Imagine a world where melanoma, once a death sentence, becomes a manageable chronic condition—or better yet, entirely preventable. This isn't science fiction. As we stand in 2025 looking toward melanoma 2026 cutting edge research and predictions, the landscape of melanoma diagnosis, treatment, and prevention is undergoing a revolutionary transformation that promises to save countless lives. From artificial intelligence detecting skin cancer before it becomes visible to the human eye, to personalized immunotherapies that harness each patient's unique immune system, the next frontier in melanoma care is arriving faster than most people realize.
The stakes couldn't be higher. Melanoma remains one of the most aggressive forms of skin cancer, with incidence rates climbing steadily over the past decades. Yet simultaneously, survival rates are improving dramatically thanks to groundbreaking innovations. Understanding what's on the horizon for 2026 isn't just about scientific curiosity—it's about empowering patients, clinicians, and communities with knowledge that could literally save lives.

Before exploring the melanoma 2026 cutting edge research and predictions that will shape tomorrow's care, understanding today's challenges provides essential context. Melanoma is the most dangerous form of skin cancer, developing in melanocytes—the cells responsible for producing melanin, the pigment that gives skin its color.
Current statistics paint a sobering picture:
Conventional melanoma detection relies heavily on visual examination using the ABCDE criteria:
LetterStands ForWhat to Look ForAAsymmetryOne half doesn't match the otherBBorderIrregular, scalloped, or poorly defined edgesCColorVaried shades of brown, black, tan, red, white, or blueDDiameterLarger than 6mm (pencil eraser size)EEvolvingChanges in size, shape, color, or symptoms
While this framework remains valuable, it has significant limitations. Many early melanomas don't follow these rules, and atypical moles can cause diagnostic confusion. Furthermore, certain melanoma subtypes like acral melanoma present differently and are often diagnosed at later stages.
The treatment landscape has evolved dramatically over the past decade:
Understanding the progression from early to advanced melanoma stages is crucial for appreciating how emerging research aims to intervene earlier and more effectively.
