Have you ever noticed painful redness and swelling around your fingernail or toenail that just won't go away? You're not alone. Paronychia—an infection of the skin around the nail—is one of the most common hand infections, affecting millions of people every year. But here's what many don't realize: not all paronychia infections are created equal. Understanding whether you're dealing with acute or chronic paronychia can mean the difference between quick relief and months of frustration.
Paronychia might seem like a minor annoyance at first, but without proper treatment, it can lead to serious complications, including permanent nail damage or spread of infection. The good news? When you know what you're dealing with, treatment is straightforward and effective.
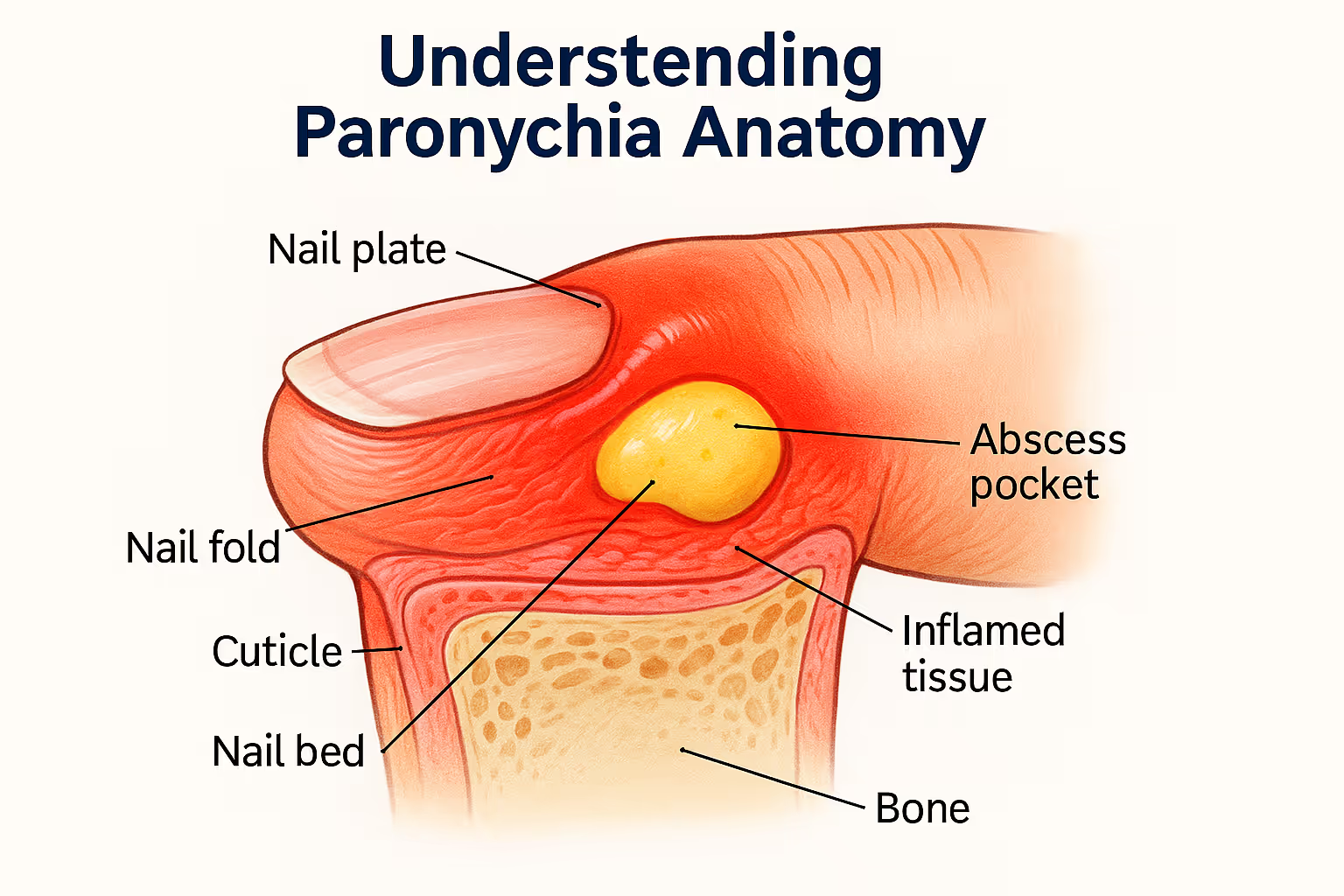
Paronychia is an infection of the nail fold—the soft tissue that frames and supports your nail on three sides. Think of the nail fold as a protective border that keeps your nail bed healthy and secure. When this area becomes infected or inflamed, you'll experience pain, swelling, redness, and sometimes pus formation around the nail.
