal is understandable. Professional removal can be expensive, and many people feel self-conscious about visible moles. However, the risks associated with using salicylic acid and other wart removers on moles far outweigh any perceived benefits. This comprehensive guide explores the science behind why this practice is dangerous, the potential complications, and the safe, professional alternatives available.
Before exploring why Salicylic Acid and Wart Removers on Moles: Why DIY Mole 'Burn-Off' Is Risky, it's essential to understand the fundamental biological differences between moles and warts.
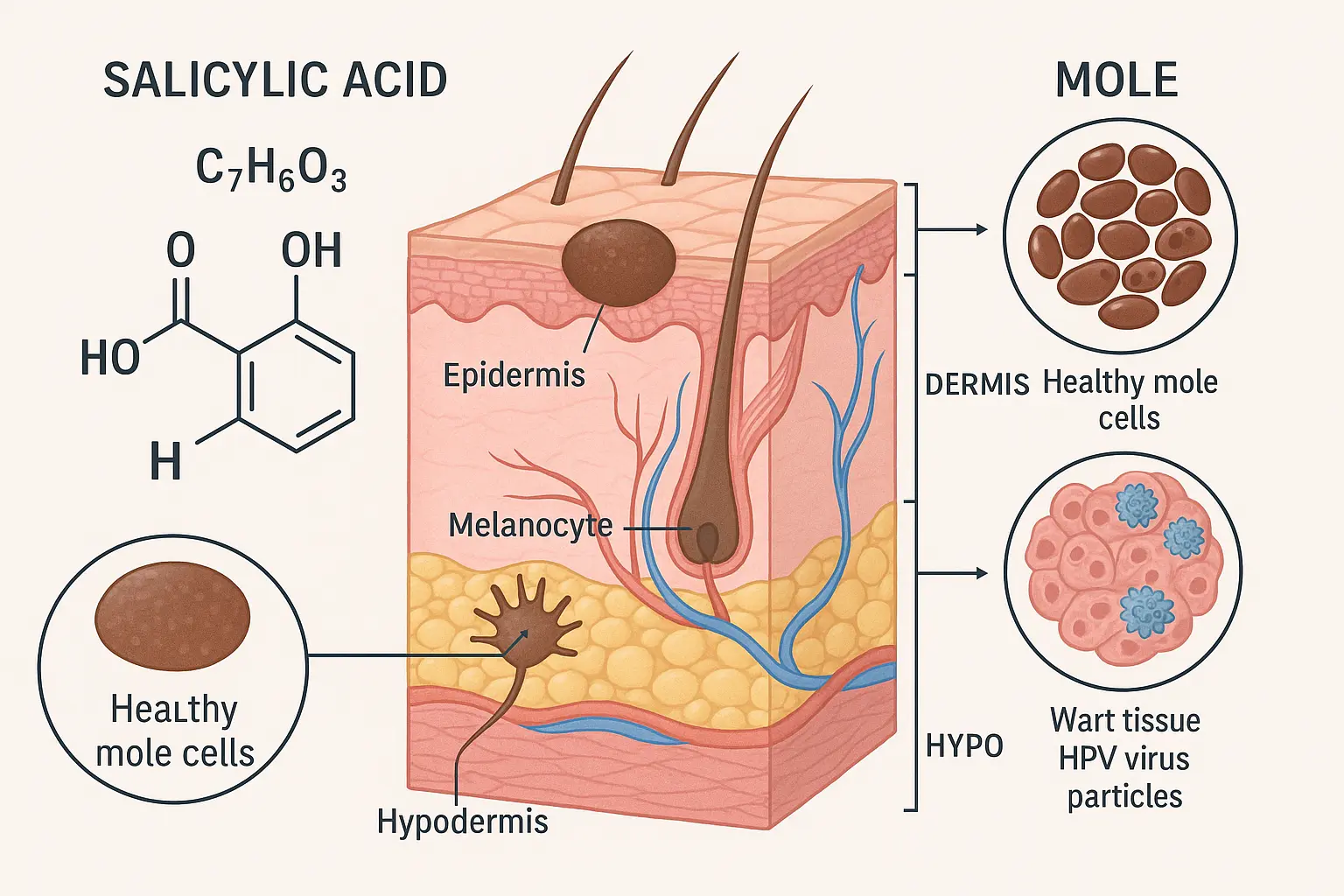
Moles (medical term: nevi) are clusters of pigment-producing cells called melanocytes that appear as brown, black, or flesh-colored spots on the skin. They develop when melanocytes grow in groups rather than spreading evenly throughout the skin[1]. Most people have between 10 and 40 moles that appear during childhood and adolescence, though new moles can develop throughout life.