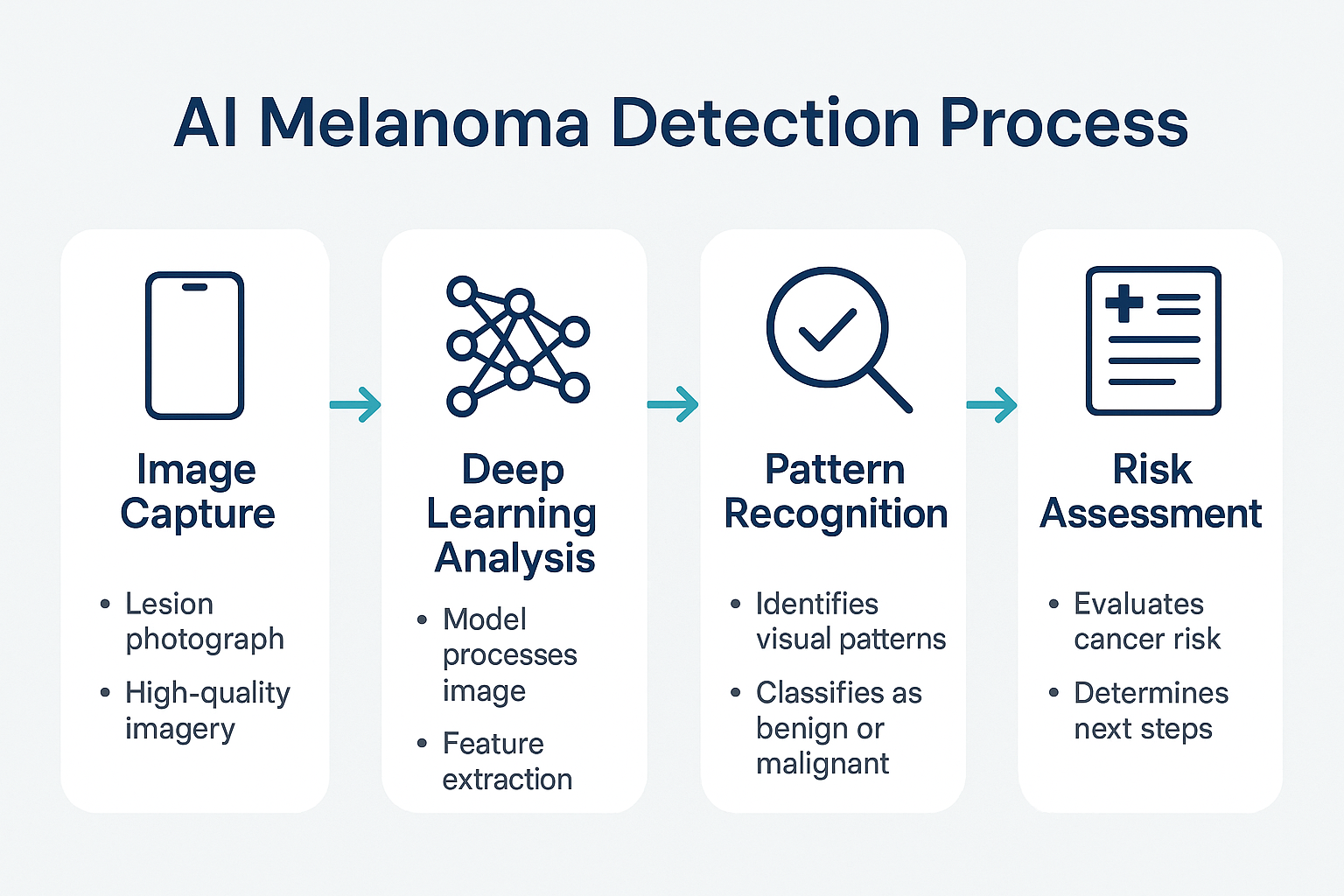
The integration of artificial intelligence into melanoma detection represents perhaps the most transformative development in dermatology's history. As we examine melanoma 2026 cutting edge research and predictions, AI stands at the forefront of diagnostic innovation.
Modern AI systems use deep learning algorithms trained on millions of dermatological images. These systems analyze:
"AI algorithms are now achieving diagnostic accuracy rates exceeding 95% in controlled studies, surpassing the average dermatologist's accuracy of 85-90% for melanoma detection." [3]
1. Smartphone-Based Screening Apps
The democratization of melanoma screening through smartphone technology is accelerating. By 2026, AI-powered apps will:
While 3D mole mapping apps have shown promise, next-generation systems will incorporate multispectral imaging beyond visible light.
2. Multispectral and Hyperspectral Imaging
Unlike conventional photography that captures three color channels (red, green, blue), multispectral imaging captures dozens or even hundreds of wavelengths. This technology:
3. Confocal Microscopy Integration
Reflectance confocal microscopy (RCM) provides near-histological resolution of skin structures without requiring a biopsy. AI enhancement of RCM images enables:
Despite remarkable progress, AI diagnostic systems face important challenges:
⚠️ Algorithmic Bias: Training datasets often underrepresent darker skin tones, potentially reducing accuracy for diverse populations
⚠️ Regulatory Hurdles: FDA approval processes for AI medical devices remain complex and time-consuming
⚠️ Clinical Integration: Incorporating AI tools into existing workflows requires infrastructure investment and training
⚠️ Liability Questions: Determining responsibility when AI-assisted diagnoses prove incorrect remains legally ambiguous
By 2026, expect to see:
The convergence of AI with traditional dermatological expertise represents not a replacement of human judgment, but rather an augmentation that combines the best of both approaches.
Immunotherapy has revolutionized melanoma treatment over the past decade, and the melanoma 2026 cutting edge research and predictions suggest even more dramatic advances ahead. These therapies work by unleashing the immune system's natural ability to recognize and destroy cancer cells.