The condition can affect fingernails or toenails, though fingernails are more commonly involved. What makes paronychia particularly troublesome is its location: your hands are constantly in use, making rest and healing challenging.
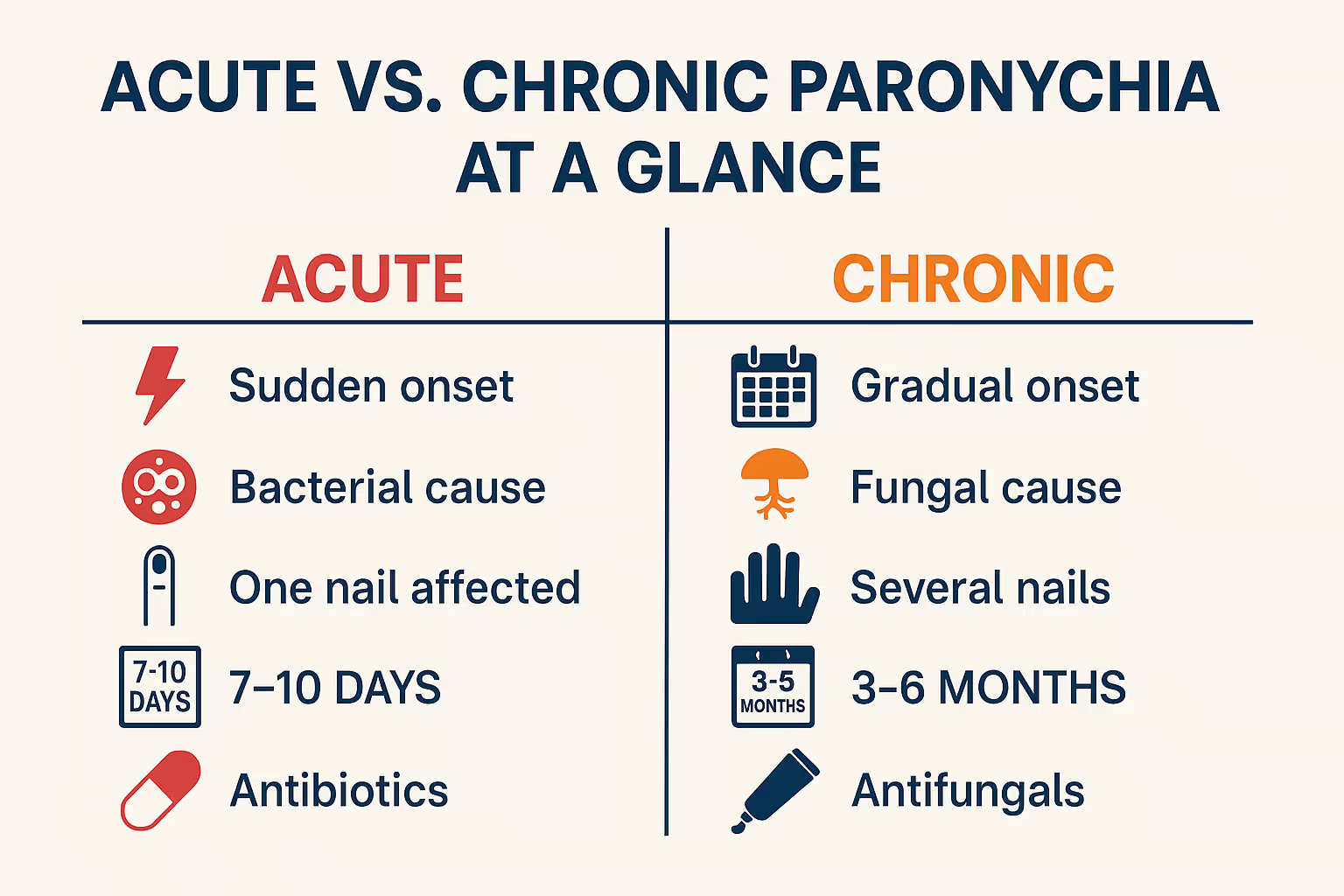
The medical community divides paronychia into two distinct categories based on how quickly symptoms develop and how long they persist:
Acute Paronychia:
Chronic Paronychia:
Understanding which type you have isn't just academic—it determines your entire treatment approach and expected recovery timeline.
