Imagine experiencing chronic lower back pain that radiates down your legs, accompanied by unexplained bladder issues and numbness in your saddle region—only to be told by multiple doctors that nothing appears wrong. For thousands of people living with Tarlov cysts, this frustrating scenario represents their reality. These fluid-filled sacs that develop along nerve roots in the spine often go undiagnosed for years, leaving patients struggling to understand why conventional treatments fail to provide relief. Understanding Tarlov Cysts: When Spinal Cysts Cause Back and Leg Pain (and When to Treat Them) can be the key to finally getting the right diagnosis and appropriate care for this often-overlooked neurological condition.

Tarlov cysts, also known as perineural cysts or sacral nerve root cysts, are abnormal fluid-filled sacs that develop between the layers of tissue covering nerve roots near the spine. First described by neurosurgeon Isadore Tarlov in 1938, these cysts represent a unique type of spinal pathology that differs significantly from other types of cysts found elsewhere in the body.
These cysts form within the nerve root sheath—the protective covering surrounding spinal nerve roots as they exit the spinal canal. Unlike simple cysts that contain only fluid, Tarlov cysts have walls that incorporate actual nerve fibers, which explains why they can cause such significant neurological symptoms when they enlarge.
The cysts fill with cerebrospinal fluid (CSF), the same clear liquid that bathes the brain and spinal cord. Through a one-way valve mechanism, fluid can enter the cyst but has difficulty draining back out, causing the cyst to gradually expand over time like a slowly inflating balloon.
Location matters tremendously with Tarlov cysts. The vast majority (approximately 90%) occur in the sacral region of the spine—specifically at the S2 and S3 nerve root levels. This area sits at the base of the spine, just above the tailbone.
Less commonly, Tarlov cysts can develop in:
The sacral predominance has significant clinical implications because nerves in this region control critical functions including bladder and bowel function, sexual function, and sensation in the pelvic region and legs.
Research suggests that Tarlov cysts affect approximately 4-9% of the general population, though the actual prevalence may be higher since many cases remain undiagnosed. Women appear to be affected more frequently than men, with some studies showing a 3:1 female-to-male ratio.
Several factors may contribute to Tarlov cyst formation:
Risk FactorDescriptionCongenital predispositionSome people may be born with weakness in nerve sheath tissuesTraumaSpinal injuries or repetitive stress may trigger cyst developmentInflammationChronic inflammation around nerve roots may weaken protective coveringsIncreased CSF pressureConditions that elevate spinal fluid pressure may promote cyst expansionConnective tissue disordersConditions affecting tissue strength may increase susceptibility
The challenge with Tarlov cysts lies in their variable presentation. Many people harbor these cysts without ever experiencing symptoms, while others develop debilitating pain and neurological complications. Understanding Tarlov Cysts: When Spinal Cysts Cause Back and Leg Pain (and When to Treat Them) requires recognizing the full spectrum of possible symptoms.
Lower back pain represents the most frequent complaint among symptomatic patients. This pain typically:
Leg pain (sciatica) occurs when enlarged cysts compress sacral nerve roots. Patients describe:
Beyond pain, Tarlov cysts can produce a constellation of neurological symptoms that significantly impact quality of life:
Sensory changes:
Motor symptoms:
Autonomic dysfunction:
Interestingly, some patients with Tarlov cysts experience positional headaches that worsen when upright and improve when lying flat. This occurs because CSF leaking into the cyst reduces overall CSF volume, creating low-pressure headaches similar to those seen after spinal taps.
Recognizing what makes symptoms worse can provide important diagnostic clues:
Activities that typically worsen symptoms:
Factors that may provide relief:
Accurate diagnosis of Tarlov cysts requires both sophisticated imaging and careful clinical correlation. Many cysts are discovered incidentally during imaging performed for other reasons, creating the challenge of determining whether the cyst is actually causing the patient's symptoms.
Magnetic Resonance Imaging (MRI) represents the definitive diagnostic tool for Tarlov cysts. Unlike X-rays or CT scans, MRI provides superior soft tissue contrast that clearly visualizes:
The radiologist will note specific characteristics:
Key MRI findings:
The difficulty with Tarlov cyst diagnosis stems from several factors:
1. Asymptomatic cysts are common - Finding a cyst doesn't automatically mean it's causing symptoms. Correlation with clinical presentation is essential.