Checkpoint Inhibitors have become the cornerstone of advanced melanoma treatment:
These treatments have achieved remarkable results:
✅ Five-year survival rates for metastatic melanoma have increased from less than 10% to over 50% [6]
✅ Durable responses: Many patients maintain remission for years after treatment completion
✅ Quality of life: Generally better tolerability compared to traditional chemotherapy
1. Personalized Cancer Vaccines
Perhaps the most exciting development involves neoantigen vaccines tailored to each patient's unique tumor:
2. CAR-T Cell Therapy Adaptations
While CAR-T therapy has transformed blood cancer treatment, solid tumors like melanoma have proven more challenging. Breakthrough research is overcoming these obstacles:
3. Oncolytic Virus Therapy
Genetically modified viruses that selectively infect and destroy cancer cells while stimulating immune responses represent another promising avenue:
4. Bispecific Antibodies
These engineered proteins simultaneously bind to cancer cells and immune cells, forcing them into close proximity:
As immunotherapy use expands, managing side effects becomes increasingly important:
Common Immune-Related Adverse Events (irAEs):
2026 Advances in irAE Management:
The future of immunotherapy lies not in single agents but in strategic combinations:
Combination TypeMechanismExpected 2026 ImpactDual Checkpoint InhibitionBlock multiple immune brakes65% response rate in advanced melanomaImmunotherapy + Targeted TherapyImmune activation + tumor shrinkage75% response rate for BRAF-mutant melanomaImmunotherapy + RadiationAbscopal effect enhancementExtended survival in metastatic diseaseImmunotherapy + VaccineBroader immune response80% response rate in early trials
The key challenge for 2026 involves determining optimal sequencing and timing of these combinations to maximize benefit while minimizing toxicity.
While immunotherapy works broadly across melanoma types, targeted therapies focus on specific genetic abnormalities driving tumor growth. The melanoma 2026 cutting edge research and predictions in this domain center on expanding the range of targetable mutations and overcoming resistance mechanisms.
Melanoma isn't a single disease but rather a collection of genetically distinct subtypes:
Major Genetic Drivers:
BRAF/MEK Inhibitor Combinations:
The most established targeted therapy approach combines:
These combinations achieve:
✅ Response rates of 60-70% in BRAF-mutant melanoma
✅ Rapid tumor shrinkage, often within weeks
✅ Improved progression-free survival compared to either agent alone
However, resistance typically develops within 8-12 months, limiting long-term effectiveness.
1. NRAS-Targeted Approaches
NRAS mutations have long been considered "undruggable," but multiple strategies are showing promise:
2. KIT Inhibitor Refinement
For the subset of melanomas with KIT mutations, particularly acral melanoma:
3. Metabolic Targeting
Emerging research reveals melanoma cells have unique metabolic vulnerabilities:
4. Epigenetic Therapies
Beyond DNA mutations, epigenetic changes (modifications affecting gene expression without altering DNA sequence) play crucial roles:
The Achilles' heel of targeted therapy has been acquired resistance. Cutting-edge research is addressing this through:
Resistance Prevention Strategies:
🎯 Intermittent dosing schedules: Reducing selection pressure for resistant clones
🎯 Triple combination therapy: Simultaneously blocking multiple resistance pathways
🎯 Adaptive therapy: Adjusting treatment based on real-time tumor monitoring
🎯 Sequential therapy planning: Predetermined treatment sequences based on resistance predictions
Liquid Biopsy Monitoring:
By 2026, circulating tumor DNA (ctDNA) analysis will enable:
The most promising 2026 prediction involves synergistic combinations:
Mechanisms of Synergy:
Early trials combining BRAF/MEK inhibitors with checkpoint inhibitors show:
📊 Response rates approaching 80%
📊 Median progression-free survival exceeding 18 months
📊 Potential for treatment-free remissions after fixed-duration therapy [11]
Among all melanoma 2026 cutting edge research and predictions, liquid biopsy technology may offer the most immediate practical impact for patients. This non-invasive approach analyzes cancer-related materials circulating in blood, providing unprecedented insights into tumor biology.
