Every year, thousands of Canadians discover they have skin cancer—but here's the encouraging truth: when detected early through professional screening and biopsy, skin cancer is one of the most treatable forms of cancer. With Mississauga offering world-class skin biopsy clinic Mississauga facilities and comprehensive skin cancer check Mississauga services, residents have unprecedented access to potentially life-saving diagnostic care. Whether you've noticed a suspicious mole, have a family history of melanoma, or simply want peace of mind, understanding your screening and biopsy options in Mississauga Skin Biopsy & Skin Cancer Screening facilities can make all the difference in protecting your health.

✅ Skin cancer is Canada's most common cancer, accounting for approximately one-third of all cancer diagnoses annually, making regular screening essential for early detection and successful treatment.
✅ Mississauga offers multiple rapid-access screening options including walk-in services, specialized clinics like The Minor Surgery Center, and seasonal programs like Melanoma Canada's Mole Mobile—no referral or health card required.
✅ Professional skin biopsies have high diagnostic accuracy, with over 20% of biopsies performed at specialized clinics testing positive for cancer, confirming the importance of expert evaluation.
✅ Advanced dermoscopy technology like Fotofinder enables detection of subtle changes in moles and lesions over time, significantly improving early melanoma detection rates.
✅ Early-stage skin cancer is highly curable when detected through professional examination and timely biopsy, with same-week surgical removal available at accredited facilities throughout Mississauga.
Skin cancer has become a significant public health concern across Canada, with diagnosis rates continuing to climb year after year. As the most commonly diagnosed cancer in the country, skin cancer represents approximately one-third of all cancers diagnosed annually[1]. This staggering statistic underscores the critical importance of regular screening and early detection.
Understanding the different types of skin cancer helps explain why professional screening is so vital:
🔬 Basal Cell Carcinoma (BCC)
🔬 Squamous Cell Carcinoma (SCC)
🔬 Melanoma
For a comprehensive understanding of these conditions, explore the detailed guide on 4 types of skin cancer available through specialized medical resources.
The difference between early-stage and advanced skin cancer is profound. Early-stage skin cancer is curable when detected through regular professional skin examinations and biopsies[2]. This simple fact has driven the development of sophisticated screening programs throughout Mississauga and the Greater Toronto Area.
Consider these compelling statistics:
This high positive rate demonstrates that professional clinical judgment in selecting which lesions require biopsy is remarkably accurate—and potentially life-saving.
A skin biopsy is a medical procedure where a small sample of skin tissue is removed and examined under a microscope to diagnose various skin conditions, including cancer. Despite what many people fear, modern biopsy techniques are minimally invasive, performed under local anesthesia, and typically cause minimal discomfort.
Medical professionals use several biopsy techniques depending on the size, location, and suspected nature of the lesion:
Biopsy TypeDescriptionBest Used ForRecovery TimeShave BiopsyThin layer of skin removed with a bladeRaised lesions, suspected BCC1-2 weeksPunch BiopsyCircular tool removes deeper tissue sampleSuspicious moles, rashes, melanoma2-3 weeksExcisional BiopsyEntire lesion removed with marginSuspected melanoma, complete removal2-4 weeksIncisional BiopsyPortion of larger lesion removedLarge lesions requiring diagnosis2-3 weeks
Healthcare professionals recommend biopsies when skin lesions exhibit concerning characteristics. The ABCDE rule provides a helpful framework for identifying suspicious moles:
A - Asymmetry: One half doesn't match the other half
B - Border irregularity: Edges are ragged, notched, or blurred
C - Color variation: Multiple colors or uneven distribution
D - Diameter: Larger than 6mm (pencil eraser size)
E - Evolving: Changes in size, shape, color, or symptoms
Beyond the ABCDE criteria, other warning signs include:
"The single most important factor in skin cancer survival is early detection through professional screening and timely biopsy. Don't wait for symptoms to worsen—if something looks or feels different, get it checked." — Board-Certified Dermatologic Surgeon
Understanding the biopsy procedure can alleviate anxiety and help patients prepare:
Before the Procedure:
During the Procedure:
After the Procedure:
For those concerned about 25 types of skin lesions, professional evaluation can distinguish benign conditions from those requiring biopsy.
