You notice a throbbing pain around your fingernail. The skin looks red, swollen, and tender to the touch. Within hours, what started as minor discomfort has become a painful, pulsing problem that makes typing, cooking, or even holding a coffee cup uncomfortable. This common yet frustrating condition—paronychia explained simply—is a nail infection affecting thousands of people every day, and understanding it is your first step toward relief.
Paronychia is more than just an annoying nail issue. It's a skin infection that targets the delicate tissue surrounding your fingernails or toenails, specifically the nail folds where skin meets nail. Whether you're a busy professional who types all day, a healthcare worker washing hands constantly, or someone who simply trimmed their cuticles a bit too aggressively, paronychia can disrupt your daily routine and cause significant discomfort.
The good news? With proper understanding and timely treatment, most cases of paronychia resolve completely, allowing you to get back to your life without lingering complications.
Paronychia is a skin infection that develops in the tissue immediately surrounding your fingernails or toenails. The name comes from the Greek words "para" (beside) and "onyx" (nail), which perfectly describes where this condition occurs.
Think of your nail as being framed by protective skin tissue called the nail fold. This includes the lateral nail folds (the skin on the sides of your nail) and the proximal nail fold (the skin at the base of your nail where your cuticle sits). These areas create a seal that protects the nail bed and nail matrix—the growing part of your nail—from infection and injury.
When this protective barrier becomes compromised through trauma, irritation, or moisture exposure, bacteria, fungi, or yeast can enter and cause infection. The result is inflammation, swelling, pain, and potentially pus formation in the affected area.
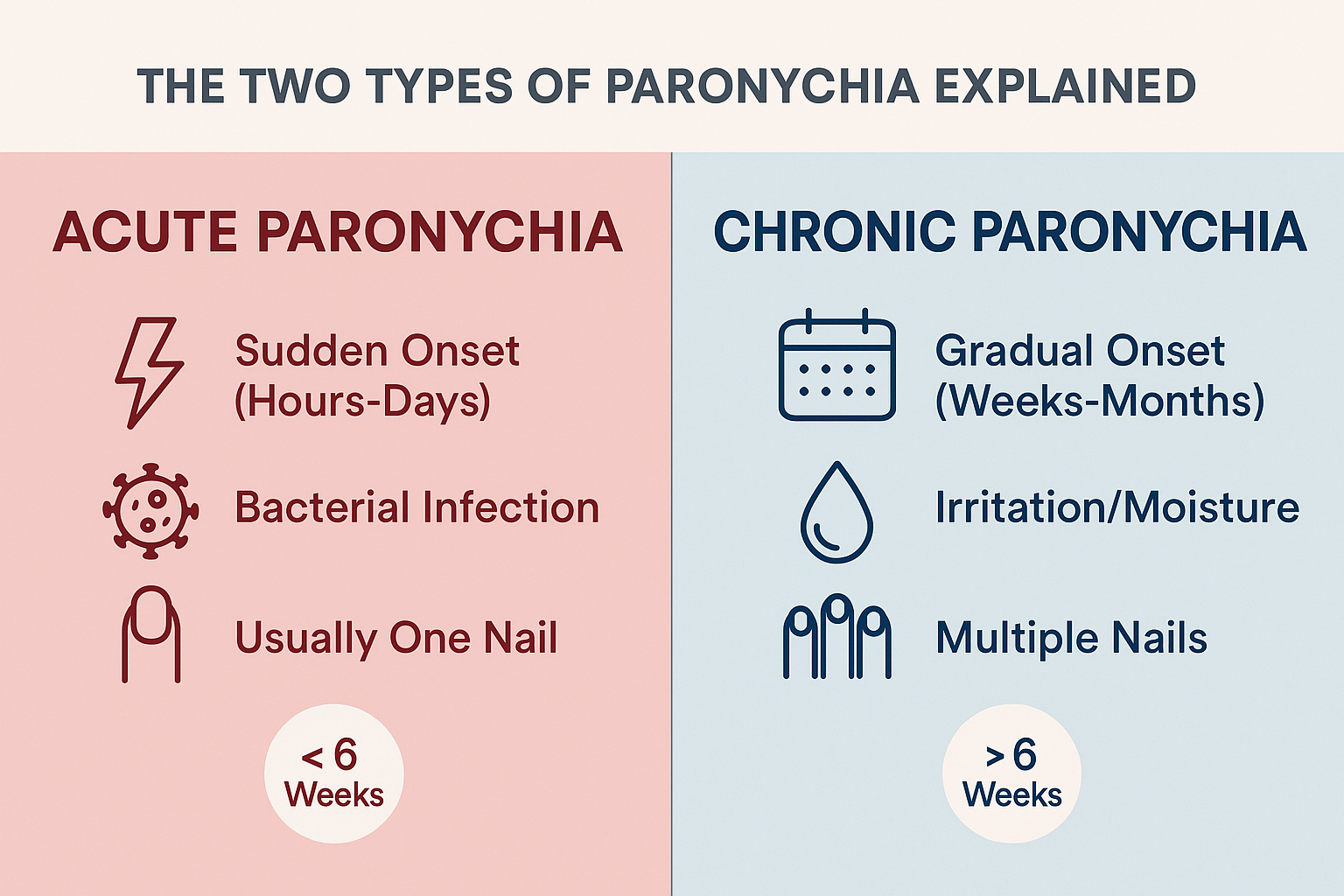
Understanding the difference between acute and chronic paronychia is crucial because they have different causes, symptoms, and treatment approaches.
Acute paronychia develops suddenly and progresses rapidly. You might notice symptoms appearing within hours to a few days after the initial trigger. This type typically affects a single nail and is almost always caused by bacterial infection, most commonly Staphylococcus aureus [1].
