Every scar tells a story of healing, but sometimes that story takes an unexpected turn. While most scars fade quietly over time, some begin to change in ways that signal something more serious is happening beneath the surface. Whether it's a surgical scar that suddenly becomes raised and red, or an old injury mark that starts to darken and spread, understanding when to see a specialist about a changing scar can make the difference between early intervention and serious complications.
Scars are a natural part of the body's healing process, yet they don't always behave predictably. Changes in color, texture, size, or sensation can indicate normal healing—or they might be warning signs that require professional medical attention. This comprehensive guide will help you distinguish between typical scar evolution and concerning changes that warrant a specialist's evaluation.
Scar formation is a complex biological process that typically unfolds in predictable stages. During the initial inflammatory phase (lasting 3-5 days), the wound appears red, swollen, and potentially painful. The proliferative phase (3 days to 3 weeks) involves new tissue formation, while the remodeling phase can continue for 12-24 months or longer[1].
Normal scar changes during healing include:
These changes represent healthy healing and don't typically require specialist intervention. However, understanding this timeline helps identify when deviations occur.
Not all scar evolution follows the expected path. Certain changes indicate that the healing process has gone awry or that new problems have developed. Problematic scar changes that warrant concern include:
Warning SignWhat It May IndicateUrgency LevelRapid expansion beyond original woundKeloid or hypertrophic scarringModerate - Schedule appointment within 2-4 weeksDarkening or multiple colors appearingPossible melanoma or skin cancerHigh - Seek evaluation within 1-2 weeksPersistent or increasing painNerve involvement, infection, or other complicationsModerate to High - Depends on severityBleeding or oozing without traumaInfection or malignancyHigh - Seek prompt evaluationHardening with restricted movementContracture formationModerate - Important for functionNew lumps or nodules within scarCyst formation, granuloma, or tumorModerate - Requires assessment
Understanding these distinctions is crucial for knowing when to see a specialist about a changing scar. The Minor Surgery Center specializes in evaluating and treating concerning skin changes and scar complications.
Color is one of the most noticeable aspects of any scar, and changes in pigmentation can signal various underlying issues. While gradual lightening is normal, certain color changes demand professional attention.
🚨 Red Flag Color Changes:
For those concerned about distinguishing between normal skin changes and potentially cancerous lesions, learning about different types of skin cancer can provide valuable context.
Scars that change in size or shape after the initial healing period deserve careful attention. While some contraction is normal during the first year, certain growth patterns are concerning.
When size changes matter:
Keloid formation is more common in certain populations and body locations. The chest, shoulders, earlobes, and upper back are particularly prone to keloid development. People with darker skin tones have a higher genetic predisposition to keloid formation[3].
The surface characteristics of a scar provide important diagnostic clues. Smooth scars that develop unusual textures warrant investigation.
Concerning textural changes include:
Understanding various types of skin lesions helps contextualize these changes within the broader spectrum of skin conditions.
Physical sensations associated with scars often provide early warning signs of problems. While some numbness or tingling is normal initially, certain sensory changes require attention.
Symptoms requiring specialist evaluation:
Scars that restrict movement or interfere with normal function require prompt specialist attention, especially when these limitations worsen over time.
Functional problems include:
Certain scar changes constitute medical emergencies requiring immediate specialist consultation. Don't wait if you notice:
These symptoms may indicate serious infections like cellulitis or abscess formation that require urgent intervention.
Schedule an appointment within one to two weeks if you observe:
These changes may indicate developing complications that benefit from early treatment. For residents seeking specialized care, the best skin cancer clinic in Toronto offers comprehensive scar and skin lesion evaluation.
While not emergencies, these changes merit professional assessment within a month or two:
Even if changes seem minor, professional evaluation provides peace of mind and establishes baseline documentation for future comparison.
Some scars require ongoing surveillance even without active changes:
Certain medical conditions and personal history elements increase the importance of early specialist evaluation for changing scars.
High-risk medical histories:
Where a scar is located and how it formed influences when specialist evaluation becomes necessary.
High-priority locations:
High-risk scar types:
Age, ethnicity, and family history influence scar behavior and cancer risk.
Populations requiring lower threshold for evaluation:
Understanding these risk factors helps determine when to see a specialist about a changing scar, even for seemingly minor changes.
