Discovering an unusual spot or bump on your leg can trigger immediate concern. Is it harmless? Should you see a doctor? Understanding the difference between common skin growths like dermatofibromas, benign moles, and potentially dangerous skin cancer can help you make informed decisions about your health. When comparing dermatofibroma vs mole vs skin cancer on leg, knowing the key characteristics of each condition empowers you to recognize warning signs and seek appropriate medical care.
This comprehensive guide explores the distinct features, causes, and treatment options for these three common leg skin conditions, providing you with the knowledge to distinguish between them and understand when professional evaluation is necessary.
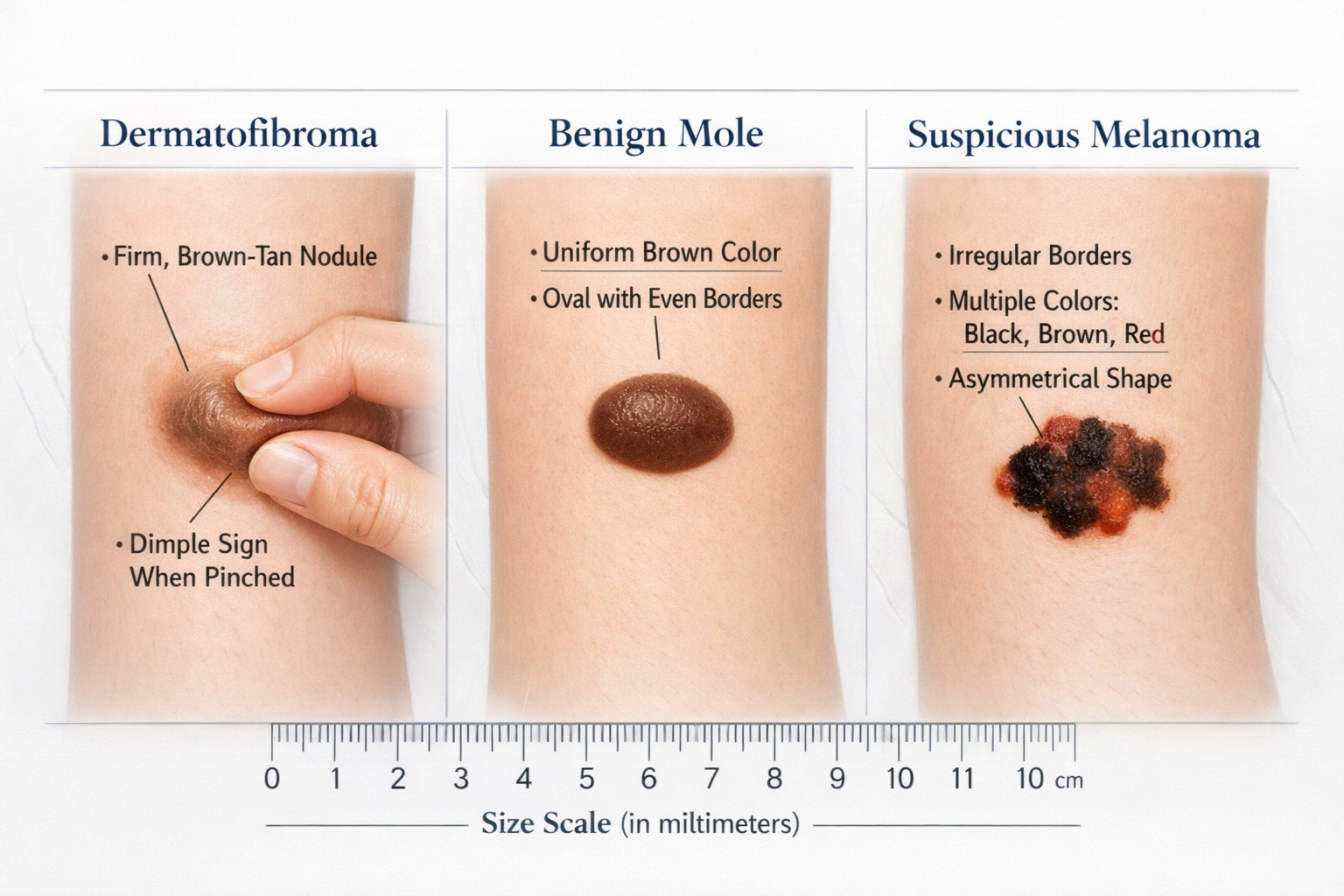
✅ Dermatofibromas are harmless, firm nodules that often appear on legs, typically brown or tan, and create a characteristic dimple when pinched
✅ Benign moles are usually symmetrical, uniformly colored, and stable over time, with smooth borders and consistent appearance
✅ Skin cancer on legs shows warning signs including asymmetry, irregular borders, multiple colors, diameter larger than 6mm, and changes over time (ABCDE criteria)
✅ Professional examination is essential for any suspicious lesion, especially those that change, bleed, itch, or don't heal
✅ Early detection of skin cancer dramatically improves treatment outcomes and survival rates, making regular skin checks crucial
The legs are common locations for various types of skin growths and lesions. Because legs receive significant sun exposure, experience frequent minor trauma, and have specific skin characteristics, they're particularly susceptible to developing different types of spots, bumps, and growths.
