A pathology report lands in the patient portal, and suddenly everyday life feels like it paused. The document is packed with medical jargon—words like "architectural atypia," "positive margins," and "compound dysplastic nevus with moderate cytologic atypia." For most people, reading it feels like trying to decode a foreign language under stress. This guide—pathology report explained (plain English): margins, atypia, dysplastic nevus—breaks down every confusing term into simple, everyday language so that anyone can understand what their report actually says and what it means for their health in 2026.
Every year, millions of skin biopsies are performed across North America. Approximately 34% of dysplastic nevi show positive biopsy margins, meaning abnormal cells reach the very edge of the tissue that was removed [1]. That single statistic proves why understanding the language on a pathology report is not optional—it is essential. Whether a doctor removed a suspicious mole, performed a shave biopsy, or completed a full excision, the pathology report is the document that determines what happens next.
This glossary-style article walks through each key term step by step. No medical degree required. 🩺

A pathology report is a medical document written by a pathologist—a doctor who specializes in examining tissue under a microscope. After a mole, cyst, or skin lesion is removed, the tissue sample (called a specimen) goes to a laboratory. The pathologist slices the tissue into thin sections, stains them with special dyes, and studies them under high magnification. The resulting report describes exactly what the tissue looks like at a cellular level [6].
The pathology report is the definitive answer about a skin lesion. Clinical examination (what the doctor sees with the naked eye or a dermatoscope) is an educated guess. The pathology report is the verdict. It determines:
For a deeper overview of what to expect after a mole is removed and sent to the lab, see this helpful guide on demystifying your pathology report after mole removal.
SectionWhat It Tells YouPatient InformationName, date of birth, medical record numberClinical HistoryWhy the biopsy was done; what the doctor suspectedSpecimen Description (Gross)Size, shape, and color of the tissue as seen without a microscopeMicroscopic DescriptionWhat the cells look like under the microscopeDiagnosisThe pathologist's final conclusion (e.g., "compound dysplastic nevus with moderate atypia")MarginsWhether abnormal cells reach the edge of the removed tissueComments / RecommendationsSuggestions for follow-up or re-excision
In pathology, margins refer to the edges of the tissue specimen that was removed. Think of it like cutting a shape out of a piece of fabric. The margin is the border between the shape that was cut and the surrounding fabric that was left behind.
When a pathologist examines margins, the question is simple:
"Do the abnormal cells reach the very edge of the tissue that was removed, or is there a buffer zone of normal tissue surrounding them?"
Negative margins (also called clear margins or free margins) mean that the abnormal or atypical cells do not extend to the edge of the specimen. There is a rim of normal, healthy tissue all the way around the lesion. This is the ideal result because it suggests the entire lesion was removed [6].
Positive margins mean that abnormal cells do extend to the edge of the removed tissue. This raises the possibility that some atypical cells may still remain in the body at the biopsy site [6].
📌 Important: A positive margin does not automatically mean cancer. It means the removal was potentially incomplete, and the doctor must decide whether to re-excise (remove more tissue) or monitor the site.