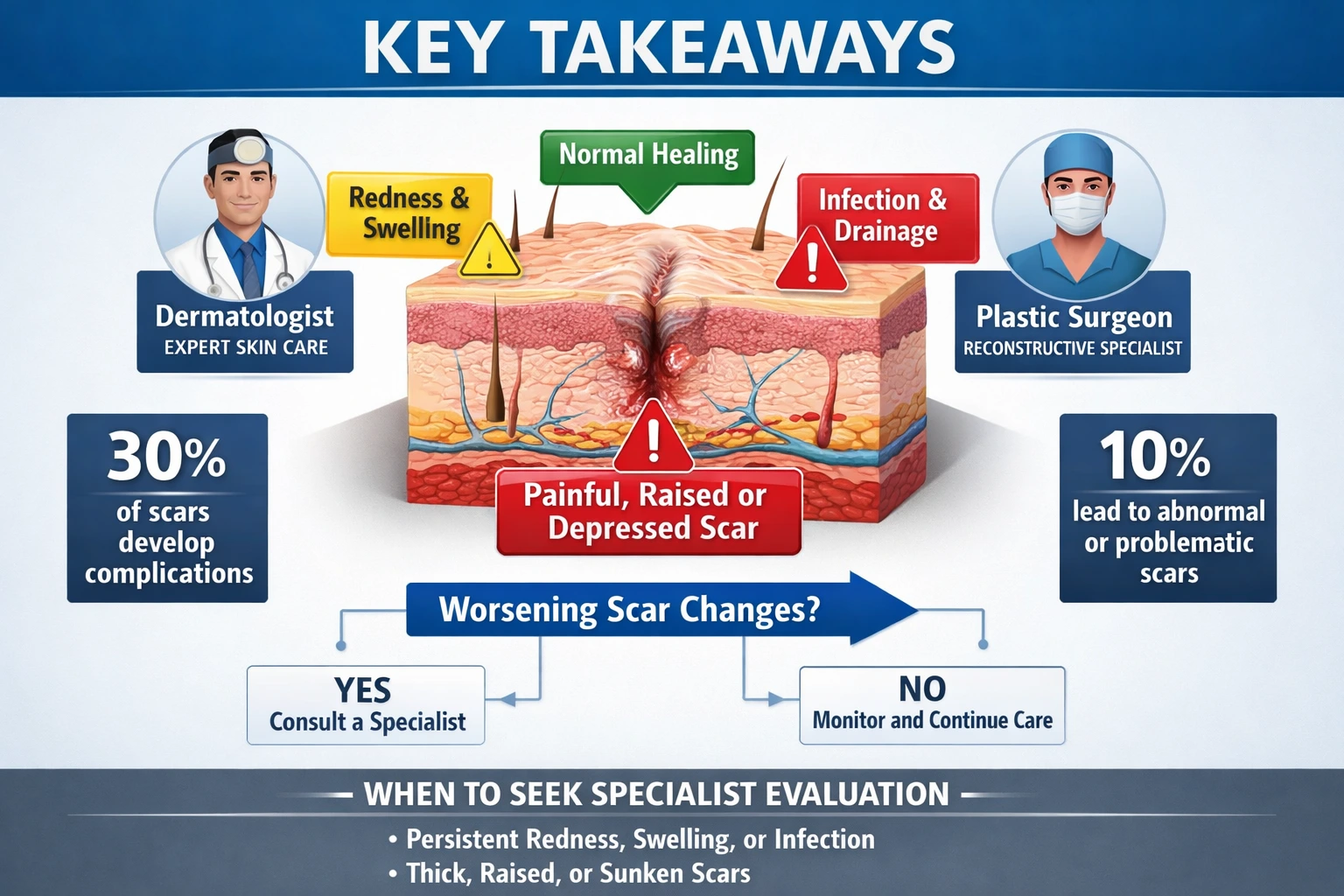
Different specialists bring unique expertise to scar evaluation and management. Understanding which specialist to see can streamline your care.
Dermatologists are often the first-line specialists for scar evaluation. They diagnose skin conditions, perform biopsies, and treat many scar-related problems medically. Dermatologists excel at identifying malignant changes and managing keloids, hypertrophic scars, and pigmentation issues.