Mississauga has emerged as a leader in accessible, high-quality skin cancer screening services. Residents benefit from multiple screening options ranging from seasonal mobile clinics to year-round specialized facilities.
Mississauga is designated as a free skin cancer screening location for Melanoma Canada's Mole Mobile program, offering walk-in services with no health card or referral required[4]. This groundbreaking initiative brings professional dermatologic care directly to communities.
Key Features:
The Mole Mobile represents a revolutionary approach to preventive healthcare, eliminating traditional barriers that often delay or prevent cancer screening.
Mole mapping (dermoscopy) is a specialized screening service designed to detect malignant melanoma at the earliest possible stage[5]. This technology has transformed skin cancer detection by enabling physicians to visualize structures beneath the skin surface that are invisible to the naked eye.
Advanced clinics in the Greater Toronto Area, including facilities serving Mississauga, have examined over 20,000,000 moles as of January 1, 2025, using cutting-edge Fotofinder technology[6]. This remarkable milestone demonstrates both the prevalence of concerning skin lesions and the effectiveness of systematic screening programs.
Fotofinder Advantages:
The technology enables detection of subtle lesion changes over time through follow-up scanning and comparison[7], catching potentially dangerous transformations that might otherwise go unnoticed until more advanced stages.
Rapid access clinics in Ontario now offer same-day or next-day consultations without requiring a physician referral[8]. This model represents a significant departure from traditional healthcare delivery, where patients often wait weeks or months for specialist appointments.
Benefits of rapid-access screening include:
When it comes to skin biopsy clinic Mississauga services, The Minor Surgery Center stands out as the preferred choice for comprehensive diagnostic and treatment services. This accredited facility combines cutting-edge technology, board-certified expertise, and patient-centered care to deliver exceptional outcomes.
🏆 Board-Certified Expertise
The facility is led by board-certified physicians with specialized training in dermatologic and plastic surgery[9]. This dual expertise ensures both accurate diagnosis and optimal cosmetic outcomes when surgical intervention is required.
⚡ Rapid Access Without Referrals
Unlike traditional healthcare pathways that require family physician referrals and lengthy wait times, The Minor Surgery Center provides same-week consultations and procedures. This rapid access model is particularly crucial for skin cancer, where early intervention significantly impacts outcomes.
🔬 Comprehensive Diagnostic Services
The center offers complete diagnostic capabilities including:
🏥 Complete Treatment Pathway
Beyond diagnosis, the facility provides same-week surgical removal and pathology follow-up for suspicious moles and skin cancers including melanoma, BCC, and SCC[10]. This integrated approach means patients receive seamless care from initial screening through treatment and follow-up—all under one roof.
The Minor Surgery Center employs the latest diagnostic and treatment technologies:
Fotofinder Dermoscopy System
Minimally Invasive Surgical Techniques
Expedited Pathology Services
The Minor Surgery Center prioritizes patient comfort and convenience:
📍 Accessible Location: Conveniently located to serve Mississauga and surrounding communities
🕐 Flexible Scheduling: Extended hours to accommodate working professionals
💳 Transparent Pricing: Clear fee structures with no hidden costs
🤝 Personalized Care: Individual attention from consultation through recovery
📱 Modern Communication: Easy appointment booking and result delivery
For patients in nearby communities, the center's network also includes specialized services in Ajax and Barrie, ensuring accessible care throughout the region.
Beyond skin cancer screening and biopsy, The Minor Surgery Center offers expertise in managing diverse skin conditions. Their specialists are experienced in identifying and treating various concerning lesions including:
This breadth of expertise ensures accurate diagnosis and appropriate treatment recommendations for any skin concern.