Moles have several important characteristics:
For more information about different types of moles, visit our guide on atypical moles.
Warts are benign skin growths caused by human papillomavirus (HPV) infection. Unlike moles, warts are viral infections that affect the top layer of skin, causing rapid cell growth that creates rough, raised bumps[2].
Key wart characteristics include:
The biological distinction between moles and warts is precisely why salicylic acid—designed for warts—is dangerous for moles:
FeatureWartsMolesCauseHPV viral infectionMelanocyte cell clustersDepthSuperficial (epidermis)Deep (dermis and below)Cell TypeInfected keratinocytesMelanocytesCancer RiskNonePotential melanoma developmentTreatment MechanismDissolve infected tissueRequires complete excisionBiopsy NecessityNot requiredOften medically necessary
Understanding these differences makes it clear why products designed for one condition should never be used for the other.
Salicylic acid is a keratolytic agent, meaning it breaks down keratin—the protein that makes up the outer layer of skin and the bulk of wart tissue[3]. When applied to warts, salicylic acid:
This mechanism works well for warts because they're composed primarily of excess keratin in the superficial skin layers. The acid concentration in over-the-counter products (typically 17-40%) is calibrated to dissolve this specific tissue type.
Moles are fundamentally different structures that don't respond to keratolytic agents:
⚠️ Critical Point: Using salicylic acid on a mole is like trying to remove a tree by pouring acid on its leaves—you might damage the surface, but the roots remain, and you've created unnecessary destruction in the process.
When salicylic acid contacts mole tissue, several harmful processes occur:
This process explains why DIY attempts rarely succeed and almost always cause complications worse than the original mole.
Understanding Salicylic Acid and Wart Removers on Moles: Why DIY Mole 'Burn-Off' Is Risky requires examining the specific complications that frequently occur.
Salicylic acid concentrations in wart removers are strong enough to cause significant chemical burns when misapplied to moles:
The skin surrounding moles is often normal, healthy tissue that becomes collateral damage during DIY removal attempts. These burns can take weeks to months to heal and frequently leave permanent marks.
Perhaps the most common complication of using salicylic acid on moles is permanent scarring that's often more noticeable than the original mole:
Types of scars that develop:
"I tried removing a small mole on my cheek with a wart remover. Now I have a dark, raised scar three times the size of the original mole. I wish I had just gone to a dermatologist from the start." — Common patient testimonial
Professional mole removal techniques minimize scarring through precise excision, proper wound closure, and optimal healing conditions—advantages impossible to replicate at home.
DIY mole removal creates open wounds without the sterile conditions necessary for safe healing:
Common infectious complications:
Signs of infection include:
Infections can lead to additional scarring, prolonged healing, antibiotic treatment, and in rare cases, serious systemic illness.
This is the most critical reason why Salicylic Acid and Wart Removers on Moles: Why DIY Mole 'Burn-Off' Is Risky—the potential to hide or destroy evidence of skin cancer.
Approximately 1 in 5 Americans will develop skin cancer by age 70[4]. Many skin cancers, particularly melanoma, begin as or resemble normal moles. The only way to definitively determine if a mole is cancerous is through biopsy and pathological examination.