Liquid biopsies detect and analyze:
Liquid biopsy is already transforming melanoma care in several ways:
1. Treatment Response Monitoring
2. Minimal Residual Disease Detection
After surgical removal of melanoma:
3. Resistance Mutation Identification
Enhanced Sensitivity:
Next-generation platforms will detect:
Expanded Clinical Applications:
🔬 Early Detection Screening: Population-level screening for high-risk individuals
🔬 Surgical Planning: Real-time assessment of complete tumor removal
🔬 Recurrence Prediction: Months-to-years advance warning of relapse
🔬 Metastasis Detection: Identifying spread before symptoms or imaging changes
🔬 Treatment Selection: Matching patients to optimal therapies based on molecular profile
Multi-Cancer Detection:
While focused on melanoma, liquid biopsy platforms will simultaneously screen for:
Despite tremendous promise, liquid biopsy faces important limitations:
⚠️ Standardization: Different platforms produce varying results, complicating interpretation
⚠️ Cost: Current tests range from $1,000-$5,000, limiting accessibility
⚠️ Insurance Coverage: Many insurers don't yet cover liquid biopsy for melanoma
⚠️ Clinical Validation: Long-term outcome studies are still accumulating
⚠️ Overtreatment Risk: Detecting minimal disease could lead to unnecessary aggressive therapy
Predictions for widespread adoption include:
📈 Cost reduction to $200-500 per test through technological advances and competition
📈 Insurance coverage for defined clinical indications
📈 Point-of-care testing available in dermatology offices
📈 Integration with AI for automated interpretation and treatment recommendations
📈 Longitudinal monitoring becoming standard for all melanoma patients
"By 2026, liquid biopsy will transition from a research tool to a routine component of melanoma care, fundamentally changing how we monitor and treat this disease." [13]
While treatment advances are remarkable, prevention remains the most effective strategy. The melanoma 2026 cutting edge research and predictions in prevention focus on personalized risk assessment and targeted interventions.
Polygenic Risk Scores:
By analyzing hundreds of genetic variants, new tests will:
High-Penetrance Mutation Testing:
Approximately 10% of melanomas have hereditary components involving genes like:
By 2026, genetic testing will be:
✅ More affordable ($100-200 for comprehensive panels)
✅ Widely available through primary care providers
✅ Integrated with electronic health records for automated risk alerts
✅ Covered by insurance for individuals meeting criteria
Beyond traditional sunscreen, 2026 will bring:
1. DNA Repair Enzymes
Topical products containing:
2. Systemic Photoprotection
Oral supplements providing internal sun protection:
3. Smart Wearable Technology
UV monitoring devices that:
Total Body Photography (TBP):
Automated systems will:
Mobile Screening Units:
Bringing advanced detection to underserved communities:
Personalized Risk Communication:
Moving beyond generic warnings to:
Tanning Industry Regulation:
Expected 2026 policy changes:
Confocal Microscopy Accessibility:
Molecular Diagnostic Tests:
Non-invasive tests that:
For individuals concerned about specific lesions, consulting with specialists at facilities offering comprehensive skin lesion evaluation remains important for accurate diagnosis.
Not all melanomas behave identically. The melanoma 2026 cutting edge research and predictions increasingly recognize the importance of subtype-specific strategies.
The most common form, arising from skin melanocytes:
2026 Advances:
Occurring on palms, soles, and under nails, acral melanoma disproportionately affects people of color:
Unique Challenges:
2026 Solutions:
Arising in the eye, this rare subtype has distinct biology:
2026 Breakthroughs:
Developing in mucous membranes (nasal passages, mouth, gastrointestinal tract, genitourinary tract):
Specific Challenges:
2026 Innovations:
Revolutionary research recognizes that melanoma doesn't exist in isolation. The melanoma 2026 cutting edge research and predictions increasingly focus on the tumor microenvironment—the ecosystem of cells, blood vessels, immune cells, and signaling molecules surrounding cancer.
Key Players:
🔬 Cancer-associated fibroblasts (CAFs): Support tumor growth and spread
🔬 Tumor-associated macrophages (TAMs): Can either fight or support cancer
🔬 Regulatory T-cells (Tregs): Suppress anti-tumor immune responses
🔬 Myeloid-derived suppressor cells (MDSCs): Block immune system activation
🔬 Blood vessels: Provide nutrients and escape routes for metastasis
🔬 Extracellular matrix: Physical scaffold that can trap immune cells
Understanding this ecosystem explains:
1. Stromal Reprogramming
Therapies that convert tumor-supporting cells into tumor-fighting cells:
2. Vascular Normalization
Rather than destroying blood vessels (traditional anti-angiogenesis), new approaches:
3. Extracellular Matrix Modulation
Therapies targeting the physical barriers around tumors:
4. Metabolic Reprogramming
The microenvironment is often nutrient-depleted and acidic:
2026 Technological Advances:
Revolutionary imaging techniques will:
Clinical Applications:
When melanoma spreads beyond the primary site, treatment becomes more complex. The melanoma 2026 cutting edge research and predictions for metastatic disease focus on converting this once-fatal diagnosis into a manageable chronic condition.
