Solar keratosis represents a fundamental change in your skin cells after prolonged ultraviolet (UV) radiation exposure. These aren't just cosmetic concerns—they're actual cellular transformations that deserve your attention.
When UV rays penetrate your skin over months and years, they damage the DNA in keratinocytes (the primary cells in your skin's outer layer). This damage accumulates, eventually causing these cells to grow abnormally. The result? Those rough, scaly patches that feel different from the surrounding skin.
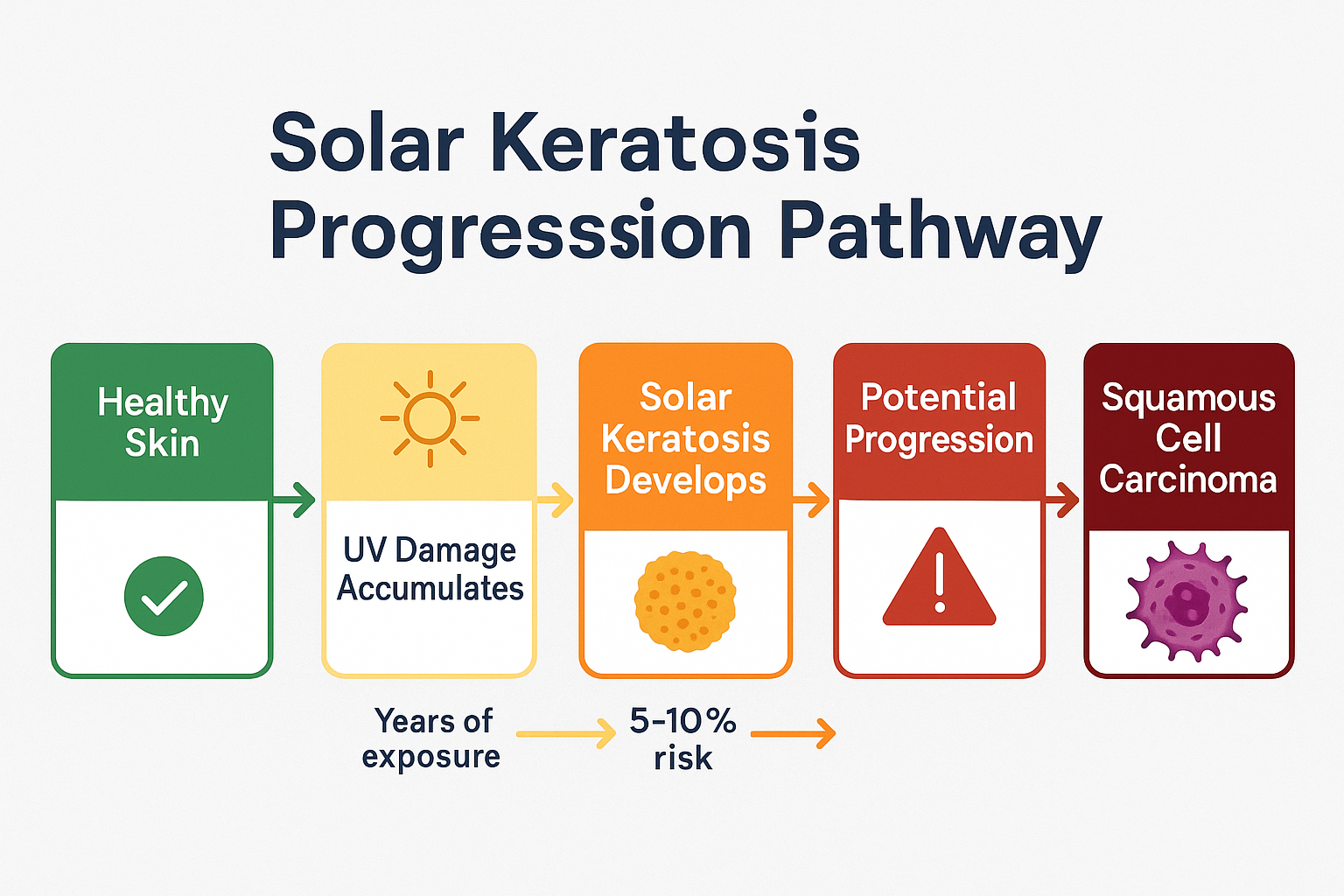
The medical community considers solar keratosis a "precancerous" or "pre-malignant" condition. This doesn't mean you have cancer—it means the affected cells have changed in ways that could potentially lead to cancer if left untreated.[1]
You might hear these lesions called by different names:
All three terms describe the same condition. We'll use them interchangeably throughout this article, just as healthcare professionals do in practice.