Chronic paronychia develops slowly over weeks or months and often affects multiple nails simultaneously. This type is usually not a true infection but rather an inflammatory reaction to repeated irritation, moisture, or chemical exposure. However, fungal organisms like Candida albicans may colonize the damaged tissue [2].
The six-week timeline is the medical dividing line: if your symptoms persist longer than six weeks, you're dealing with chronic paronychia rather than acute.
For a deeper understanding of the differences between these two forms, you can explore our detailed comparison on acute vs chronic paronychia.
Knowing what to look for helps you identify paronychia early, when treatment is most effective and complications are least likely.
Acute paronychia announces itself dramatically. The symptoms develop quickly and are hard to ignore:
Pain and Tenderness 💢
The affected area becomes intensely painful, often with a throbbing sensation that worsens with pressure or when your hand hangs down. The pain can be severe enough to interfere with sleep or daily activities.
Redness and Warmth 🔴
The skin around the nail becomes noticeably red and feels warm to the touch. This warmth indicates active inflammation and increased blood flow to the area as your body fights the infection.
Swelling 🫧
Significant swelling develops rapidly around the nail fold. The tissue may appear puffy and tense, and the normal contours of your finger may be obscured.
Pus Formation 💧
Within 24-48 hours, you may notice a yellowish or whitish collection of pus forming under the skin adjacent to the nail or beneath the nail itself. This abscess formation is a hallmark of acute bacterial paronychia.
Single Nail Involvement
Acute paronychia typically affects only one nail—usually the nail that experienced recent trauma or injury.
Chronic paronychia is subtler and develops gradually over weeks or months:
Mild Tenderness
Rather than severe pain, chronic paronychia causes mild, persistent tenderness around the nail. The discomfort is usually tolerable but annoying.
Minimal Swelling
The nail fold appears slightly puffy or boggy rather than dramatically swollen. The tissue may feel soft and spongy to the touch.
Missing or Damaged Cuticles ✂️
One of the most characteristic signs of chronic paronychia is the absence of the cuticle. The protective seal at the base of the nail is lost, leaving the nail matrix vulnerable to irritants and organisms.