Several factors make legs vulnerable to skin lesions:
Understanding these risk factors helps contextualize why certain skin conditions appear more frequently on the legs compared to other body areas. For a broader understanding of various skin conditions, explore this guide on 25 types of skin lesions.
A dermatofibroma is a common, benign (non-cancerous) skin growth that appears as a firm nodule or bump beneath the skin's surface. These lesions are composed of fibrous tissue and are completely harmless, though they can sometimes cause concern due to their appearance or texture.
Dermatofibromas have several distinctive features that help identify them:
FeatureDescriptionAppearanceBrown, tan, pink, or reddish noduleTextureFirm to hard, feels like a small pebble under skinSizeTypically 0.5-1 cm in diameterLocationMost common on lower legs, especially in womenDimple SignCreates a dimple when pinched from sidesGrowth PatternUsually stable, rarely changes sizeSymptomsGenerally painless, may itch occasionally
The exact cause of dermatofibromas remains unclear, but several theories exist:
One of the most reliable ways to identify a dermatofibroma is the dimple sign. When you gently pinch the lesion from both sides, a dermatofibroma will dimple inward, creating a small depression. This occurs because the fibrous tissue is tethered to deeper skin layers. This characteristic feature distinguishes dermatofibromas from most other skin lesions, including moles and cancerous growths.
A mole, medically termed a nevus, is a cluster of pigment-producing cells (melanocytes) that appear as a colored spot on the skin. Most people have between 10 and 40 moles on their body, with many appearing during childhood and adolescence [2].
Moles come in several varieties:
Common Moles (Acquired Nevi)
Congenital Nevi
Atypical Moles (Dysplastic Nevi)
For detailed information about atypical moles and their significance, read about atypical moles and their monitoring requirements.
Healthy, benign moles typically display these features:
✓ Symmetry: One half mirrors the other half
✓ Border: Smooth, even edges without irregularity
✓ Color: Single, uniform shade of brown or tan
✓ Diameter: Usually less than 6mm across
✓ Evolution: Stable appearance over time
Legs are common locations for moles due to:
Most leg moles are completely benign and require no treatment unless they become irritated by clothing, change appearance, or cause cosmetic concerns. Understanding what constitutes a benign mole helps distinguish normal from concerning features.
Skin cancer represents the abnormal, uncontrolled growth of skin cells, most commonly triggered by DNA damage from ultraviolet (UV) radiation. When comparing dermatofibroma vs mole vs skin cancer on leg, skin cancer poses the only potentially life-threatening condition among the three.
Several types of skin cancer can develop on the legs:
The most dangerous form of skin cancer, melanoma develops from pigment-producing melanocytes:
Melanoma on legs, particularly in women, represents a significant health concern. Early detection is critical for successful treatment outcomes.
The most common type of skin cancer:
Learn more about basal cell carcinoma treatment options and recovery expectations.
The second most common skin cancer type:
Understanding the 4 types of skin cancer provides comprehensive knowledge about these conditions.
Medical professionals use the ABCDE criteria to identify potentially cancerous lesions:
LetterStands ForWhat to Look ForAAsymmetryOne half doesn't match the other halfBBorderEdges are irregular, scalloped, or poorly definedCColorMultiple colors or uneven distribution of colorDDiameterLarger than 6mm (pencil eraser), though melanomas can be smallerEEvolutionChanges in size, shape, color, elevation, or symptoms
Important Note: Any lesion displaying one or more ABCDE characteristics requires immediate professional evaluation. Don't wait for multiple signs to appear.