When you attempt DIY removal:
Melanoma is the deadliest form of skin cancer, responsible for the vast majority of skin cancer deaths. Early detection is critical—the 5-year survival rate for melanoma caught early is 99%, but drops to 27% once it spreads to distant organs[5].
Warning signs of melanoma (ABCDE rule):
If a mole displays any of these characteristics and you remove it at home, you've potentially eliminated crucial evidence and delayed life-saving diagnosis.
Learn more about melanoma detection at our best skin cancer clinic page.
It's not just melanoma—other skin cancers can be mistaken for benign moles:
For more information, read our comprehensive guide on 4 types of skin cancer.
Even when DIY removal appears successful initially, regrowth is extremely common:
This cycle of removal and regrowth leads to progressively worse cosmetic outcomes and increased health risks.
Salicylic acid and other ingredients in wart removers can cause:
These reactions are unpredictable and can affect areas beyond the treatment site.
While this article focuses on Salicylic Acid and Wart Removers on Moles: Why DIY Mole 'Burn-Off' Is Risky, it's worth briefly addressing other popular DIY methods—all of which carry similar or greater risks:
Claimed mechanism: Acid in vinegar burns away mole tissue
Reality: Causes chemical burns, scarring, and pain without proper removal
Risk level: ⚠️⚠️⚠️ High
Claimed mechanism: Dries out and removes mole
Reality: Skin irritation, burns, and staining without effective removal
Risk level: ⚠️⚠️⚠️ High
Claimed mechanism: Natural enzymes dissolve mole
Reality: Chemical burns from sulfur compounds, no actual mole removal
Risk level: ⚠️⚠️ Moderate to High
Claimed mechanism: Freeze and kill mole cells
Reality: Designed for warts, not moles; causes tissue damage and incomplete removal
Risk level: ⚠️⚠️⚠️ High
Claimed mechanism: Physical removal of mole
Reality: Extreme infection risk, severe scarring, bleeding, and incomplete removal
Risk level: ⚠️⚠️⚠️⚠️ Very High
Claimed mechanism: Herbal ingredients dissolve moles
Reality: Often contain undisclosed acids or caustic substances; unpredictable results and complications
Risk level: ⚠️⚠️⚠️ High
None of these methods are recommended by medical professionals. They all carry risks of scarring, infection, incomplete removal, and most critically, the potential to mask skin cancer.
For safe alternatives, explore our mole removal services.
Certain mole characteristics require immediate professional evaluation, regardless of any DIY removal considerations:
Annual skin cancer screenings are recommended for high-risk individuals and every 2-3 years for average-risk adults. During these exams, dermatologists:
Early detection through professional screening saves lives. Learn more about 25 types of skin lesions to better understand what professionals look for.
Understanding Salicylic Acid and Wart Removers on Moles: Why DIY Mole 'Burn-Off' Is Risky naturally leads to the question: what are the safe alternatives?
Qualified healthcare providers offer several proven, safe mole removal methods:
Best for: Potentially cancerous moles, large moles, or deep moles
Procedure:
Advantages:
Disadvantages:
Best for: Raised moles, benign-appearing lesions
Procedure:
Advantages:
Disadvantages:
Best for: Small, benign moles; cosmetic removal in sensitive areas
Procedure:
Advantages:
Disadvantages:
Important: Laser removal should only be used for confirmed benign moles, never for suspicious lesions.
Best for: Certain benign lesions (rarely used for moles)
Procedure:
Advantages:
Disadvantages:
Who can safely remove moles?