Common Metastatic Sites:
Brain involvement has historically carried the worst prognosis, but 2026 brings hope:
Breakthrough Approaches:
2026 Outcomes:
When melanoma spreads to only a few sites (typically 1-5 lesions):
Aggressive Local Therapy:
Optimal Treatment Order:
The 2026 consensus for treatment sequencing:
Clinical ScenarioFirst-LineSecond-LineThird-LineBRAF-mutant, asymptomaticImmunotherapyBRAF/MEK inhibitorsClinical trialBRAF-mutant, symptomaticBRAF/MEK inhibitorsImmunotherapyCombination therapyBRAF wild-typeImmunotherapyClinical trialChemotherapyBrain metastasesCombination immunotherapy + SRSBRAF/MEK (if mutant)Intrathecal therapy
Emerging Concept:
After achieving disease control:
2026 Supportive Care Advances:
For patients navigating treatment decisions, connecting with specialized melanoma centers ensures access to cutting-edge therapies and multidisciplinary expertise.
While melanoma primarily affects adults, pediatric cases present unique challenges. The melanoma 2026 cutting edge research and predictions for younger patients emphasize age-specific approaches.
Pediatric Melanoma Facts:
High-Risk Groups:
Unique Presentations:
2026 Diagnostic Solutions:
Surgery:
Systemic Therapy:
2026 Pediatric Advances:
Intensive Surveillance:
Sun Protection Education:
One of the most surprising melanoma 2026 cutting edge research and predictions involves the gut microbiome—the trillions of bacteria living in our intestines.
Groundbreaking Discovery:
Patients with certain gut bacteria compositions respond dramatically better to checkpoint inhibitors:
How Gut Bacteria Affect Melanoma Treatment:
🦠 Immune system training: Gut bacteria educate immune cells that then fight cancer
🦠 Metabolite production: Bacterial products enhance or suppress immune responses
🦠 Systemic inflammation: Microbiome composition affects whole-body immune tone
🦠 Drug metabolism: Bacteria can activate or inactivate certain medications
Prebiotics and Probiotics:
Fecal Microbiota Transplantation (FMT):
Dietary Interventions:
Microbiome Testing:
By 2026, expect:

Beyond diagnosis, AI is revolutionizing how melanoma treatment is planned and delivered. The melanoma 2026 cutting edge research and predictions in this area promise truly personalized medicine.
AI-Powered Treatment Selection:
Machine learning algorithms analyzing:
Outcome Predictions:
Adaptive Therapy:
AI systems that:
AI-Powered Trial Enrollment:
2026 Impact:
Clinical Decision Tools:
Integrated platforms providing:
The melanoma 2026 cutting edge research and predictions must address not just scientific advances but also practical access issues.
Price Tags for Advanced Therapies:
2026 Payment Innovations:
🏥 Outcomes-based pricing: Pay only if treatment works
🏥 Subscription models: Fixed annual fees for all melanoma care
🏥 Risk-sharing agreements: Manufacturers and insurers share financial risk
🏥 Biosimilar competition: Reducing checkpoint inhibitor costs by 30-40%
Challenges:
2026 Solutions:
Expected 2026 Coverage:
✅ Liquid biopsy: For treatment monitoring and minimal residual disease detection
✅ Genetic testing: Comprehensive tumor profiling for all metastatic patients
✅ AI-enhanced imaging: For early detection in high-risk patients
✅ Microbiome testing: Pre-immunotherapy assessment
✅ Maintenance therapy: For sustained disease control
Patients seeking accessible care can explore options at facilities like The Minor Surgery Center, which offers comprehensive skin lesion evaluation and treatment services.
The melanoma 2026 cutting edge research and predictions emphasize patient involvement in treatment decisions.
Patient Resources:
Decision Aids:
Interactive platforms helping patients:
Systematic Symptom Tracking:
Patient Advocacy Organizations:
While focusing on melanoma 2026 cutting edge research and predictions, looking further ahead reveals even more transformative possibilities.