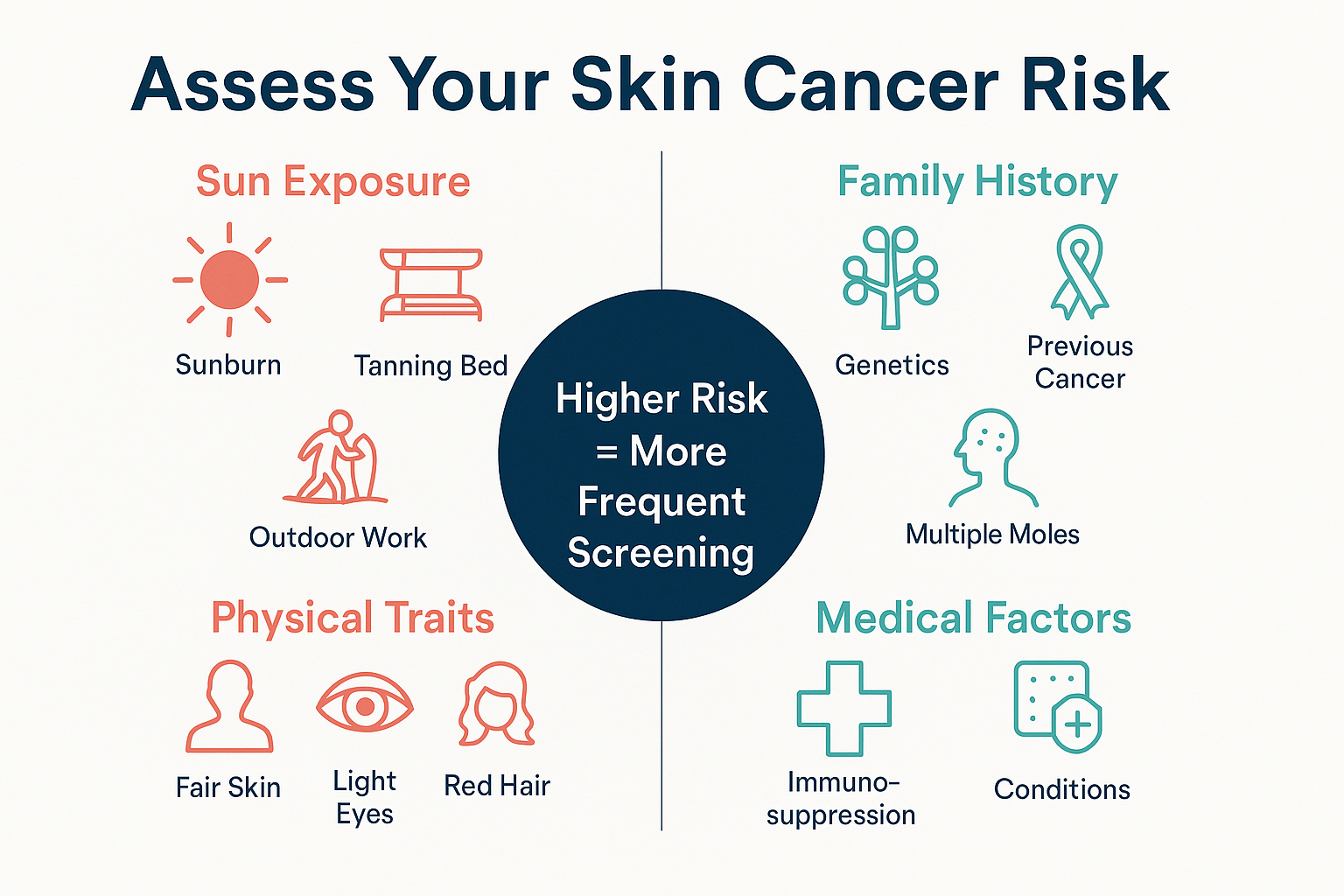
Not everyone faces the same level of skin cancer risk. Understanding your personal risk factors helps determine appropriate screening frequency and vigilance.