Acute paronychia almost always starts with a break in the skin barrier around your nail. This creates an entry point for bacteria, which quickly multiply in the warm, moist environment. The most common culprits include:
🦠 Bacterial Invaders:
Common Triggers:
The infection typically develops within hours of the initial injury. Your body's immune response kicks in quickly, causing the characteristic inflammation and pus formation.
Acute paronychia announces itself loudly. You'll typically notice:
✋ Primary Symptoms:
Red Flags Requiring Immediate Attention:
If you notice any of these warning signs, seek professional medical care immediately. At The Minor Surgery Center, our team can quickly assess the severity and provide expert treatment without long wait times.
The good news about acute paronychia is that it usually responds well to treatment, especially when caught early. Your treatment plan depends on the severity of infection.
If you catch the infection within the first 24-48 hours before pus accumulates, conservative treatment often works:
Home Care Measures:
Medical Treatment:
When pus has collected under the skin, forming an abscess, you'll need incision and drainage—a minor surgical procedure that provides immediate relief.
The Drainage Procedure:
Post-Procedure Care:
Our experienced team at The Minor Surgery Center specializes in these minor procedures, making them as comfortable and stress-free as possible. You'll receive clear instructions and compassionate care throughout your recovery.
Unlike its acute counterpart, chronic paronychia isn't typically caused by a single traumatic event or bacterial infection. Instead, it results from repeated or prolonged exposure to irritants that damage the protective cuticle seal.
🔬 Primary Causative Factors:
Fungal Organisms:
Occupational and Lifestyle Risk Factors:
The condition creates a vicious cycle: irritation damages the cuticle → moisture gets trapped → fungi proliferate → inflammation persists → cuticle can't heal → cycle continues.
Chronic paronychia presents very differently from acute infection. Instead of sudden, severe pain, you'll experience:
📊 Characteristic Features:
Associated Changes:
The persistent nature of chronic paronychia can be frustrating. Many people try multiple treatments before finding what works, which is why accurate diagnosis is crucial.
Treating chronic paronychia requires patience and a multifaceted approach. Unlike acute infection, you can't simply drain an abscess and expect resolution.
Avoidance Strategies (Most Important!):
Topical Medications:
When conservative measures fail after 6-8 weeks, additional interventions may help:
Systemic Medications:
Procedural Options:
Adjunctive Therapies:
The key to success with chronic paronychia is consistency and patience. You might not see significant improvement for 4-6 weeks, and complete resolution can take 3-6 months.
Understanding the distinctions between these two conditions helps you recognize what you're dealing with and seek appropriate treatment.
FeatureAcute ParonychiaChronic ParonychiaOnsetSudden (hours to days)Gradual (weeks to months)Primary CauseBacterial (Staph aureus)Fungal (Candida) + irritantsPain LevelSevere, throbbingMild to moderateSwellingIntense, localizedModerate, intermittentPus FormationCommon, visible abscessRare, minimal dischargeNumber of NailsUsually single nailOften multiple nailsCuticleInitially intactLost or separatedNail ChangesMinimal (if treated early)Discoloration, ridging, thickeningTreatment Duration7-10 days3-6 monthsPrimary TreatmentAntibiotics ± drainageAvoidance + antifungalsRecurrenceUncommon (if treated)Common without lifestyle changes
Both types of paronychia can lead to serious complications if left untreated or improperly managed. Understanding these risks emphasizes why professional medical care matters.
⚠️ Potential Consequences:
Abscess Formation:
Felon:
Osteomyelitis:
Septic Arthritis:
Systemic Infection:
🔴 Long-Term Effects:
Permanent Nail Deformity:
Nail Loss:
Secondary Infections:
Functional Impairment:
Psychological Impact:
These complications aren't meant to scare you—they're preventable with timely, appropriate treatment. If you're experiencing symptoms of paronychia, don't wait. Contact The Minor Surgery Center for expert evaluation and treatment.