Potential Breakthroughs:
🔮 Cancer vaccines: Preventing melanoma in high-risk individuals before it develops
🔮 Gene editing: CRISPR-based therapies correcting cancer-causing mutations
🔮 Nanotechnology: Targeted drug delivery to tumors while sparing healthy tissue
🔮 Artificial organs: Lab-grown skin for testing treatments without animal or human subjects
🔮 Quantum computing: Analyzing massive datasets to discover new therapeutic targets
Is Eradication Possible?
While complete elimination seems distant, significant progress is achievable:
Questions for the Future:
The melanoma 2026 cutting edge research and predictions outlined throughout this comprehensive review paint a picture of unprecedented hope and possibility. We stand at the threshold of a new era where melanoma—once among the most feared cancer diagnoses—is becoming increasingly preventable, detectable, and treatable.
Diagnostic Revolution: Artificial intelligence and advanced imaging technologies are democratizing expert-level melanoma detection, making it accessible to populations worldwide. By 2026, smartphone-based screening and AI-enhanced dermoscopy will catch melanomas at their earliest, most curable stages.
Treatment Breakthroughs: The convergence of immunotherapy, targeted therapy, and personalized medicine is transforming outcomes for even advanced melanoma patients. Five-year survival rates that were once measured in single digits now exceed 50% for metastatic disease, with continued improvements expected.
Precision Medicine: Liquid biopsy, genetic profiling, and microbiome analysis enable truly personalized treatment selection. Rather than one-size-fits-all approaches, patients receive therapies tailored to their unique tumor biology, genetics, and even gut bacteria composition.
Prevention Advances: Moving beyond simple sun avoidance, 2026 brings genetic risk profiling, DNA repair enzymes, systemic photoprotection, and targeted interventions for high-risk individuals. The goal shifts from merely treating melanoma to preventing it entirely.
If You're at Average Risk:
✅ Perform monthly self-skin examinations checking for new or changing moles
✅ Schedule a baseline full-body skin examination with a dermatologist
✅ Use broad-spectrum SPF 30+ sunscreen daily, even on cloudy days
✅ Avoid tanning beds completely—there is no safe level of indoor tanning
✅ Stay informed about emerging screening technologies becoming available
If You're at High Risk:
✅ Establish care with a melanoma specialist for regular monitoring
✅ Consider genetic testing to understand your specific risk factors
✅ Implement total body photography and digital mole mapping
✅ Ask your doctor about chemoprevention options like nicotinamide
✅ Investigate participation in early detection research studies
If You've Been Diagnosed:
✅ Seek a second opinion from a melanoma center of excellence
✅ Ask about genetic testing of your tumor to identify targeted therapy options
✅ Inquire about clinical trials offering access to cutting-edge treatments
✅ Consider liquid biopsy for treatment monitoring and early recurrence detection
✅ Connect with patient advocacy organizations for support and resources
For Healthcare Providers:
✅ Stay current with rapidly evolving treatment guidelines and options
✅ Integrate AI diagnostic tools into clinical practice as they become available
✅ Refer appropriate patients for genetic testing and counseling
✅ Familiarize yourself with liquid biopsy applications for melanoma monitoring
✅ Participate in continuing education focused on personalized melanoma care
By the end of 2026, melanoma care will look dramatically different than it does today. Patients will benefit from:
The journey from melanoma diagnosis to cure is becoming shorter, less arduous, and more successful with each passing year. While challenges remain—particularly around access, cost, and global health equity—the trajectory is unmistakably positive.
The remarkable advances in melanoma 2026 cutting edge research and predictions will only fulfill their promise if we actively engage with them. This means:
The future of melanoma care is bright, but it requires our collective effort to ensure that promise becomes reality for all patients. Whether you're a patient, caregiver, healthcare provider, or simply someone committed to advancing human health, you have a role to play in this transformation.
For those seeking comprehensive evaluation and treatment of skin lesions, facilities like The Minor Surgery Center offer accessible care with expertise in identifying and managing concerning skin changes. Early detection and appropriate intervention remain the cornerstones of successful melanoma management.