Moist, Boggy Skin
The skin around the nail may appear moist, wrinkled, or macerated (softened by moisture). It may peel easily or appear whitish.
Nail Changes
Over time, chronic paronychia causes visible changes to the nail itself:
Multiple Nail Involvement
Chronic paronychia often affects several nails at once, particularly on the dominant hand or on hands frequently exposed to moisture or irritants.
While most paronychia cases remain localized, certain symptoms indicate the infection may be spreading and requires immediate medical attention:
If you experience any of these systemic symptoms, seek prompt medical care. At The Minor Surgery Center, our experienced surgical team provides expert outpatient care for complicated paronychia cases that require professional intervention.
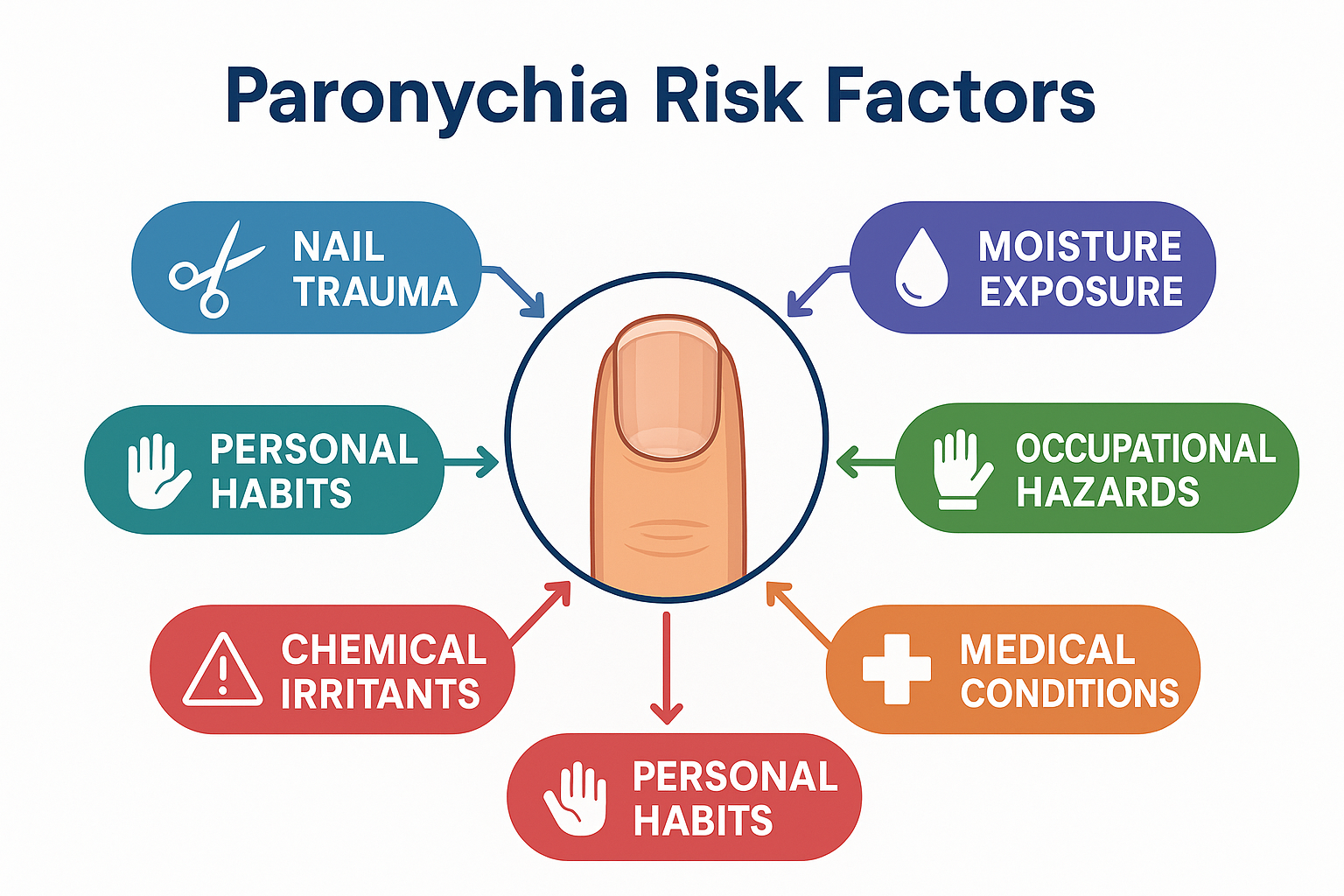
Paronychia doesn't appear randomly. Specific triggers and risk factors create the conditions for infection or inflammation to develop.