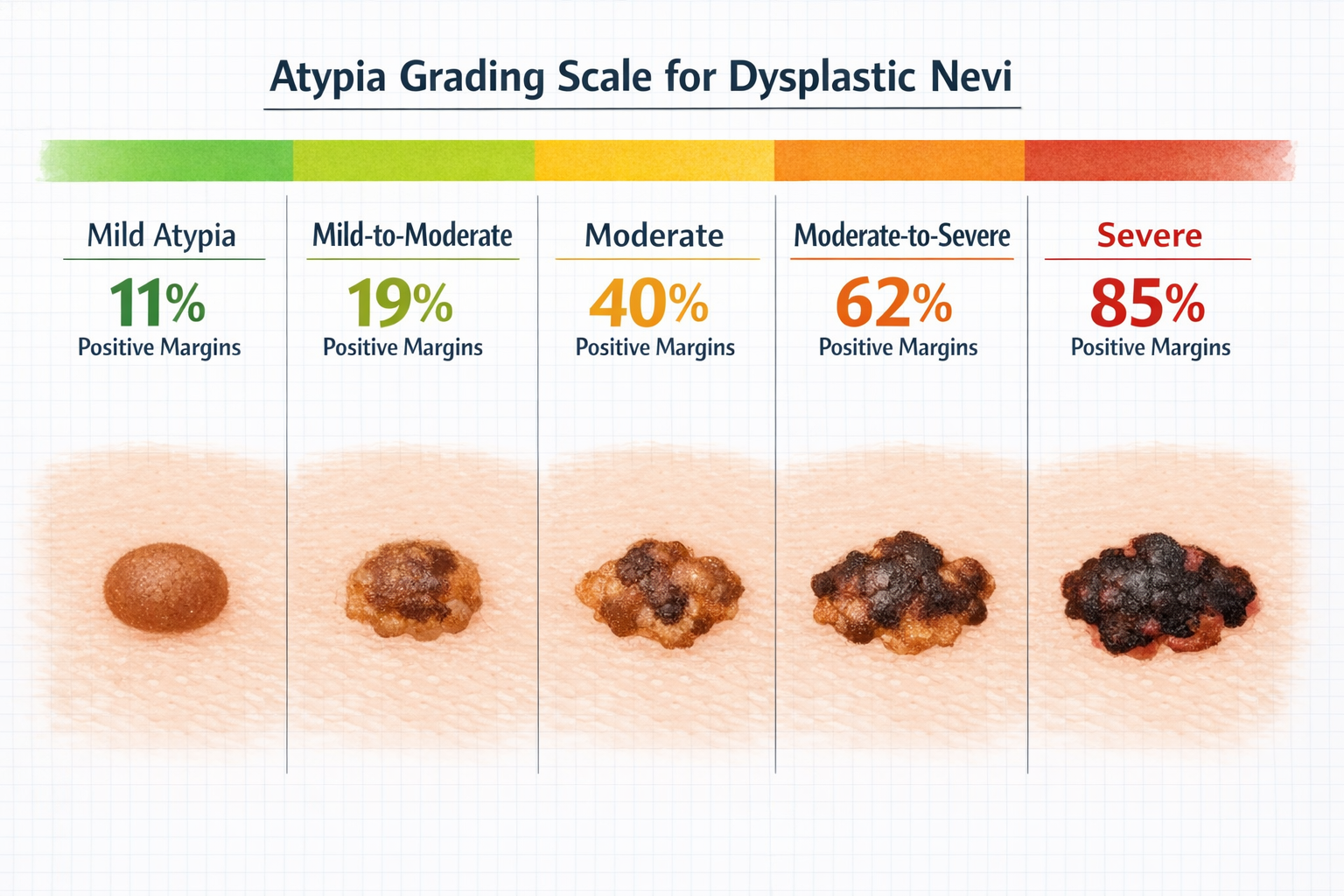
Research shows a clear relationship between how atypical a mole looks and how likely it is to have positive margins after biopsy [1]:
Atypia GradePositive Margin RateMild11%Mild-to-Moderate19%Moderate40%Moderate-to-Severe62%Severe85%
Source: JAMA Dermatology [1]
As the table shows, the more abnormal the cells appear, the more likely it is that they extend to the specimen's edge. Severely atypical moles have positive margins 85% of the time, which is one reason pathologists and surgeons take severe atypia very seriously.
The next step depends on the grade of atypia (explained in detail below) and whether there is any visible residual lesion at the biopsy site:
The frequency of re-excision after positive margins varies widely [1]:
Atypia GradeRe-Excision RateMild12%Mild-to-Moderate53%Moderate63%Moderate-to-Severe—Severe82%
The greatest management variability (meaning doctors disagree most about what to do) occurs with mildly-to-moderate and moderate dysplastic nevi [1]. This is why understanding the report and having a thorough conversation with the treating physician is so important.