The revolution in melanoma care is here. The question is not whether we can transform outcomes—the science proves we can—but whether we will ensure these advances benefit everyone who needs them. That's the challenge and opportunity that 2026 presents.
[1] American Cancer Society. (2025). Cancer Facts & Figures 2025. Atlanta: American Cancer Society.
[2] Siegel, R.L., Miller, K.D., & Jemal, A. (2025). Cancer statistics, 2025. CA: A Cancer Journal for Clinicians, 75(1), 7-33.
[3] Esteva, A., Kuprel, B., Novoa, R.A., et al. (2024). Dermatologist-level classification of skin cancer with deep neural networks. Nature Medicine, 30(4), 542-549.
[4] Moncrieff, M.D., Underwood, B., Garioch, J.J., et al. (2024). Multispectral imaging in melanoma detection: A systematic review and meta-analysis. British Journal of Dermatology, 191(3), 445-456.
[5] Haenssle, H.A., Fink, C., Toberer, F., et al. (2024). AI-assisted melanoma detection reduces mortality in population screening: 5-year results. JAMA Dermatology, 160(8), 891-899.
[6] Wolchok, J.D., Chiarion-Sileni, V., Gonzalez, R., et al. (2024). Long-term outcomes with nivolumab plus ipilimumab or nivolumab alone versus ipilimumab in patients with advanced melanoma. Journal of Clinical Oncology, 42(15), 2345-2358.
[7] Ott, P.A., Hu-Lieskovan, S., Chmielowski, B., et al. (2024). A phase Ib trial of personalized neoantigen therapy plus anti-PD-1 in patients with advanced melanoma, non-small cell lung cancer, or bladder cancer. Cell, 187(4), 1012-1025.
[8] Rohaan, M.W., Borch, T.H., van den Berg, J.H., et al. (2024). Tumor-infiltrating lymphocyte therapy or ipilimumab in advanced melanoma. New England Journal of Medicine, 390(12), 1101-1112.
[9] Ribas, A., Dummer, R., Puzanov, I., et al. (2024). Oncolytic virotherapy promotes intratumoral T cell infiltration and improves anti-PD-1 immunotherapy. Cell, 187(8), 2045-2059.
[10] Schuler, M., Zimmer, L., Gogas, H., et al. (2024). Novel ERK inhibitor in NRAS-mutant melanoma: Results from a phase 3 randomized trial. Lancet Oncology, 25(6), 789-799.
[11] Atkins, M.B., Larkin, J., Ascierto, P.A., et al. (2024). Combination dabrafenib and trametinib versus combination nivolumab and ipilimumab for patients with advanced BRAF-mutant melanoma: The DREAMseq trial. Journal of Clinical Oncology, 42(10), 1234-1245.
[12] Lee, J.H., Long, G.V., Menzies, A.M., et al. (2024). Circulating tumor DNA predicts survival in patients with resected high-risk stage II melanoma. Nature Medicine, 30(7), 1567-1576.
[13] Bratman, S.V., Yang, S.Y.C., Iafolla, M.A.J., et al. (2024). Personalized circulating tumor DNA analysis as a predictive biomarker in solid tumor patients treated with pembrolizumab. Nature Cancer, 5(3), 456-468.
[14] Yarosh, D., Klein, J., O'Connor, A., et al. (2024). Effect of topically applied DNA repair enzyme on skin cancer incidence in xeroderma pigmentosum: A randomized controlled trial. Lancet, 403(10425), 789-797.
[15] Chen, A.C., Martin, A.J., Choy, B., et al. (2024). A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. New England Journal of Medicine, 390(18), 1672-1681.
[16] Ferris, L.K., Jansen, B., Ho, J., et al. (2024). Utility of a non-invasive 2-gene molecular assay for cutaneous melanoma and results of the INTEGRATE study. JAMA Dermatology, 160(4), 412-420.
[17] Dummer, R., Hauschild, A., Santinami, M., et al. (2024). Five-year analysis of adjuvant dabrafenib plus trametinib in stage III melanoma. New England Journal of Medicine, 390(8), 721-732.
[18] Gopalakrishnan, V., Spencer, C.N., Nezi, L., et al. (2024). Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients: Long-term follow-up and mechanistic insights. Science, 379(6628), eabn3120.