✅ Dermatologists: Skin specialists with extensive training in mole evaluation and removal
✅ Plastic surgeons: Experts in cosmetic outcomes and complex removals
✅ General surgeons: Qualified for mole excision, especially in medical settings
✅ Trained family physicians: Can perform simple removals with proper training
❌ Avoid: Spas, beauty salons, unlicensed practitioners, or anyone offering non-medical removal
Understanding the process helps reduce anxiety:
Before the procedure:
During the procedure:
After the procedure:
Healing timeline:
Professional mole removal costs vary based on:
Insurance coverage: Most insurance plans cover mole removal when:
Cost comparison:
The small additional cost of professional removal is insignificant compared to the value of safety, proper diagnosis, and optimal cosmetic outcomes.
Explore professional options at The Minor Surgery Center.
One of the most critical aspects of professional mole removal that DIY methods completely eliminate is pathological examination.
After surgical mole removal, the tissue is sent to a pathology laboratory where:
Benign diagnoses:
Atypical/Precancerous findings:
Malignant diagnoses:
Additional information:
The pathology report determines:
When you remove a mole at home, you forfeit all of this critical medical information.
While respecting patient privacy, healthcare providers frequently encounter complications from DIY mole removal attempts. These scenarios illustrate why Salicylic Acid and Wart Removers on Moles: Why DIY Mole 'Burn-Off' Is Risky:
A 34-year-old woman removed a "bothersome" mole on her shoulder using a salicylic acid wart remover over several weeks. The mole appeared to fade, leaving a light scar. Two years later, she developed swollen lymph nodes under her arm. Biopsy revealed metastatic melanoma—cancer that had spread from the original mole site. Without the original tissue, staging was impossible, and treatment options were limited. Early detection could have resulted in simple removal with near-certain cure.
A 28-year-old man used wart remover on a facial mole, hoping to improve his appearance before his wedding. The treatment caused a severe chemical burn, resulting in a raised, dark keloid scar significantly larger and more noticeable than the original mole. Multiple scar revision procedures improved but couldn't completely eliminate the disfigurement. Professional removal would have cost $200 and left a nearly invisible scar.
A 45-year-old woman applied salicylic acid to a mole on her leg, creating an open wound. Within days, the area became red, swollen, and painful. She developed cellulitis requiring hospitalization, IV antibiotics, and wound care. The infection left permanent scarring and cost thousands in medical bills—far more than professional removal would have cost.
A 52-year-old man repeatedly treated a back mole with wart remover over six months. The mole appeared lighter but never fully disappeared. When he finally consulted a dermatologist, biopsy revealed an atypical nevus with severe dysplasia (precancerous changes). Wide excision was required to ensure complete removal. The repeated chemical exposure had complicated the tissue architecture, making pathological interpretation more difficult.
These scenarios are not rare exceptions—they represent common outcomes of DIY mole removal attempts that dermatologists encounter regularly.
Beyond avoiding DIY removal, protecting your skin health requires proactive measures:
UV radiation is the primary modifiable risk factor for skin cancer:
Daily sun protection:
Special considerations:
Monthly self-skin exams help detect changes early:
How to perform a self-exam:
What to look for:
For high-risk individuals, advanced monitoring techniques include:
Digital mole mapping:
Benefits:
Learn about modern monitoring approaches in our article on 3D mole mapping apps.
Additional protective measures:
No. No mole should be removed at home, regardless of appearance. Even benign-looking moles require professional evaluation to rule out malignancy and ensure complete, safe removal with optimal cosmetic results.
Many dermatologists offer payment plans for cosmetic procedures. Additionally, if a mole has any concerning features, removal may be covered by insurance as medically necessary. Consult with a provider to discuss options—the cost of complications from DIY removal often exceeds professional removal costs.
Use the ABCDE rule: Asymmetry, Border irregularity, Color variation, Diameter >6mm, and Evolving (changing). Any of these features warrants professional evaluation. However, only pathological examination can definitively determine if a mole is cancerous.
All removal methods leave some evidence, but professional techniques minimize scarring. Surgical excision typically leaves a thin line scar that fades significantly over 6-12 months. This is far preferable to the irregular, hyperpigmented, or keloid scars common with DIY removal.