Here is a reassuring fact: among dysplastic nevi with positive margins that underwent surgical re-excision, only 33% showed residual nevus (leftover mole tissue) in the re-excision specimen [1]. In other words, two-thirds of the time, the re-excision found nothing abnormal remaining. Furthermore, margin positivity and atypia grade were not associated with whether residual nevus was present [1].
Atypia (sometimes written as cytologic atypia or architectural atypia) is a term pathologists use to describe cells that look abnormal compared to what is expected. It does not mean cancer. It means the cells have features that deviate from normal—things like:
Pathology reports should specify the degree of melanocyte atypia on a scale from mild to severe [2]. This grading is critical because it directly influences treatment decisions.
GradeWhat It Means in Plain EnglishClinical SignificanceMildCells look slightly different from normal. Minor irregularities.Low concern. Usually no re-excision needed [2].Mild-to-ModerateCells show a bit more irregularity but are still far from cancerous.Low-to-moderate concern. Management varies [1].ModerateCells have noticeable abnormalities in size, shape, or organization.Moderate concern. Observation may be reasonable for positive margins [3].Moderate-to-SevereCells are significantly abnormal. Approaching the boundary of pre-cancer.Higher concern. Carries clinically significant lifetime melanoma transformation risk [1].SevereCells are very abnormal. Difficult to distinguish from melanoma in situ under the microscope.High concern. Re-excision with 2-mm margins recommended [2].
Reports may mention two types of atypia:
Both types contribute to the overall atypia grade. A mole can have mild cytologic atypia but moderate architectural atypia, or vice versa.
The atypia grade is arguably the single most important piece of information on a dysplastic nevus pathology report because it drives every downstream decision:
Understanding the different types of skin lesions and how they are classified can provide valuable context. A comprehensive overview is available in this guide to 25 types of skin lesions explained.
A dysplastic nevus (plural: dysplastic nevi) is a mole that has atypical features when examined under the microscope. Clinically, it may look like a regular mole or it may appear slightly irregular in color, shape, or border. The key distinction is that the diagnosis of "dysplastic nevus" is a microscopic diagnosis—it is made by the pathologist, not by the naked eye [5].
Common clinical features of dysplastic nevi include:
For a thorough deep dive into the clinical and pathological characteristics of atypical moles, visit this detailed resource on dysplastic nevus explained.
This is the question that causes the most anxiety: Is a dysplastic nevus the same as melanoma?
No. A dysplastic nevus is not melanoma. However, the relationship between the two is nuanced:
💡 Bottom line: Most dysplastic nevi will never become melanoma. But severely atypical ones deserve respect and close follow-up.
One of the most reassuring findings from research is that only 1.6% of cases (2 out of 127) showed a clinically significant diagnosis change upon re-excision—upgrading from a moderately-to-severely dysplastic nevus to melanoma in situ [1]. This is rare, but it underscores why severely atypical moles are treated aggressively.
Additionally, of the 27 melanomas that were found to be associated with dysplastic nevi, 96% (26 of 27) were 1 mm or less in depth [1]. This means that even in the uncommon scenario where a dysplastic nevus is associated with melanoma, the melanoma tends to be caught very early—at a stage where outcomes are excellent.
For those who want to understand what a benign mole looks like and how it differs from an atypical one, that resource provides helpful comparisons.
Below is an A-to-Z glossary of terms commonly found on pathology reports related to moles, dysplastic nevi, and skin biopsies. Each term is explained in plain, accessible language.
Architectural disorder / Architectural atypia The way cells are organized within the tissue looks abnormal. Instead of neat, orderly nests, the melanocytes (pigment cells) are arranged in irregular, disorganized patterns.
Atypia Cells that look abnormal under the microscope. Graded from mild to severe. Does not mean cancer by itself. See the detailed section above.