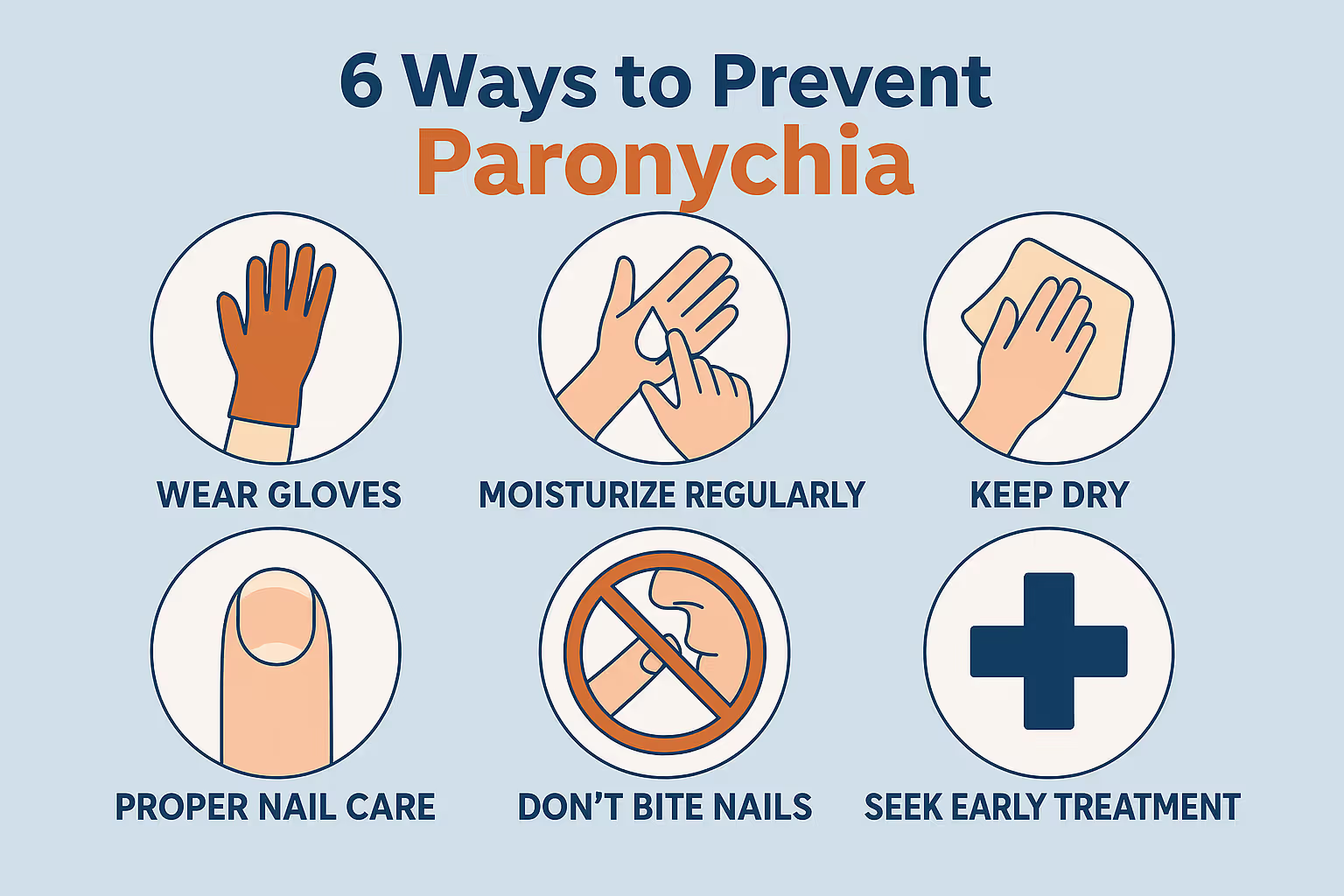
Prevention is always better than treatment. Whether you've had paronychia before or want to avoid it altogether, these strategies significantly reduce your risk.
🛡️ Essential Protective Measures:
Nail Care Best Practices:
Hand Hygiene:
Protective Equipment:
If you have diabetes, work in a wet environment, or have had paronychia before, take extra precautions:
For Healthcare Workers & Food Handlers:
For People with Diabetes:
For Those with Previous Paronychia:
While some very mild cases of paronychia might improve with home care, professional medical evaluation is important for proper diagnosis and treatment. Here's when you should definitely seek expert help:
🏥 Seek Medical Care If:
Immediate Attention Needed:
Schedule an Appointment Soon:
Why Professional Care Makes a Difference:
At The Minor Surgery Center, you'll receive:
✅ Accurate Diagnosis:
✅ Appropriate Treatment:
✅ Efficient Care:
Our team understands that nail infections can be painful, embarrassing, and disruptive to your daily life. We're here to provide compassionate, expert care that gets you back to normal quickly. Learn more about our approach to patient care.