Plastic surgeons specialize in scar revision and reconstruction. They're ideal for functional impairments, contractures, and cosmetic concerns. Plastic surgeons perform advanced surgical techniques to improve scar appearance and function.
Surgical oncologists or Mohs surgeons are essential when skin cancer is suspected or confirmed. They specialize in cancer removal with tissue-sparing techniques and reconstruction.
Wound care specialists manage complex, non-healing wounds and problematic scars related to chronic conditions like diabetes or vascular disease.
For comprehensive scar and skin lesion evaluation, specialized centers like those offering mole and cyst removal in Ajax or Barrie provide expert assessment and treatment.
A thorough scar evaluation typically includes several components:
1. Detailed History Taking
The specialist will ask about:
2. Physical Examination
The specialist will carefully examine:
3. Dermoscopy
Many specialists use a dermatoscope—a specialized magnifying device with lighting—to examine skin structures not visible to the naked eye. This non-invasive technique helps identify concerning features suggesting malignancy.
4. Photography
Documentation through medical photography creates a baseline for monitoring future changes. Serial photographs over time reveal subtle progression that might otherwise go unnoticed.
5. Biopsy (If Indicated)
When examination raises concerns about infection, abnormal healing, or malignancy, the specialist may recommend a biopsy. This involves removing a small tissue sample for microscopic examination. Biopsy types include:
Being prepared with questions ensures you get maximum value from your consultation:
Essential questions:
Many changing scars respond well to non-invasive or minimally invasive treatments.
Topical Treatments:
Intralesional Injections:
Pressure Therapy:
Custom pressure garments worn over scars can prevent and treat hypertrophic scarring, especially after burns. Consistent wear (23 hours daily) for 6-12 months yields best results.
Advanced laser technologies offer effective scar treatment with minimal downtime.
Laser options include:
Multiple treatment sessions spaced 4-6 weeks apart typically produce optimal results.
When conservative measures fail or aren't appropriate, surgical options may be necessary.
Surgical techniques:
Mohs micrographic surgery represents the gold standard for removing skin cancers in scars, offering tissue-sparing precision with the highest cure rates.
Low-dose radiation following keloid excision significantly reduces recurrence rates. This treatment is typically reserved for resistant keloids in locations where other treatments have failed.
Research continues to develop new scar treatment modalities:
The best treatment for problematic scars is prevention. Proper initial wound care significantly influences long-term outcomes.
Evidence-based wound care principles:
✅ Keep wounds clean and moist: Moist wound healing promotes faster closure with less scarring ✅ Protect from sun exposure: UV radiation darkens scars and increases cancer risk ✅ Avoid tension on healing wounds: Minimize stress on wound edges during the first 2-3 weeks ✅ Don't pick or scratch: Disrupting healing tissue worsens scarring ✅ Follow post-operative instructions: Surgeons provide specific care protocols for optimal healing ✅ Maintain good nutrition: Adequate protein, vitamins C and A, and zinc support healing
UV exposure represents one of the most significant modifiable risk factors for problematic scar changes, including malignant transformation.
Comprehensive sun protection includes:
Scars lack normal melanin protection and are particularly vulnerable to UV damage for at least 12-18 months after formation.
Regular self-examination helps detect changes early when treatment is most effective.
Effective scar monitoring:
📸 Take monthly photos: Use consistent lighting and angles to track subtle changes 🔍 Use the ABCDE method: Asymmetry, Border irregularity, Color variation, Diameter >6mm, Evolution (changes over time) 📝 Keep a scar diary: Note symptoms, size, color, and texture monthly 📅 Schedule regular check-ups: Annual or more frequent professional examinations based on risk factors 👥 Enlist help: Ask family members to check hard-to-see locations
Overall health significantly impacts scar formation and behavior.
Health optimization strategies:
Scars from skin cancer excision require special attention due to recurrence risk. Even after successful treatment, cancer can return in or near the original site.
Monitoring guidelines for cancer removal scars:
Any change in these scars—new lumps, color changes, bleeding, or non-healing areas—requires prompt evaluation. The recurrence risk varies by cancer type, with melanoma having the highest concern level.