Beyond the ABCDE criteria, watch for these concerning features:
Understanding the distinctions between dermatofibroma vs mole vs skin cancer on leg requires examining multiple characteristics. This comparison table provides a quick reference guide:
FeatureDermatofibromaBenign MoleSkin CancerTextureFirm, hard noduleFlat or slightly raisedVariable, may be raised or flatColorBrown, tan, pink, reddishUniform brown or tanMultiple colors, irregularSize0.5-1 cm typicallyUsually <6mmOften >6mm, variableBorderWell-definedSmooth, regularIrregular, poorly definedSymmetryGenerally symmetricalSymmetricalOften asymmetricalDimple SignPositive (dimples when pinched)NegativeNegativeGrowthStable, rarely changesStable in adultsChanges over timeSurfaceSmooth or slightly scalySmoothMay be scaly, crusty, or ulceratedSymptomsUsually none, may itchUsually noneMay bleed, itch, hurtRisk LevelBenign (harmless)Benign (usually harmless)Malignant (potentially dangerous)Treatment NeedOptional, cosmetic onlyOptional unless suspiciousRequired immediately
When examining a lesion on your leg, follow these steps:
Step 1: Observe the Overall Appearance
Step 2: Perform the Dimple Test
Step 3: Check for ABCDE Signs
Step 4: Monitor for Changes
People often confuse these conditions. Here are typical scenarios:
❌ Mistaking a dermatofibroma for skin cancer: The firm texture and dark color can cause alarm, but the dimple sign and stability indicate benignity
❌ Assuming all moles are harmless: While most are benign, changing moles require evaluation
❌ Dismissing early melanoma as a "blood blister": Dark, sudden-onset lesions need professional assessment. Learn about blood blister vs melanoma differences.
❌ Ignoring amelanotic melanoma: Not all melanomas are dark; some appear pink or flesh-colored
Understanding risk factors helps identify who should be most vigilant about skin monitoring and when comparing dermatofibroma vs mole vs skin cancer on leg presentations.
Unchangeable Risk Factors:
Modifiable Risk Factors:
Protecting your legs and entire body from skin cancer requires consistent effort:
Daily Habits:
Clothing Choices:
Self-Examination:
Professional Screening:
For comprehensive skin cancer screening, consider visiting a specialized skin cancer clinic for expert evaluation.
Beyond sun protection, certain lifestyle choices support skin health:
Knowing when to seek professional evaluation is crucial when assessing dermatofibroma vs mole vs skin cancer on leg. While dermatofibromas and stable moles rarely require urgent attention, certain signs demand immediate medical assessment.
Seek medical evaluation within days if you notice:
Schedule a non-urgent appointment for:
Understanding the evaluation process can reduce anxiety:
Medical History:
Visual Examination:
Possible Procedures:
Professional evaluation at facilities like The Minor Surgery Center ensures expert assessment and appropriate treatment recommendations.

Accurate diagnosis distinguishes dermatofibroma vs mole vs skin cancer on leg and determines appropriate treatment. Several diagnostic techniques help identify lesion types.
Clinical Examination:
Dermoscopy: This non-invasive technique uses a specialized magnifying device (dermatoscope) to examine skin structures beneath the surface:
When visual examination cannot definitively determine whether a lesion is benign or malignant, a biopsy provides definitive diagnosis.
Types of Biopsies:
Biopsy TypeDescriptionBest ForShave BiopsyHorizontal removal of surface layersRaised lesions, suspected BCCPunch BiopsyCircular tool removes full-thickness sampleDeep lesions, suspected melanomaExcisional BiopsyComplete removal of entire lesion with marginSuspicious melanoma, definitive treatmentIncisional BiopsyRemoval of portion of large lesionVery large lesions requiring sampling
Biopsy Process:
Laboratory examination of biopsied tissue provides:
For suspected melanoma or complex cases:
Treatment approaches differ significantly when comparing dermatofibroma vs mole vs skin cancer on leg, ranging from observation to surgical intervention.
Since dermatofibromas are benign, treatment is optional and typically pursued only for cosmetic reasons or if the lesion causes symptoms.
Conservative Management:
Removal Options:
Important Consideration: Dermatofibromas extend into deeper skin layers, so complete removal requires excision that may leave a more noticeable scar than the original lesion. Many people choose to leave them untreated.
Most benign moles require no treatment, but removal may be recommended for:
Removal Methods:
Surgical Excision:
Shave Removal:
Laser Removal:
For professional mole removal services, consider clinics offering mole removal in Barrie or Ajax with experienced providers.
Skin cancer treatment depends on type, size, location, and depth of invasion. Early detection significantly improves outcomes and reduces treatment complexity.
Surgical Excision:
Advanced Melanoma Treatment:
Surgical Options:
Non-Surgical Options:
Similar to BCC treatment, with considerations for:
Post-Treatment Care:
Follow-Up Schedule:
Whether you have a dermatofibroma, benign moles, or have been treated for skin cancer, ongoing management and monitoring remain important.