Acute paronychia almost always begins with a break in the protective skin barrier around the nail, followed by bacterial invasion.
Common Triggers Include:
Nail Trauma 🔨
Bacterial Entry
Once the skin barrier is breached, bacteria—particularly Staphylococcus aureus—enter the tissue and multiply rapidly. Other bacteria that can cause acute paronychia include Streptococcus species and, less commonly, Pseudomonas aeruginosa [3].
Ingrown Nails
When a nail grows into the surrounding skin, it creates a wound that becomes an entry point for bacteria.
Manicure or Pedicure Complications
Professional nail services that are too aggressive or use non-sterile equipment can introduce bacteria while damaging the protective cuticle seal.
Chronic paronychia has different underlying causes, primarily related to repeated irritation rather than acute infection.
Moisture Exposure 💧
Prolonged or frequent contact with water is the single most important risk factor for chronic paronychia. Water softens and breaks down the cuticle, allowing irritants and organisms to penetrate.
Occupational Risks
Certain professions significantly increase chronic paronychia risk:
Chemical Irritants 🧪
Regular exposure to harsh chemicals damages the protective nail fold:
Fungal and Yeast Colonization
While not the primary cause, Candida albicans (a yeast) often colonizes chronically inflamed nail folds, contributing to ongoing inflammation and preventing healing.
Medical Conditions
Certain health conditions increase susceptibility to chronic paronychia:
Medications 💊
Some medications increase chronic paronychia risk:
Contact Dermatitis
Allergic reactions to substances touching the nail area can cause chronic inflammation. Learn more about contact dermatitis explained and how it relates to nail problems.
Beyond occupational and medical factors, certain personal habits make paronychia more likely:
Diagnosing paronychia is usually straightforward, based primarily on visual examination and your medical history. However, proper diagnosis is essential to ensure appropriate treatment and rule out other conditions.
A healthcare provider will examine the affected nail and surrounding tissue, looking for characteristic signs:
Your provider will ask specific questions to determine the type and cause:
In most cases of acute paronychia, no laboratory testing is needed. However, testing may be ordered when:
Culture and Sensitivity
If pus is present, your provider may collect a sample to identify the specific bacteria or fungus causing infection and determine which antibiotics will be most effective. This is particularly important if:
Fungal Testing
For chronic paronychia, testing for fungal organisms (particularly Candida species) helps guide treatment. This may include:
Blood Tests
If systemic infection is suspected (fever, spreading redness, severe symptoms), blood tests may include:
Your provider will also consider other conditions that can mimic paronychia:
Understanding various types of skin lesions can help you recognize when a nail problem might be something other than paronychia.
Treatment for paronychia depends on whether you're dealing with acute or chronic type, the severity of symptoms, and whether complications have developed.
Early-Stage Treatment (No Abscess)
If you catch acute paronychia in its earliest stages—before pus formation—conservative home treatment may be sufficient:
Warm Water Soaks 🛁
Soak the affected finger in warm water for 15-20 minutes, three to four times daily. This increases blood flow, reduces pain, and may help the infection resolve without further intervention.
Add Epsom salts (magnesium sulfate) to enhance the soak's effectiveness. The warmth and salt help draw out infection and reduce inflammation.
Elevation
Keep your hand elevated above heart level when possible to reduce throbbing pain and swelling.