See a dermatologist immediately. Bring information about what product you used and when. The provider can assess for complications, evaluate the area for residual mole tissue or concerning changes, and develop an appropriate treatment plan. Be honest about DIY attempts—doctors need complete information to provide optimal care.
No. Many "natural" products contain undisclosed acids or caustic substances. They carry the same risks as other DIY methods: scarring, infection, incomplete removal, and potential masking of skin cancer. Natural does not mean safe or effective.
The procedure itself typically takes 15-30 minutes. Including consultation, preparation, and post-procedure instructions, plan for a 45-60 minute appointment. This small time investment provides safe, complete removal with pathology examination.
With complete surgical excision, recurrence is rare (<5%). Shave excision has slightly higher recurrence rates (10-15%) because some deep cells may remain. Laser removal has the highest recurrence rate. If a mole returns after professional removal, it should be re-evaluated.
For more information about professional services, visit our Barrie mole removal page.
The temptation to save money and time with DIY mole removal is understandable, but the risks far outweigh any perceived benefits. Salicylic Acid and Wart Removers on Moles: Why DIY Mole 'Burn-Off' Is Risky comes down to several undeniable facts:
✅ Moles and warts are fundamentally different biological structures requiring different treatments
✅ Salicylic acid doesn't effectively remove moles but does cause burns, scars, and complications
✅ DIY removal eliminates the possibility of pathology examination, potentially allowing cancer to progress undetected
✅ Professional removal is safe, effective, and provides peace of mind through proper diagnosis
✅ The cost of treating DIY complications often exceeds professional removal costs
Your skin is your body's largest organ and your first line of defense against the environment. It deserves professional care when something needs to be removed. Moles, unlike warts, carry potential health implications that require medical expertise to properly evaluate and address.
Understanding Salicylic Acid and Wart Removers on Moles: Why DIY Mole 'Burn-Off' Is Risky is essential for anyone considering at-home mole removal in 2025. The science is clear: salicylic acid and other wart removers are designed for viral wart tissue, not the melanocyte cell clusters that form moles. Using these products on moles causes chemical burns, permanent scarring, infections, and most critically, eliminates the ability to detect skin cancer through pathological examination.
The risks of DIY mole removal—disfiguring scars, serious infections, incomplete removal, and masked melanoma—are simply not worth the modest cost savings. Professional mole removal by qualified dermatologists or surgeons offers safe, complete removal with optimal cosmetic outcomes and the critical benefit of tissue diagnosis.
If you have moles that concern you or that you'd like removed:
Your skin health is too important to risk with unproven, dangerous DIY methods. Professional care provides safety, accuracy, and peace of mind that no over-the-counter product can match.
For expert mole evaluation and safe removal, contact The Minor Surgery Center to schedule a consultation. Don't let a simple desire for mole removal turn into a serious health complication—choose professional care and protect your skin health for life.
[1] American Academy of Dermatology Association. (2024). "Moles: Overview." AAD.org. Retrieved from https://www.aad.org/public/diseases/a-z/moles-overview
[2] American Academy of Dermatology Association. (2024). "Warts: Diagnosis and Treatment." AAD.org. Retrieved from https://www.aad.org/public/diseases/a-z/warts-treatment
[3] Arif, T. (2015). "Salicylic acid as a peeling agent: a comprehensive review." Clinical, Cosmetic and Investigational Dermatology, 8, 455-461. doi:10.2147/CCID.S84765
[4] American Academy of Dermatology Association. (2024). "Skin Cancer: By the Numbers." AAD.org. Retrieved from https://www.aad.org/media/stats-skin-cancer
[5] American Cancer Society. (2024). "Survival Rates for Melanoma Skin Cancer." Cancer.org. Retrieved from https://www.cancer.org/cancer/melanoma-skin-cancer/detection-diagnosis-staging/survival-rates-for-melanoma-skin-cancer-by-stage.html