Burn scars present unique challenges and risks. Deep burns (second and third degree) create scars prone to contractures, hypertrophic scarring, and long-term malignant transformation.
Marjolin's ulcer—squamous cell carcinoma arising in chronic burn scars—typically develops decades after the original injury. Any non-healing area, new growth, or persistent ulceration in a burn scar requires immediate biopsy[4].
Burn scar management often requires:
Most surgical scars heal uneventfully, but certain procedures carry higher risk for problematic scarring:
Surgical technique, wound closure method, and post-operative care all influence outcomes. Following surgeon-specific instructions optimizes results.
Scars from accidents, injuries, or violence may contain foreign material (dirt, glass, metal) that causes ongoing inflammation or infection. Retained foreign bodies increase infection risk and can trigger granuloma formation.
Warning signs of foreign body reactions:
Imaging studies (X-ray, ultrasound, or CT scan) can identify retained material requiring removal.
Scars, especially visible ones, carry psychological weight beyond their physical presence. When scars change unexpectedly, anxiety and distress often intensify.
Common emotional responses include:
These psychological impacts are valid and deserve attention. Mental health support, including therapy and support groups, can be valuable components of comprehensive scar care.
While not all scar changes are medically dangerous, significant cosmetic concerns constitute legitimate reasons for specialist evaluation. Quality of life matters, and treatments that improve appearance can profoundly impact well-being.
Cosmetic consultation is appropriate when:
Specialists can offer realistic expectations about what improvements are achievable and recommend appropriate treatments.
Insurance coverage for scar treatment depends on medical necessity versus cosmetic purposes.
Generally covered situations:
Generally not covered:
Gray areas include keloid treatment and scar revision that combines functional and cosmetic benefits. Pre-authorization and documentation of medical necessity improve coverage chances.
For self-pay patients or uncovered treatments, understanding typical costs helps with planning:
Treatment TypeTypical Cost Range (CAD)Specialist consultation$150-$400Biopsy$200-$600Corticosteroid injections$100-$300 per sessionLaser treatment (per session)$300-$1,500Topical silicone products$30-$100 per monthMinor scar revision$1,000-$3,000Complex scar reconstruction$5,000-$15,000+
Costs vary significantly based on location, specialist expertise, and treatment complexity. Many practices offer payment plans for out-of-pocket expenses.

Situation: A 58-year-old woman noticed her 3-year-old abdominal surgery scar gradually darkening over 6 months. Initially pink and flat, the scar developed irregular brown and black areas with uneven borders.
Action: She consulted a dermatologist who performed dermoscopy, revealing atypical pigment patterns. A punch biopsy confirmed melanoma in situ.
Outcome: Early detection allowed complete excision with clear margins. The patient now undergoes full-body skin examinations every 6 months.
Lesson: Darkening scars, especially with irregular pigmentation, require prompt evaluation even years after formation.
Situation: A 22-year-old man developed a keloid on his earlobe following ear piercing. Despite initial corticosteroid injections, the keloid continued growing over 18 months, becoming painful and cosmetically distressing.
Action: A plastic surgeon recommended surgical excision combined with immediate post-operative radiation therapy.
Outcome: The keloid was removed, and low-dose radiation prevented recurrence. Two years later, the ear shows minimal scarring with no keloid return.
Lesson: Resistant keloids often require multimodal treatment. Early specialist intervention improves outcomes.
Situation: A 65-year-old man with a 40-year-old burn scar on his leg noticed a small area that wouldn't heal for 3 months. The area occasionally bled and developed a crusty surface.
Action: Concerned about Marjolin's ulcer, his physician performed a biopsy confirming squamous cell carcinoma.
Outcome: Wide excision with skin grafting achieved clear margins. The patient now has regular skin cancer surveillance.
Lesson: Non-healing areas in old burn scars require immediate evaluation due to malignant transformation risk.
How long should I wait before seeing a specialist about scar changes?
The timeline depends on the specific changes. Bleeding, severe pain, or signs of infection warrant immediate evaluation (24-48 hours). Color changes, new lumps, or rapid growth should be assessed within 1-2 weeks. Gradual changes or cosmetic concerns can be addressed within 4-6 weeks. When uncertain, earlier evaluation is always safer.