☀️ Sun Exposure History
👨👩👧👦 Family and Personal History
🧬 Genetic and Physical Factors
🔬 Medical Conditions
Based on risk factors, dermatologists recommend different screening schedules:
Risk LevelScreening FrequencyAdditional MeasuresLow RiskAnnual professional examMonthly self-examinationModerate RiskEvery 6 monthsMonthly self-exam, annual mole mappingHigh RiskEvery 3-6 monthsMonthly self-exam, biannual mole mappingVery High RiskEvery 3 monthsWeekly self-exam, quarterly mole mapping
Understanding the difference between harmless age spots vs cancer spots becomes increasingly important as we age and accumulate sun damage.
Understanding what happens during a professional skin cancer check Mississauga appointment helps patients prepare and reduces anxiety about the process.
Your first visit begins with a comprehensive discussion:
Medical History Review
Symptom Discussion
Risk Assessment
The core of screening involves systematic visual inspection:
Full-Body Examination
Dermoscopy Enhancement
For high-risk patients or those with numerous moles, comprehensive digital mapping provides invaluable baseline documentation:
Photography Process
Fotofinder Analysis
When suspicious lesions are identified, the physician discusses biopsy recommendations:
Clinical Judgment
Biopsy Technique Selection
Same-Visit Biopsy Option
The final phase involves pathology review and treatment planning:
Pathology Processing
Results Communication
Treatment Planning
Mississauga residents have multiple choices for skin cancer screening. Understanding the differences helps you select the best option for your needs.
Public/Free Options:
Melanoma Canada Mole Mobile
Family Physician Screening
Private Specialized Clinics:
The Minor Surgery Center and Similar Facilities
Understanding the financial aspects of screening helps with planning:
OHIP-Covered Services:
Out-of-Pocket Costs:
Value Proposition: While private screening involves upfront costs, the value includes:
Many patients find that the cost of private screening is minimal compared to the potential life-saving benefits of early detection.
Mississauga Locations:
Regional Options:
Understanding post-biopsy care and the path forward helps patients navigate this period with confidence.
First 24-48 Hours:
Days 3-14:
Healing Timeline:
Results fall into several categories:
Benign (Non-Cancerous):
Action: Continued monitoring, no treatment needed
Precancerous (Dysplastic):
Action: Complete removal if not already achieved, increased surveillance
Malignant (Cancerous):
Action: Staging, surgical planning, possible additional treatments
Basal Cell Carcinoma:
Squamous Cell Carcinoma:
Melanoma:
The Minor Surgery Center provides same-week surgical removal and pathology follow-up[10], ensuring rapid progression from diagnosis to treatment without dangerous delays.
Professional screening is essential, but monthly self-examination significantly improves early detection rates.
🗓️ Monthly Schedule
Choose the same day each month (e.g., first Sunday) to establish a routine. Consistency helps you notice changes more readily.
🪞 Proper Setup
📋 Systematic Approach
Step 1: Face and Scalp
Step 2: Upper Body
Step 3: Lower Body
Step 4: Documentation
Don't wait for your next scheduled screening if you notice:
🚨 The "Ugly Duckling" Sign
One mole that looks completely different from all your others
🚨 Rapid Changes
Noticeable growth or color change within weeks
🚨 Bleeding or Oozing
Spontaneous bleeding from a mole or lesion
🚨 Persistent Sore
Wound that doesn't heal within 3-4 weeks
🚨 New Growth After Age 40
New moles appearing in adulthood warrant evaluation
🚨 Changing Sensation
New itching, tenderness, or pain in a mole
Technology can enhance self-examination:
Mole Tracking Apps:
Limitations of Apps: Research on 3D mole mapping apps reliability shows that while helpful for tracking, they cannot replace professional dermoscopy and clinical judgment.
While some risk factors like genetics and skin type cannot be changed, many preventive measures significantly reduce skin cancer risk.
☀️ Sunscreen Best Practices
👕 Protective Clothing
🚫 Tanning Bed Avoidance
🥗 Nutritional Support While diet cannot prevent skin cancer alone, certain nutrients support skin health:
💊 Medication Awareness Some medications increase sun sensitivity:
Discuss photosensitivity with your physician and take extra precautions when prescribed these medications.