2. Symptoms overlap with other conditions:
3. Multiple cysts may be present - Determining which cyst (if any) is symptomatic can be challenging.
A thorough neurological examination helps establish the connection between imaging findings and symptoms:
Examination components:
When diagnosis remains uncertain, additional tests may help:
CT myelography: Involves injecting contrast dye into the spinal canal before CT scanning. This can demonstrate CSF communication with the cyst and provide detailed bone anatomy.
Diagnostic cyst aspiration: In select cases, temporarily draining fluid from the cyst under imaging guidance can help determine if it's the pain source. If symptoms improve after aspiration, it supports the cyst as the culprit.
Electromyography (EMG) and nerve conduction studies: These tests assess nerve function and can identify which specific nerves are affected, helping correlate symptoms with cyst location.
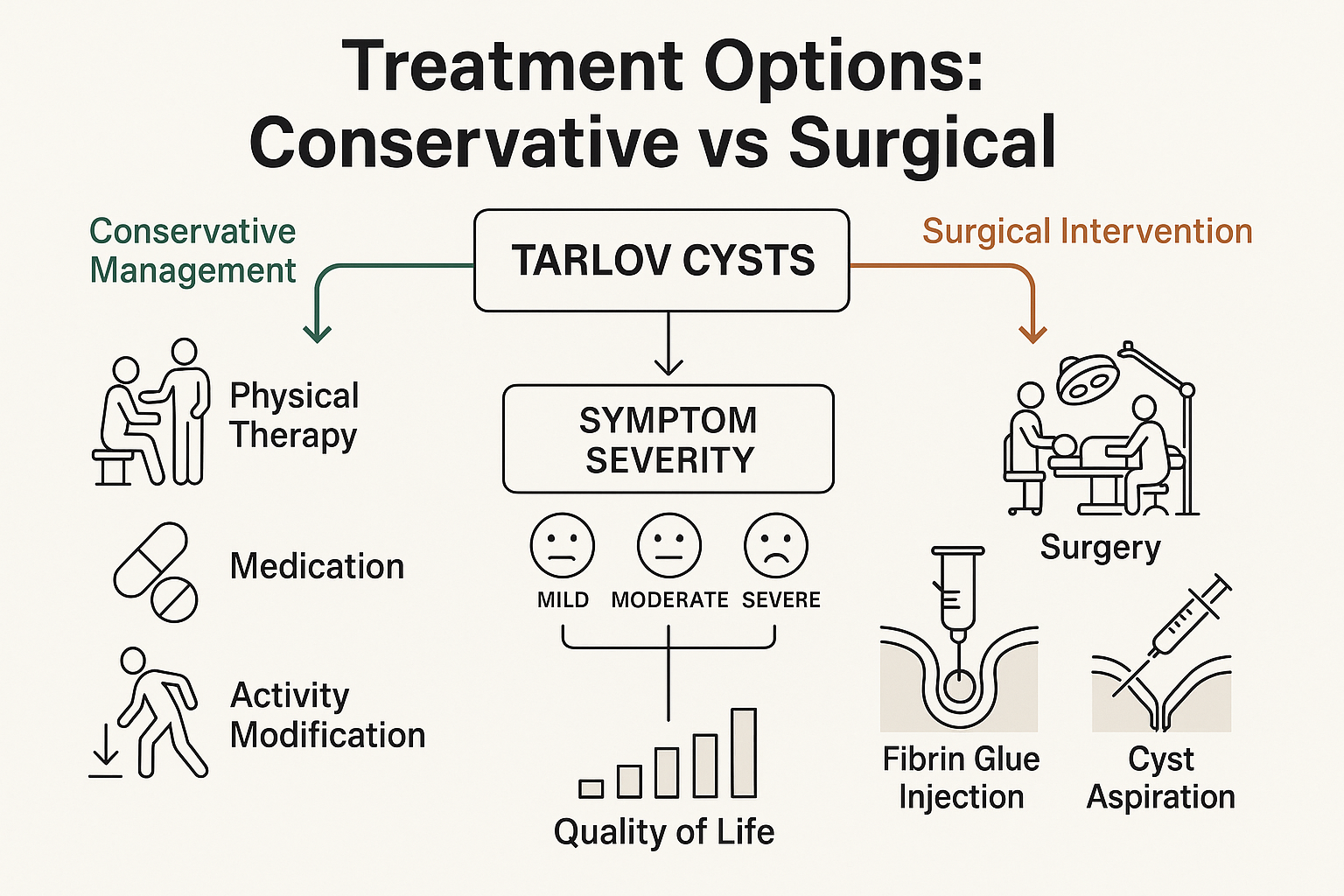
For most patients with symptomatic Tarlov cysts, conservative (non-surgical) management represents the appropriate initial approach. Understanding Tarlov Cysts: When Spinal Cysts Cause Back and Leg Pain (and When to Treat Them) includes knowing that surgery should be reserved for cases where conservative measures fail.