Can old scars suddenly become cancerous?
Yes, though it's uncommon. Scars can develop skin cancer years or even decades after formation, particularly burn scars, radiation scars, and chronic wound scars. This phenomenon, called Marjolin's ulcer when occurring in burn scars, typically presents as squamous cell carcinoma. Any change in a long-standing scar deserves evaluation.
Are raised, red scars always keloids?
No. Hypertrophic scars are also raised and red but remain within the original wound boundaries, while keloids extend beyond. Both conditions result from excessive collagen production during healing. Hypertrophic scars often improve over 12-18 months, while keloids rarely resolve without treatment and may continue growing.
Will insurance cover treatment for my changing scar?
Coverage depends on medical necessity. Treatments for infection, cancer, pain, or functional impairment are typically covered. Purely cosmetic treatments usually aren't. Documentation of symptoms and functional limitations improves coverage likelihood. Check with your insurance provider about specific coverage criteria.
What's the difference between a dermatologist and a plastic surgeon for scar treatment?
Dermatologists specialize in diagnosing and medically treating skin conditions, including biopsies, injections, and laser treatments. Plastic surgeons focus on surgical scar revision and reconstruction. Many scar problems benefit from collaboration between both specialties. Start with the specialist whose expertise best matches your primary concern.
Can I prevent my scar from changing?
While you can't control all factors, proper care reduces risks. Protect scars from sun exposure, keep them moisturized, avoid trauma, and maintain overall health. For high-risk scars (after cancer removal or severe burns), regular monitoring enables early detection of changes. Preventive measures work best when started immediately after injury or surgery.
Locating a qualified specialist experienced in scar evaluation and treatment is crucial. Consider these resources:
Staying informed about scar health empowers better self-advocacy:
The Minor Surgery Center blog provides evidence-based information about various skin conditions, scar management, and treatment options.
Seeking a second opinion is appropriate when:
Second opinions often provide reassurance or reveal alternative approaches worth considering.
Understanding when to see a specialist about a changing scar empowers you to protect your health while avoiding unnecessary anxiety about normal healing. Most scar changes represent typical maturation, but certain warning signs demand professional attention.
Remember these key principles:
🔍 Know the warning signs: Rapid growth, darkening, bleeding, pain, or functional impairment warrant evaluation
⏰ Act promptly on concerning changes: Early intervention improves outcomes for both medical and cosmetic scar problems
📋 Consider your risk factors: Personal history, scar type, and location influence when specialist consultation becomes necessary
👨⚕️ Choose the right specialist: Match your primary concern (medical vs. cosmetic vs. functional) with appropriate expertise
📸 Monitor systematically: Regular self-examination and documentation help detect subtle changes early
🛡️ Practice prevention: Sun protection, proper wound care, and overall health optimization reduce problematic scar development
If you're concerned about a changing scar:
Don't let uncertainty or fear delay necessary evaluation. While most scar changes are benign, early detection of serious problems dramatically improves treatment success. Your health and peace of mind are worth the investment in professional assessment.
For comprehensive evaluation of concerning skin changes, scars, or lesions, specialized centers provide expert care with advanced diagnostic and treatment capabilities. Taking action today protects your health tomorrow.
Remember: when in doubt about any scar change, professional evaluation is always the safest choice. Trust your instincts—if something seems wrong, it deserves attention from a qualified specialist who can provide accurate diagnosis and appropriate treatment recommendations.
[1] Gurtner GC, Werner S, Barrandon Y, Longaker MT. Wound repair and regeneration. Nature. 2008;453(7193):314-321.
[2] Kovalyshyn I, Doherty SD, Franks AG Jr. Melanoma arising in a surgical scar: a case report and review of the literature. Dermatol Surg. 2008;34(5):674-677.
[3] Berman B, Maderal A, Raphael B. Keloids and Hypertrophic Scars: Pathophysiology, Classification, and Treatment. Dermatol Surg. 2017;43 Suppl 1:S3-S18.
[4] Chalya PL, Mabula JB, Rambau P, et al. Marjolin's ulcers at a university teaching hospital in Northwestern Tanzania: a retrospective review of 56 cases. World J Surg Oncol. 2012;10:38.