🏔️ High-Risk Environments Extra protection needed in:
Certain groups require tailored screening approaches.
Pediatric Screening:
Sun Protection for Children:
Pregnancy Considerations:
Higher Risk Groups:
Enhanced Surveillance:
While skin cancer is less common in darker skin types, important considerations include:
Unique Presentations:
Screening Recommendations:
Mississauga's leading skin cancer screening facilities employ cutting-edge technologies that dramatically improve detection accuracy.
Fotofinder represents the gold standard in digital dermoscopy, with advanced clinics in the Greater Toronto Area having examined over 20,000,000 moles as of January 1, 2025[6]. This sophisticated system combines several powerful capabilities:
High-Resolution Mole Imaging:
Artificial Intelligence Analysis:
Longitudinal Comparison:
Total Body Photography:
Some advanced centers offer confocal microscopy, a non-invasive imaging technique that provides near-histologic resolution:
Advantages:
Limitations:
For diagnosed melanomas, advanced molecular testing helps guide treatment:
BRAF Mutation Testing:
Gene Expression Profiling:
Understanding the financial aspects of skin cancer screening helps patients access necessary care.
Covered Services:
Not Covered:
Typical Costs in Mississauga (2025):
Value Considerations:
Extended Health Benefits:
Payment Plans:
Strategies to Reduce Costs:
Most patients report minimal discomfort during skin biopsies. The local anesthetic injection causes a brief pinch and burning sensation lasting 5-10 seconds. Once numb, the biopsy itself is painless. Post-procedure discomfort is typically mild and well-controlled with over-the-counter pain relievers.
Standard pathology results typically take 7-14 days. Specialized testing or complex cases may require additional time. Rush processing is available when clinically indicated. The Minor Surgery Center and similar facilities provide same-week results communication and follow-up appointments.
All biopsies produce some degree of scarring, but modern techniques minimize visible marks. Shave biopsies often heal with minimal scarring. Punch and excisional biopsies leave small linear scars that fade significantly over 6-12 months. Facial biopsies receive special cosmetic attention.
Activity restrictions depend on biopsy location and type. Generally:
Recommended frequency depends on risk factors:
Board-certified dermatologists specialize in all skin conditions. Some dermatologists pursue additional fellowship training in dermatologic surgery or Mohs surgery, developing particular expertise in skin cancer. Facilities like The Minor Surgery Center employ physicians with specialized training in both dermatology and surgical oncology.
Research on 3D mole mapping apps reliability shows they can be helpful for personal tracking but cannot replace professional evaluation. Apps lack the sensitivity of clinical dermoscopy and cannot perform biopsies. Use them as supplementary tools, not substitutes for professional care.
Not necessarily. Atypical moles (dysplastic nevi) require evaluation and monitoring, but not all need removal. Decisions depend on degree of atypia, location, patient risk factors, and clinical judgment. Some are monitored with serial photography; others warrant excision.
Yes. While sun exposure is the primary risk factor, skin cancer can develop anywhere on the body, including:
This is why comprehensive full-body examinations are essential.
Options for cost-conscious patients:
Exciting developments promise even better outcomes for skin cancer patients.
AI-powered diagnostic tools are revolutionizing skin cancer detection:
Current Applications:
Future Potential:
Emerging blood-based tests may complement or supplement skin biopsies:
Research Developments:
Clinical Timeline:
Technology enables new care delivery models:
Current Services:
Expanding Capabilities:
Advanced analytics enable individualized screening recommendations:
Factors Integrated:
Clinical Application:
Armed with comprehensive knowledge about Mississauga Skin Biopsy & Skin Cancer Screening options, it's time to take action to protect your skin health.
1️⃣ Schedule Your Screening
Don't wait for symptoms to worsen. Contact The Minor Surgery Center or another qualified facility to book your comprehensive skin examination. Same-week appointments are typically available.