Topical Antibiotics
Over-the-counter antibiotic ointments like bacitracin or mupirocin applied to the affected area may help prevent bacterial growth.
Pain Management 💊
Over-the-counter pain relievers like ibuprofen or acetaminophen reduce pain and inflammation.
Advanced Treatment (Abscess Present)
Once an abscess forms—indicated by a visible collection of pus—drainage becomes necessary. This is not a do-it-yourself situation.
Incision and Drainage
A healthcare provider will:
This procedure provides immediate pain relief and allows the infection to heal. At The Minor Surgery Center, our experienced surgical team performs these procedures with a comfort-first approach, ensuring safe and efficient surgery with minimal discomfort.
Oral Antibiotics
After drainage, or if infection is extensive, oral antibiotics are prescribed. Common choices include:
The typical course is 7-10 days, and it's crucial to complete the entire prescription even if symptoms improve quickly.
Partial Nail Removal
If infection extends under the nail or if an ingrown nail caused the problem, partial nail removal may be necessary. This allows proper drainage and healing of the nail bed.
Chronic paronychia requires a different approach focused on eliminating irritants and protecting the nail fold.
Moisture Avoidance 💧
This is the single most important treatment step:
Irritant Avoidance
Identify and eliminate contact with chemical irritants:
Topical Corticosteroids
Medium to high-potency topical steroid creams (like triamcinolone or betamethasone) reduce inflammation. Apply twice daily to the affected nail folds for several weeks.
Topical Antifungals 🍄
If Candida colonization is present, antifungal creams or solutions (like clotrimazole, ketoconazole, or ciclopirox) are applied to the nail folds twice daily.
Topical Calcineurin Inhibitors
For cases that don't respond to steroids, tacrolimus ointment provides anti-inflammatory effects without steroid side effects.
Oral Antifungals
Severe or resistant chronic paronychia may require oral antifungal medications:
These are typically prescribed for 6-12 weeks and require monitoring for potential side effects.
Surgical Treatment
For chronic paronychia that doesn't respond to conservative treatment, surgical options include:
En Bloc Excision of Proximal Nail Fold
This procedure removes the chronically inflamed nail fold tissue, allowing healthy tissue to regenerate. It's particularly effective for cases involving the base of the nail.
Eponychial Marsupialization
The surgeon creates a permanent opening in the nail fold to improve drainage and prevent moisture accumulation.
These procedures are performed under local anesthesia as outpatient surgeries. Our team provides personalized treatment plans tailored to your specific situation, ensuring you receive the most appropriate care for your condition.
Acute Paronychia:
Chronic Paronychia:
Prevention is far easier than treatment when it comes to paronychia. These evidence-based strategies significantly reduce your risk.
Nail Care Best Practices ✂️
Hand Hygiene Without Overdoing It 🧼
Protective Measures
Avoid Nail Trauma
Be mindful during activities that could injure your nails:
Treat Minor Injuries Promptly
If you do injure the skin around your nail:
Choose Safe Manicure Practices
Occupational Modifications 👷
If your job involves frequent water or chemical exposure:
Moisture Management
Identify and Avoid Allergens
If you suspect allergic contact dermatitis contributes to your nail fold inflammation:
Medical Management
If you have diabetes or other conditions affecting immune function:
For People with Diabetes 🩺
Diabetes increases both infection risk and healing complications:
For Immunocompromised Individuals
If you have HIV, cancer, or take immunosuppressive medications:
For Healthcare Workers
Frequent handwashing is non-negotiable in healthcare, but you can still protect your nails:
While paronychia may seem like a minor problem, untreated or inadequately treated cases can lead to serious complications.
Permanent Nail Damage 💅
Chronic or severe paronychia can permanently alter nail growth:
The nail matrix (growth center) can be damaged by prolonged inflammation or infection, resulting in permanent changes to how the nail grows.
Nail Bed Infection (Onychia)
Infection can spread from the nail fold to the nail bed itself, causing:
Abscess Formation
Untreated acute paronychia almost always progresses to abscess formation, which requires surgical drainage. Delaying drainage prolongs pain and increases the risk of spread.