Strategic activity modification forms the cornerstone of managing Tarlov cyst symptoms. The goal is to reduce activities that increase cyst pressure while maintaining overall function and quality of life.
Recommended modifications:
✅ Sitting strategies:
✅ Movement patterns:
✅ Sleep positioning:
Critical understanding: Certain exercises can significantly worsen Tarlov cyst symptoms by increasing intracranial pressure or placing excessive stress on the sacral region.
High-risk exercises to avoid:
❌ Valsalva-inducing activities:
❌ High-impact activities:
❌ Positions that increase sacral pressure:
❌ Activities that jar the spine:
Low-impact activities can maintain fitness without aggravating symptoms:
✅ Swimming and water aerobics (excellent options) ✅ Walking on soft surfaces (grass, track, treadmill) ✅ Gentle yoga (modified poses, avoid deep flexion) ✅ Tai chi ✅ Stationary cycling with proper positioning (short duration) ✅ Upper body strength training (seated, supported)
Specialized physical therapy can provide significant benefit when tailored to Tarlov cyst patients:
Therapeutic interventions:
Similar to approaches used for other nerve-related conditions, physical therapy should progress gradually and avoid aggravating positions.
Medication options for symptom control:
Over-the-counter:
Prescription medications:
Non-pharmacological approaches:
When conservative measures provide insufficient relief, minimally invasive procedures may offer temporary symptom control:
Epidural steroid injections: Can reduce inflammation around affected nerve roots, though effectiveness for Tarlov cysts specifically remains debated.
Nerve blocks: Selective nerve root blocks may provide diagnostic information and temporary relief.
Important note: These procedures don't address the cyst itself but may help manage associated inflammation and pain while determining if more definitive treatment is needed.
While most Tarlov cyst patients can manage symptoms conservatively, some develop progressive neurological deficits or intractable pain that significantly impairs quality of life. For these individuals, surgical intervention may become necessary.
Surgery for Tarlov cysts should be considered when:
Absolute indications:
Relative indications:
Poor surgical candidates:
Several surgical approaches exist for Tarlov cyst treatment, each with specific advantages and limitations:
1. Cyst Fenestration and Nerve Root Decompression
This procedure involves:
Advantages: Relatively straightforward, addresses compression Limitations: High recurrence rate (cysts often refill)
2. Cyst Imbrication with Fibrin Glue
The most commonly performed technique:
Advantages: Lower recurrence rates, preserves nerve function Limitations: Technically demanding, requires specialized materials
3. Cyst Excision
Complete removal of the cyst:
Advantages: Definitive treatment, lowest recurrence Limitations: Higher risk of nerve damage, more extensive surgery
4. Cyst-Peritoneal Shunt
Creating a drainage pathway:
Advantages: Avoids extensive dissection Limitations: Hardware complications, shunt malfunction possible
Expected outcomes vary based on several factors:
Success rates:
Factors affecting outcomes:
As with any spinal surgery, Tarlov cyst procedures carry potential risks:
Common complications:
Serious but rare complications:
Long-term considerations:
Typical recovery timeline:
Immediate post-operative (0-2 weeks):
Early recovery (2-6 weeks):
Intermediate recovery (6-12 weeks):
Long-term (3-6 months):
Whether managing symptoms conservatively or recovering from surgery, patients with Tarlov cysts benefit from comprehensive long-term strategies that address physical, emotional, and practical aspects of this chronic condition.
Successful long-term management requires individualized approaches:
Key components:
📋 Regular monitoring:
📋 Lifestyle adaptations:
📋 Support systems:
Many Tarlov cyst patients face challenges maintaining employment, particularly in physically demanding jobs:
Workplace strategies:
✅ Job modifications:
✅ Legal protections:
Women with Tarlov cysts face unique concerns regarding pregnancy:
Potential challenges:
Management recommendations:
Chronic pain and neurological symptoms significantly impact mental health:
Common psychological challenges:
Supportive interventions:
The field of Tarlov cyst management continues to evolve:
Areas of active research:
Investigational treatments:
Certain symptoms require urgent evaluation:
🚨 Emergency warning signs:
These symptoms may indicate cauda equina syndrome or other serious complications requiring immediate intervention.