Atypical melanocytic proliferation A general term meaning there is an abnormal growth of melanocytes (pigment-producing cells). The pathologist may use this phrase when the findings are difficult to classify precisely.
Benign Not cancerous. A benign lesion will not spread to other parts of the body. Most moles are benign.
Biopsy The procedure of removing a small piece of tissue (or the entire lesion) for examination under a microscope. Types include:
Breslow depth (relevant if melanoma is found) The thickness of a melanoma measured in millimeters from the top of the skin (epidermis) down to the deepest point of tumor invasion. Thinner is better [6][7].
Clark level (relevant if melanoma is found) A system that describes how deeply melanoma has invaded into the layers of the skin (epidermis, papillary dermis, reticular dermis, subcutaneous fat) [6].
Clear margins See Negative margins below.
Compound nevus A mole that has melanocyte nests in both the epidermis (top layer of skin) and the dermis (deeper layer). This is a normal type of mole and is usually benign.
Cytologic atypia Abnormalities seen in individual cells—such as enlarged nuclei, irregular nuclear shapes, or abnormal pigment distribution.
Deep margin The bottom edge of the tissue specimen. A "negative deep margin" means no abnormal cells reach the bottom of the specimen.
Dermal Relating to the dermis, the thick layer of skin beneath the epidermis. "Dermal melanocytes" are pigment cells located in this deeper layer.
Dysplasia A general term for abnormal cell growth. In the context of skin, it usually refers to atypical changes in melanocytes. Not cancer, but a step beyond completely normal.
Dysplastic nevus An atypical mole with microscopic features of dysplasia. See the detailed section above. For related conditions that may appear on pathology reports, learn about Bowen's disease, a form of squamous cell carcinoma in situ.
Epidermis The outermost layer of skin. Many early changes in moles occur here.
Excision Surgical removal of a lesion, typically with a surrounding margin of normal tissue.
Excisional margins The edges of the surgically removed tissue. See Margins above.
Free margins Another term for negative margins—no abnormal cells at the edge of the specimen.
Gross description The pathologist's description of the tissue specimen as seen with the naked eye (without a microscope). Includes size, shape, color, and texture.
Histologic Relating to the microscopic study of tissue. "Histologic examination" means looking at tissue under a microscope.
Hyperplasia An increase in the number of cells in a tissue. Not the same as dysplasia or cancer, but it indicates the tissue is more active than normal.
In situ Latin for "in place." When used in pathology (e.g., "melanoma in situ"), it means the abnormal cells are confined to their original location and have not invaded deeper tissues. This is the earliest, most treatable stage [6].
Intradermal nevus A mole where melanocyte nests are located entirely within the dermis (not in the epidermis). These are usually mature, benign moles.
Junctional nevus A mole where melanocyte nests are located at the junction between the epidermis and dermis (the dermal-epidermal junction). These are flat moles and are usually benign.
Lateral margin The side edges of the tissue specimen (as opposed to the deep/bottom margin).
Lentiginous A growth pattern where melanocytes are arranged in a single-cell pattern along the basal layer of the epidermis. "Lentiginous melanocytic hyperplasia" means there are more melanocytes than usual arranged in this pattern.
Lesion A general medical term for any abnormal area of tissue. A mole, a rash, a cyst—all are "lesions."
Malignant Cancerous. A malignant lesion has the ability to invade surrounding tissues and potentially spread (metastasize) to other parts of the body.
Margins The edges of the removed tissue specimen. See the detailed section above.
Melanocyte A cell that produces melanin, the pigment that gives skin, hair, and eyes their color. Moles are clusters of melanocytes. Melanoma is a cancer of melanocytes.
Melanoma in situ The earliest form of melanoma, confined to the epidermis. Has not invaded the dermis. Highly curable with appropriate excision [6].