Felon
If infection spreads to the pulp space (the fleshy pad) of the fingertip, a felon develops. This is a serious, deep infection requiring:
Cellulitis 🔴
Bacterial infection can spread beyond the nail fold into surrounding skin and soft tissue, causing:
Osteomyelitis
In rare cases, particularly in people with diabetes or immunosuppression, infection can spread to the bone of the finger or toe. Osteomyelitis is a serious condition requiring:
Sepsis
Although uncommon, paronychia can lead to bloodstream infection (septicemia) and sepsis, particularly in immunocompromised individuals. This life-threatening condition requires:
Tenosynovitis
Infection can spread to the tendon sheaths in the finger, causing:
Beyond medical complications, untreated paronychia affects daily function:
These functional impacts underscore why timely, appropriate treatment is essential. Don't wait for a minor nail problem to become a major health issue.
Knowing when to see a healthcare provider versus managing paronychia at home can prevent complications and ensure optimal outcomes.
🚨 Emergency Warning Signs:
📅 Non-Emergency Situations Requiring Professional Evaluation:
If you fall into any of these categories, don't wait to see if symptoms resolve on their own:
For these individuals, even mild paronychia can progress rapidly to serious complications.
When you visit a healthcare provider for paronychia, the appointment typically includes:
Examination
Visual inspection of the affected nail and surrounding tissue, assessment of severity, and evaluation for complications.
Discussion
Questions about symptom onset, duration, occupation, medical history, and previous treatments attempted.
Treatment
Depending on severity, this may include:
Follow-Up
Your provider will schedule a follow-up visit if needed to ensure proper healing and address any complications.
At The Minor Surgery Center, we understand that nail infections can be painful and disruptive. Our experienced surgical team provides expert outpatient care with a comfort-first approach, ensuring you receive personalized treatment plans tailored to your specific needs. We specialize in minimally invasive solutions that help you get back to your life quickly and safely.
For some individuals, particularly those in high-risk occupations or with underlying medical conditions, chronic paronychia becomes a recurring challenge requiring ongoing management.
Occupational Adjustments 💼
If your job contributes to chronic paronychia, consider:
Home Life Modifications 🏠
Some individuals benefit from ongoing preventive treatment:
Intermittent Topical Therapy
Applying topical corticosteroids or antifungals 1-2 times weekly (even when asymptomatic) may prevent flare-ups in susceptible individuals.
Regular Moisturization
Daily application of thick, fragrance-free moisturizers maintains skin barrier integrity and prevents cracking.
Nail Care Routine
Establish a gentle nail care routine:
Regular Self-Inspection 🔍
Check your nails daily for:
Scheduled Provider Visits
For chronic or recurrent cases, regular follow-up appointments allow your healthcare provider to:
Chronic paronychia can affect mental health and quality of life:
Don't hesitate to discuss these concerns with your healthcare provider. Support groups, counseling, or adjustments to your treatment plan may help address the psychological burden of chronic conditions.
While chronic paronychia can be challenging, many people successfully manage the condition with:
Remember: improvement is measured in weeks and months, not days. Nail appearance may take 3-6 months to normalize as healthy nail grows out to replace damaged nail. Persistence with prevention and treatment strategies pays off.
Certain groups face unique challenges with paronychia and require tailored approaches.
Common Causes in Children:
Treatment Considerations:
Prevention Strategies:
Considerations:
Safe Treatment Options:
Always inform your healthcare provider if you're pregnant or planning to become pregnant.
Unique Risk Factors:
Management Strategies:
Diabetes significantly increases both the risk and severity of paronychia:
Why Diabetes Increases Risk:
Special Precautions:
Treatment Modifications:
People with HIV, cancer, organ transplants, or those taking immunosuppressive medications face heightened risks:
Increased Complications:
Modified Treatment Approach:

Several conditions can mimic paronychia or occur alongside it. Understanding the differences helps ensure accurate diagnosis and appropriate treatment.