Accurate diagnosis becomes critical because Tarlov cyst symptoms overlap significantly with other spinal and pelvic conditions. Understanding these distinctions helps ensure appropriate treatment.
Herniated disc:
Spinal stenosis:
Arachnoiditis:
Many Tarlov cyst symptoms mimic pelvic conditions:
Pudendal neuralgia:
Interstitial cystitis:
Endometriosis (in women):
Given the complexity of symptoms, patients often benefit from multidisciplinary evaluation involving:
Similar to how skin lesions require expert evaluation to distinguish benign from concerning findings, spinal cysts need specialized assessment to determine clinical significance.
Tarlov cysts represent a relatively uncommon condition, and not all spine specialists have extensive experience treating them. Finding knowledgeable providers significantly impacts outcomes.
Ideal specialist characteristics:
🔍 Experience with Tarlov cysts specifically:
🔍 Surgical expertise (if considering surgery):
🔍 Comprehensive approach:
Important questions before treatment decisions:
Given the complexity of Tarlov cyst management, second opinions are often valuable:
When to seek additional input:
Helpful organizations and resources:
Tarlov Cyst Disease Foundation:
Online support communities:
Medical literature:
For those seeking comprehensive care for various conditions, facilities like The Minor Surgery Center demonstrate the importance of specialized expertise, though Tarlov cyst treatment typically requires neurosurgical or spine surgery specialists rather than minor surgery centers.
Understanding Tarlov Cysts: When Spinal Cysts Cause Back and Leg Pain (and When to Treat Them) empowers patients to make informed decisions about their care and advocate effectively for appropriate treatment. While these perineural cysts can cause significant symptoms ranging from chronic back and leg pain to bladder dysfunction and neurological deficits, many patients successfully manage their condition through conservative approaches including activity modification, physical therapy, and pain management strategies.
The key to optimal outcomes lies in accurate diagnosis, appropriate treatment selection, and realistic expectations. Not every Tarlov cyst requires treatment—many remain asymptomatic throughout a person's lifetime. For symptomatic cysts, conservative management should be tried first, with surgery reserved for patients with progressive neurological symptoms or severe, treatment-resistant pain that significantly impacts quality of life.
If you suspect you may have Tarlov cysts or have been recently diagnosed:
✅ Step 1: Obtain proper imaging - Request an MRI of your lumbar and sacral spine if you have unexplained lower back pain, leg pain, or bladder/bowel symptoms.
✅ Step 2: Find an experienced specialist - Seek evaluation from a neurosurgeon or spine surgeon with specific Tarlov cyst experience rather than general spine practitioners.
✅ Step 3: Start conservative management - Work with physical therapists and pain specialists to develop a comprehensive conservative treatment plan, including identifying exercises to avoid with Tarlov cysts.
✅ Step 4: Track your symptoms - Keep a detailed journal of pain patterns, neurological symptoms, and functional limitations to help guide treatment decisions.
✅ Step 5: Connect with support - Join patient support groups to learn from others' experiences and reduce the isolation that often accompanies this condition.
✅ Step 6: Consider surgery only when appropriate - If conservative measures fail after adequate trial (typically 6-12 months) and symptoms significantly impair your quality of life, discuss surgical options with your specialist.
✅ Step 7: Advocate for yourself - Don't accept dismissive responses from healthcare providers. Tarlov cysts can cause real, significant symptoms that deserve appropriate evaluation and treatment.
Remember that living with Tarlov cysts requires patience, persistence, and partnership with knowledgeable healthcare providers. While this condition presents challenges, many patients achieve significant symptom improvement and maintain good quality of life through appropriate management strategies tailored to their individual situation.
The journey from diagnosis to effective management may be long, but understanding your condition, knowing your options, and working with experienced specialists provides the best foundation for optimal outcomes. Whether your path involves conservative management, surgical intervention, or a combination of approaches, taking an active role in your care decisions and maintaining realistic expectations will serve you well in managing Tarlov Cysts: When Spinal Cysts Cause Back and Leg Pain (and When to Treat Them).
For additional information on various medical conditions and treatment approaches, visit The Minor Surgery Center's blog for educational resources on a wide range of health topics.