Certain groups face unique challenges with paronychia and may need modified treatment approaches.
Paronychia in children often relates to thumb sucking, nail biting, or finger-in-mouth habits. Treatment considerations include:
Pregnancy changes can increase paronychia risk through:
Treatment modifications:
People with diabetes face significantly higher complication risks from paronychia:
Enhanced care includes:
Those with weakened immune systems (from HIV, chemotherapy, immunosuppressive medications, or chronic illness) need:
If you fall into any of these categories, don't hesitate to seek professional care early. Visit our conditions page to learn more about how we address various medical concerns.
For those dealing with chronic paronychia, the condition becomes a long-term management challenge rather than a quick fix. Success requires lifestyle adjustments and ongoing vigilance.
Daily Routine:
Weekly Maintenance:
Monthly Check-ins:
If your job contributes to chronic paronychia, you may need:
Environmental Modifications:
Career Considerations:
Living with a chronic condition affecting visible body parts can be emotionally challenging:
Remember: chronic paronychia is manageable, and most people achieve significant improvement with the right approach and patience.
Q: Can paronychia go away on its own without treatment?
Very mild acute paronychia caught extremely early might resolve with warm soaks alone, but this is risky. Without proper treatment, the infection typically worsens, potentially leading to abscess formation or deeper tissue involvement. Chronic paronychia virtually never resolves without addressing the underlying causes and using appropriate medications. Don't gamble with your health—seek professional evaluation.
Q: Is paronychia contagious?
No, paronychia itself isn't contagious. You can't "catch it" from someone else's infected nail. However, the bacteria or fungi that cause paronychia can be transferred (for example, through shared nail clippers or contaminated nail salon equipment), potentially leading to infection if you have a break in your skin. This is why proper instrument sterilization is crucial.
Q: How long does paronychia take to heal?
Acute paronychia: With proper treatment (antibiotics and drainage if needed), you should see significant improvement within 2-3 days, with complete healing in 7-10 days.
Chronic paronychia: This is a marathon, not a sprint. Initial improvement may take 4-6 weeks, with full resolution requiring 3-6 months of consistent treatment and avoidance of triggers.
Q: Can I still get manicures if I have chronic paronychia?
During active infection, avoid manicures completely. Once healed, you can resume manicures with important precautions: choose salons with excellent sterilization practices, inform your technician about your history, request they avoid cutting or pushing back cuticles, and consider bringing your own sanitized tools. Skip artificial nails, which trap moisture and increase recurrence risk.
Q: Will my nail look normal again after paronychia?
After acute paronychia: If treated promptly before significant nail matrix damage occurs, your nail should return to completely normal appearance as it grows out (3-6 months for fingernails).
After chronic paronychia: Nail changes like ridging, discoloration, or irregular growth may persist even after infection resolves. Some changes gradually improve over many months; others may be permanent. Early treatment minimizes lasting damage.
For more answers to common questions, visit our comprehensive FAQs page.
Paronychia—whether acute or chronic—is more than just a minor inconvenience. It's a genuine medical condition that deserves proper attention and treatment. The key distinctions between acute and chronic paronychia determine everything about your treatment approach, expected timeline, and prevention strategies.
Remember these essential points:
🎯 Acute paronychia requires prompt treatment with antibiotics and possibly drainage to prevent serious complications. Don't wait and hope it improves on its own.
🎯 Chronic paronychia demands patience, lifestyle modifications, and consistent treatment over months. Success depends on identifying and avoiding triggers while using appropriate antifungal therapy.
🎯 Professional diagnosis is crucial because misidentifying the type leads to ineffective treatment and prolonged suffering.
🎯 Prevention is your best strategy—protect your hands, avoid trauma to the nail folds, and seek early treatment for any signs of infection.
At The Minor Surgery Center, we understand that nail infections can be painful, frustrating, and embarrassing. You deserve expert care delivered with compassion and without the long wait times typical of emergency rooms or overcrowded clinics. Our experienced team provides accurate diagnosis, effective treatment, and clear guidance to help you achieve complete recovery.
Whether you're dealing with sudden, severe pain from acute paronychia or the persistent frustration of chronic nail fold inflammation, we're here to help. Don't let a nail infection disrupt your life any longer.
Ready to feel confident in your hands again? Contact us today to schedule your appointment. We'll provide the expert care you need in a safe, welcoming environment—because you deserve to feel comfortable in your own skin.
For more information about our services and approach to patient care, visit our blog for additional health resources and educational content.