Herpetic Whitlow is a viral infection of the finger caused by herpes simplex virus (HSV).
Key Differences:
Who's at Risk:
Healthcare workers (especially dentists and respiratory therapists), people with oral or genital herpes who bite their nails or suck their thumbs.
Felon is a deep infection of the fingertip pulp (the fleshy pad).
Key Differences:
Ingrown toenails occur when the nail grows into the surrounding skin.
Similarities:
Key Differences:
Psoriasis can affect nails, causing inflammation that mimics chronic paronychia.
Key Differences:
Rarely, squamous cell carcinoma (a type of skin cancer) can present as chronic inflammation around the nail.
Warning Signs:
Action Required:
Any chronic paronychia that doesn't respond to appropriate treatment within 6-8 weeks should be biopsied to rule out malignancy.
For more information about skin cancers, explore our comprehensive guides on 4 types of skin cancer and basal cell carcinoma treatment.
Dyshidrotic eczema or hand dermatitis can affect the nail folds.
Key Differences:
While mild, early-stage paronychia may respond to home treatment, professional medical care offers significant advantages and is essential in many situations.
Accurate Diagnosis 🔬
Healthcare providers can distinguish paronychia from conditions that mimic it, ensuring you receive appropriate treatment rather than wasting time on ineffective approaches.
Appropriate Treatment Selection
Professionals determine whether you need:
Proper Drainage Technique
If an abscess is present, professional drainage offers:
Culture-Guided Therapy
When infection is severe, recurrent, or in high-risk individuals, culture and sensitivity testing identifies:
Some paronychia cases require surgical procedures beyond simple drainage:
Partial Nail Removal (Partial Nail Avulsion)
Indicated when:
The procedure involves:
Complete Nail Removal (Complete Nail Avulsion)
Rarely necessary, but indicated when:
Eponychial Marsupialization
For chronic paronychia resistant to medical management:
En Bloc Excision
For severe chronic paronychia:
At The Minor Surgery Center, we specialize in providing expert outpatient care for conditions like paronychia. Our approach offers:
Experienced Surgical Team 👨⚕️
Our surgeons have extensive experience managing both simple and complex paronychia cases, ensuring you receive the highest quality care.
Comfort-First Approach
We understand that nail procedures can be anxiety-inducing. We prioritize your comfort through:
Efficient, Convenient Service
We respect your time and schedule:
Personalized Treatment Plans 📋
We don't believe in one-size-fits-all approaches. Your treatment plan is tailored to:
Safe, Minimally Invasive Solutions
We use the most conservative approach that will effectively resolve your condition, avoiding unnecessary procedures while ensuring complete treatment.
Comprehensive Follow-Up
Your care doesn't end when the procedure is complete. We provide:
Similar to our approach for cyst excision and other minor surgical procedures, we ensure every patient receives personalized, high-quality care in a comfortable outpatient setting.
Early-stage acute paronychia without abscess formation may resolve with home treatment (warm soaks, elevation). However, once an abscess forms, drainage is necessary. Chronic paronychia rarely resolves without addressing the underlying cause (moisture exposure, irritants).
Acute paronychia typically improves within 2-3 days of appropriate treatment and resolves completely in 1-2 weeks. Chronic paronychia takes much longer—weeks to months—and requires consistent prevention strategies to prevent recurrence.
Paronychia itself is not contagious. However, the bacteria causing acute paronychia (particularly Staphylococcus aureus) can spread to others through direct contact or contaminated surfaces. Good hand hygiene prevents transmission.
No. Self-drainage carries significant risks:
Always seek professional care for abscess drainage.
Most cases of paronychia do not result in nail loss. However, severe or prolonged infection may cause:
Early, appropriate treatment minimizes the risk of permanent nail damage.
This depends on:
Mild cases may allow continued work with protective measures. Severe cases, particularly those requiring drainage, may necessitate a few days off to allow initial healing. Jobs involving food handling may require temporary reassignment until infection resolves.