Mitotic rate / Mitotic figures The number of cells actively dividing. A higher mitotic rate may suggest a more aggressive process. In melanoma pathology, this is an important prognostic factor [6].
Negative margins ✅ No abnormal cells at the edge of the specimen. The lesion appears to have been completely removed. This is the desired outcome [6].
Nevus (plural: nevi) The medical term for a mole. A nevus is a benign growth of melanocytes.
Pagetoid spread Melanocytes that have migrated upward into the upper layers of the epidermis. This pattern can be seen in melanoma but can also occur in benign conditions. Context matters.
Peripheral margin Same as lateral margin—the side edges of the specimen.
Positive margins ⚠️ Abnormal cells extend to the edge of the specimen, suggesting the removal may have been incomplete [6].
Re-excision A second surgical procedure to remove additional tissue around the original biopsy site. Done when margins are positive or when a more serious diagnosis (like melanoma) requires wider margins.
Residual nevus Leftover mole tissue found in a re-excision specimen. Present in about 33% of re-excisions for dysplastic nevi with positive margins [1].
Sentinel lymph node biopsy (relevant for invasive melanoma) A procedure to check whether melanoma has spread to the nearest lymph node. Not relevant for dysplastic nevi but may appear on reports if melanoma is diagnosed [7].
Shave biopsy A technique where the doctor uses a blade to shave off the top portion of a skin lesion. Because it does not go as deep as an excision, the deep margin may not be assessable.
Specimen The piece of tissue that was removed and sent to the pathology lab.
Spindle cells Elongated, spindle-shaped cells. Can be seen in certain types of nevi (like Spitz nevi) and some melanomas.
Transection When a pathologist says a lesion is "transected" at the margin, it means the lesion is cut through at the edge—essentially the same as a positive margin.
Ulceration Loss of the surface skin (epidermis) over a lesion. In melanoma, ulceration is a negative prognostic factor [6].
Vertical growth phase In melanoma, this refers to the tumor growing downward into the dermis. This is more concerning than radial (horizontal) growth.
Reading a pathology report does not have to be overwhelming. Here is a simple, step-by-step approach:
Skip to the "Diagnosis" section. This is the bottom line. It will say something like:
Look for words like mild, moderate, severe, or combinations (mild-to-moderate, moderate-to-severe). This tells how abnormal the cells look and directly influences the next steps [2].
Look for language about margins:
The pathologist may include recommendations such as:
The pathology report is a tool for the treating physician. Always discuss the findings, the atypia grade, the margin status, and the recommended plan of action during a follow-up appointment.
For patients concerned about suspicious moles or early warning signs, this resource on early-stage skin cancer provides additional context on what to watch for.
One of the most common questions after receiving a pathology report with a dysplastic nevus diagnosis is: "Do I need more surgery?"
The answer depends on several factors. Here is a simplified decision framework based on current evidence:
Understanding the relationship between dysplastic nevi and melanoma helps reduce unnecessary anxiety while maintaining appropriate vigilance.
FactDataAssociation rate between dysplastic nevi and invasive melanoma11% [1]Melanomas arising de novo (not from a pre-existing mole)~71% [3]Diagnosis upgrade upon re-excision (dysplastic nevus → melanoma in situ)1.6% (2 of 127 cases) [1]Depth of melanomas associated with dysplastic nevi (≤1 mm)96% (26 of 27) [1]Lifetime transformation risk for mildly atypical neviSimilar to typical moles [1]Lifetime transformation risk for severely atypical neviClinically significant [1]
For patients who want to understand the UV exposure connection and how to protect their skin proactively, the complete UV index guide is an excellent resource.
A: No. A dysplastic nevus is an atypical mole, not cancer. Most dysplastic nevi are benign and will never become melanoma [5]. The atypia grade on the report indicates how abnormal the cells look, and the treating physician will determine whether any further action is needed.