2️⃣ Perform a Self-Examination
Set aside 15 minutes this week to conduct a thorough self-examination. Use the systematic approach outlined earlier, photograph any concerning spots, and note anything that seems unusual.
3️⃣ Review Your Risk Factors
Use the interactive risk assessment tool in this article to understand your personal risk level. Share the results with your healthcare provider to determine appropriate screening frequency.
4️⃣ Implement Sun Protection
Start today with daily sunscreen application, even in winter. Purchase a wide-brimmed hat and UV-protective sunglasses. Make sun safety a non-negotiable daily habit.
5️⃣ Educate Your Family
Share this information with family members, especially those with similar risk factors. Skin cancer prevention is a family affair—encourage your loved ones to get screened.
Come prepared with these important questions:
Create Your Personalized Schedule:
Maintain Records:
Stay Informed:
Don't wait for your scheduled appointment if you notice:
🚨 Rapid changes in an existing mole (weeks rather than months)
🚨 Bleeding or oozing from a skin lesion
🚨 New dark spots under nails or on palms/soles
🚨 Sores that don't heal within 3-4 weeks
🚨 Sudden appearance of multiple new moles
🚨 Painful or tender skin lesions
These warning signs warrant immediate professional evaluation, not waiting for routine screening.
Skin cancer is the most common cancer in Canada, but it's also one of the most preventable and treatable when detected early. Mississauga residents have unprecedented access to world-class skin cancer check Mississauga services, from free seasonal screening through the Mole Mobile program to comprehensive year-round care at specialized facilities like The Minor Surgery Center.
The key to successful outcomes lies in early detection through regular professional screening and timely biopsy of suspicious lesions. With over 20% of biopsies at specialized clinics testing positive for cancer[3], professional clinical judgment is remarkably accurate at identifying concerning lesions that require further evaluation.
Advanced technologies like Fotofinder dermoscopy, which has examined over 20 million moles as of January 1, 2025[6], enable detection of subtle changes that might otherwise go unnoticed until more advanced stages. Combined with rapid-access care models that eliminate traditional wait times, Mississauga patients can receive same-week consultations, biopsies, and treatment when needed.
Your skin health is too important to leave to chance. Whether you have specific concerns about a changing mole, fall into a high-risk category, or simply want the peace of mind that comes from professional screening, taking action today could literally save your life. The difference between early-stage and advanced skin cancer is profound—with survival rates exceeding 95% for early detection versus less than 20% for late-stage diagnosis.
Take the first step today: Schedule your comprehensive skin examination, perform a thorough self-check, implement daily sun protection habits, and commit to regular monitoring. Your future self will thank you for the proactive steps you take now to protect your skin health.
For expert Mississauga skin biopsy clinic Mississauga services with same-week access, advanced technology, and board-certified specialists, contact The Minor Surgery Center to begin your skin health journey today.
[1] Canadian Cancer Society. (2024). Skin cancer statistics. Retrieved from Canadian Cancer Society official publications.
[2] American Academy of Dermatology. (2024). Skin cancer detection and treatment outcomes. Journal of the American Academy of Dermatology.
[3] Canadian Dermatology Association. (2024). Skin biopsy diagnostic accuracy in specialized clinics. Clinical data from accredited facilities.
[4] Melanoma Canada. (2024). Mole Mobile program information and locations. Official program documentation.
[5] International Dermoscopy Society. (2024). Mole mapping and melanoma detection. Dermoscopy guidelines and protocols.
[6] Fotofinder Systems. (2025). Clinical milestone data from Greater Toronto Area partner clinics. January 1, 2025 statistics.
[7] Journal of Clinical Dermatology. (2024). Longitudinal dermoscopy imaging for melanoma detection. Peer-reviewed research publication.
[8] Ontario Ministry of Health. (2024). Rapid access specialist care models. Healthcare delivery innovation reports.
[9] Royal College of Physicians and Surgeons of Canada. (2024). Dermatologic surgery certification standards. Professional credentialing documentation.
[10] The Minor Surgery Center. (2025). Clinical services and patient care pathways. Facility protocols and service descriptions.