Most health insurance plans cover medically necessary treatment for paronychia, including:
Coverage varies by plan, so check with your insurance provider. At The Minor Surgery Center, our staff can help verify coverage and discuss payment options.
Prevention strategies include:
Seek professional care if:
Untreated or severe paronychia can cause:
Early, appropriate treatment prevents most permanent complications.
Paronychia explained doesn't have to be complicated. Whether you're dealing with the sudden, painful onset of acute paronychia or the frustrating persistence of chronic paronychia, understanding this common nail infection empowers you to take appropriate action.
Key Points to Remember:
✅ Recognize the difference between acute and chronic paronychia—they have different causes and require different treatments
✅ Act early when symptoms appear—prompt treatment prevents complications and speeds recovery
✅ Don't attempt self-drainage of abscesses—professional care ensures safe, effective treatment with proper pain control
✅ Address underlying causes, especially moisture exposure and occupational factors, to prevent recurrence
✅ Seek professional care when symptoms are severe, persistent, or if you have risk factors like diabetes
✅ Prevention is possible through proper nail care, protective measures, and lifestyle modifications
If you're currently experiencing paronychia symptoms:
At The Minor Surgery Center, we understand that nail infections can be painful, disruptive, and concerning. Our experienced surgical team provides expert outpatient care with a comfort-first approach, offering personalized treatment plans designed to resolve your paronychia safely and efficiently.
We specialize in minimally invasive solutions that address the root cause of your condition while minimizing discomfort and recovery time. Whether you need simple drainage, comprehensive chronic paronychia management, or surgical intervention, we're here to help you get back to your life—pain-free and confident.
Don't let paronychia control your life. With the right knowledge, timely treatment, and expert care, you can overcome this common condition and prevent future episodes.
For more information about our services or to schedule a consultation, visit our website or contact our office. We serve patients throughout the Toronto area, including Ajax and Barrie, providing accessible, high-quality outpatient surgical care when you need it most.
Your nail health matters. Your comfort matters. Your ability to return to the activities you love matters. Let us partner with you in achieving optimal outcomes and lasting relief.
[1] Rigopoulos, D., Larios, G., Gregoriou, S., & Alevizos, A. (2008). Acute and chronic paronychia. American Family Physician, 77(3), 339-346.
[2] Tosti, A., Piraccini, B. M., & Ghetti, E. (2001). Chronic paronychia: a now-curable disease. Skin Therapy Letter, 6(10), 1-3.
[3] Rockwell, P. G. (2001). Acute and chronic paronychia. American Family Physician, 63(6), 1113-1116.
[4] Shafritz, A. B., & Coppage, J. M. (2014). Acute and chronic paronychia of the hand. Journal of the American Academy of Orthopaedic Surgeons, 22(3), 165-174.
[5] Wollina, U. (2001). Acute paronychia: comparative treatment with topical antibiotic alone or in combination with corticosteroid. Journal of the European Academy of Dermatology and Venereology, 15(1), 82-84.
[6] Daniel, C. R., & Scher, R. K. (2004). Nail changes secondary to systemic drugs or ingestants. Journal of the American Academy of Dermatology, 50(2), 229-246.
[7] Tosti, A., Piraccini, B. M., Ghetti, E., & Colombo, M. D. (2002). Topical steroids versus systemic antifungals in the treatment of chronic paronychia: an open, randomized double-blind and double dummy study. Journal of the American Academy of Dermatology, 47(1), 73-76.
[8] Haneke, E., & Baran, R. (2011). Longitudinal melanonychia. Dermatologic Surgery, 27(6), 580-584.
[9] Leggit, J. C. (2017). Acute and chronic paronychia. American Family Physician, 96(1), 44-51.
[10] Relhan, V., Goel, K., Bansal, S., & Garg, V. K. (2014). Management of chronic paronychia. Indian Journal of Dermatology, 59(1), 15-20.