A: Not at all. Positive margins are common, especially with shave biopsies, and they do not indicate an error. Approximately 34% of dysplastic nevi have positive margins after biopsy [1]. The initial biopsy is designed to get a diagnosis; if re-excision is needed, it is a planned next step, not a correction of a mistake.
A: It depends on the atypia grade and margin status. Mildly atypical moles with positive margins usually just need monitoring [2]. Severely atypical moles with positive margins typically require re-excision with 2-mm margins [2]. Moderately atypical moles fall in between, and the decision is made on a case-by-case basis [3].
A: At minimum, annually. Patients with multiple dysplastic nevi, a personal or family history of melanoma, or severely atypical moles may need checks every 3 to 6 months. The treating physician will recommend an appropriate schedule.
A: Yes, it is possible. Among re-excisions for positive margins, about 33% show residual nevus tissue [1]. This is why follow-up monitoring of the biopsy site is important, especially in the first year [2].
A: Vigilance, not panic. Having one dysplastic nevus does not mean all moles are dangerous. However, it is a good reminder to perform regular self-examinations and to have a dermatologist or qualified physician evaluate any moles that change in size, shape, color, or symptoms. Learn more about what to look for in clear moles and other common mole types.
Bringing a list of questions to the follow-up appointment can make the conversation more productive. Here are suggested questions:
ScenarioTypical ActionEvidenceMild atypia, negative marginsNo further treatment; routine follow-up[2]Mild atypia, positive margins, no residual lesionMonitor for 1 year; return for changes[2]Moderate atypia, negative marginsNo further treatment; routine follow-up[3]Moderate atypia, positive marginsObservation may be reasonable; discuss with physician[3]Severe atypia, negative marginsNo re-excision; closer follow-up recommended[2]Severe atypia, positive marginsRe-excision with 2-mm margins[2]Any grade with clinical concern for melanomaUrgent excision and further workup[6][7]
Receiving a pathology report with terms like "dysplastic nevus," "atypia," and "positive margins" can feel alarming—but knowledge is the best antidote to fear. This guide has broken down the pathology report explained in plain English: margins, atypia, and dysplastic nevus are not mysteries when the language is translated into everyday words.
Here are actionable next steps to take in 2026:
A pathology report is not a verdict—it is a roadmap. With the right understanding and a trusted medical team, every patient can navigate it with confidence. For comprehensive skin care and expert evaluation, visit The Minor Surgery Center to learn about available services and specialist consultations.
[1] jamanetwork - https://jamanetwork.com/journals/jamadermatology/fullarticle/1695326
[2] Standard Classification Of Dysplastic Nevi - https://www.clinicaladvisor.com/features/standard-classification-of-dysplastic-nevi/
[3] practicaldermatology - https://practicaldermatology.com/topics/skin-cancer-photoprotection/assessing-clinical-options-for-moderately-dysplastic-nevi-excised-with-positive-margins/20322/
[4] Dysplastic Nevus Mild Moderate Atypia - https://www.flderms.com/path-results/dysplastic-nevus-mild-moderate-atypia
[5] 24841 Dysplastic Nevus Atypical Moles - https://my.clevelandclinic.org/health/diseases/24841-dysplastic-nevus-atypical-moles
[6] Understanding Your Pathology - https://www.aimatmelanoma.org/melanoma-101/newly-diagnosed/understanding-your-pathology/
[7] Get Educated - https://www.curemelanoma.org/patient-eng/ten-tips-for-people-just-diagnosed-with-melanoma/get-educated
[8] Mole And Dysplastic Nevi Treatment - https://dermatologyoffice.com/surgical/mole-and-dysplastic-nevi-treatment/
[9] Diagnosing Irregular Darkly Pigmented Lesion Dorsolateral Forefoot Patient Previous Skin Cancer - https://www.hmpgloballearningnetwork.com/site/podiatry/diagnosing-irregular-darkly-pigmented-lesion-dorsolateral-forefoot-patient-previous-skin-cancer