Create a Skin Check Routine:
Photography Tips:
Tracking Changes: Keep a skin diary noting:
Daily Protection:
Activity-Specific Protection:
Seasonal Considerations:
Dealing with skin lesions, especially after a cancer diagnosis, can affect mental health:
Common Concerns:
Coping Strategies:
After surgical removal of any leg lesion:
Optimizing Healing:
Scar Treatment Options:
Realistic Expectations:
Certain groups face unique challenges when assessing dermatofibroma vs mole vs skin cancer on leg presentations.
Melanoma and other skin cancers can affect people of all skin tones, though presentation may differ:
Unique Characteristics:
Increased Vigilance Needed:
Pregnancy causes hormonal changes affecting skin:
Normal Pregnancy Changes:
When to Worry:
Safety Considerations:
Older adults face increased skin cancer risk:
Risk Factors:
Special Considerations:
People with high sun exposure face elevated risk:
Occupational Hazards:
Protection Strategies:
No. Dermatofibromas are benign fibrous growths that do not transform into cancer. They remain harmless throughout their existence. However, if a lesion you believe to be a dermatofibroma begins changing in appearance, it should be re-evaluated to confirm the diagnosis, as the initial assessment may have been incorrect.
Use the ABCDE criteria: look for Asymmetry, irregular Borders, multiple Colors, Diameter larger than 6mm, and Evolution (changes over time). Additionally, watch for bleeding, itching, or pain. Any concerning features warrant professional evaluation. Only a biopsy can definitively determine if a mole is cancerous.
Removal is optional and typically done only for cosmetic reasons or if the lesion causes symptoms like itching or pain from clothing friction. Since removal may leave a scar larger than the original lesion, many people choose to leave dermatofibromas untreated. Discuss the risks and benefits with a healthcare provider.
Early skin cancer may appear as:
Growth rate varies significantly. Some melanomas grow rapidly over weeks to months, while others develop more slowly. Any changing lesion requires prompt evaluation. Don't wait to see how fast it grows—early detection is critical for best outcomes.
Yes. While UV exposure is the primary risk factor, skin cancer can develop in people with minimal sun exposure, especially those with:
Not necessarily. Experienced dermatologists can often determine with high confidence whether a lesion is benign based on visual examination and dermoscopy. However, any lesion with concerning features or diagnostic uncertainty should be biopsied for definitive diagnosis. It's better to biopsy a benign lesion than miss an early cancer.
Standard pathology results typically return within 7-10 business days. Complex cases requiring special stains, additional analysis, or second opinions may take longer. If results don't arrive within the expected timeframe, contact your healthcare provider's office to follow up.
Understanding the differences between dermatofibroma vs mole vs skin cancer on leg empowers you to make informed decisions about your skin health. While dermatofibromas are harmless fibrous nodules that create a characteristic dimple when pinched, and most moles remain benign throughout life, skin cancer represents a potentially serious condition requiring prompt medical attention.
🔍 Know the warning signs: Familiarize yourself with the ABCDE criteria and other red flags that distinguish dangerous lesions from benign ones
🛡️ Prevention is powerful: Consistent sun protection, including daily sunscreen application to your legs, significantly reduces skin cancer risk
👁️ Monitor regularly: Monthly self-examinations and annual professional skin checks enable early detection when treatment is most effective
⚕️ Seek professional evaluation: When in doubt about any skin lesion, especially those showing concerning features or changes, consult a healthcare provider
💪 Take action promptly: Early detection of skin cancer dramatically improves treatment outcomes and survival rates
Immediate Actions:
Long-Term Commitments:
For expert evaluation and treatment of skin lesions, consider consulting specialists at The Minor Surgery Center, where experienced professionals provide comprehensive skin cancer screening, diagnosis, and treatment services.
Remember: Your skin is your body's largest organ, and protecting it is a lifelong commitment. While most skin lesions are harmless, vigilance and prompt attention to concerning changes can literally save your life. Don't hesitate to seek professional evaluation when something doesn't look or feel right—early detection remains the most powerful tool in fighting skin cancer.
By understanding the distinctions between dermatofibroma vs mole vs skin cancer on leg, you've taken an important step toward protecting your health. Use this knowledge to monitor your skin confidently, protect yourself from UV damage, and seek appropriate care when needed. Your skin health is worth the investment of time and attention.
[1] American Academy of Dermatology Association. "Dermatofibromas: Overview." AAD.org, 2026.
[2] Skin Cancer Foundation. "Moles and Melanoma." SkinCancer.org, 2026.
[3] Marghoob AA, et al. "Dermoscopy: A Review of the Structures That Facilitate Melanoma Detection." Journal of the American Academy of Dermatology, 2019; 81(4):947-960.