Solar keratosis is remarkably prevalent, especially in certain populations:
If you've discovered a solar keratosis, you're far from alone. This is one of the most frequent reasons people visit dermatologists and skin specialists.
Recognizing solar keratosis early gives you the best chance for simple, effective treatment. These lesions have distinctive characteristics that set them apart from other skin conditions.
Solar keratoses typically appear as:
Texture:
Color:
Size:
Location: The most common sites include:
Many patients notice solar keratoses by touch before they become visually obvious. You might feel a rough patch when washing your face or applying moisturizer, even when it's barely visible. This tactile detection is actually valuable—it means you're catching the lesion early.
Solar keratosis can be confused with several other conditions. Here's how to tell them apart:
ConditionKey DifferencesFeelSolar KeratosisRough, scaly, persistentSandpaper-like, crustyAge SpotsFlat, smooth, purely pigmentedCompletely smoothSeborrheic KeratosisWaxy, "stuck-on" appearanceRaised, softer textureSkin CancerMay bleed, grow rapidly, irregular bordersVariable, often firmDry SkinImproves with moisturizerTemporarily rough
For more detailed information about different skin lesions, visit our comprehensive guide on 25 types of skin lesions.
While most solar keratoses remain stable or grow slowly, certain changes warrant prompt evaluation:
⚠️ Seek professional assessment if you notice:
These symptoms might indicate progression toward squamous cell carcinoma, requiring more aggressive treatment.
Understanding the root causes helps you prevent new lesions and protect your skin going forward. Solar keratosis doesn't appear overnight—it's the culmination of years of sun exposure and cellular damage.
Ultraviolet radiation is the overwhelming cause of solar keratosis. Both UVA and UVB rays contribute to skin damage:
UVB rays (the "burning" rays):
UVA rays (the "aging" rays):
Every time UV radiation hits your skin, it creates the potential for cellular damage. Most of this damage gets repaired by your body's natural mechanisms, but some accumulates over time. After years or decades, this cumulative damage manifests as solar keratosis.
While anyone can develop these lesions, certain factors dramatically increase your risk:
Skin Type and Genetics:
Sun Exposure History:
Age:
Immune System Status:
Other Medical Conditions:
Think of sun damage like filling a bucket—each exposure adds a little more. Eventually, the bucket overflows, and that's when solar keratoses appear. This explains why:
The damage that leads to solar keratosis today might have started decades ago. That sunburn you got as a teenager? Those years of outdoor sports without sunscreen? They're all contributing factors.
The connection between solar keratosis and skin cancer is what makes this condition more than just a cosmetic concern. Let's break down exactly what the risks are—and what they mean for you.
Solar keratosis sits in a unique position on the spectrum between normal skin and cancer:
Normal Skin → Sun Damage → Solar Keratosis → Squamous Cell Carcinoma
Not every solar keratosis progresses to cancer. In fact, most don't. But understanding this pathway helps explain why dermatologists and surgeons take these lesions seriously.
Research on solar keratosis progression reveals important patterns:
Here's the critical point: while any single lesion has a relatively low chance of becoming cancerous, people with solar keratoses typically have multiple lesions and ongoing sun damage. This creates a cumulative risk that's more significant than the numbers for individual spots suggest.
When solar keratosis does progress, it typically becomes squamous cell carcinoma—the second most common form of skin cancer. Understanding this helps contextualize the importance of treatment:
SCC characteristics:
For comprehensive information about skin cancer types and risks, explore our detailed guide on 4 types of skin cancer.
When you have solar keratosis, it's rarely just about that one spot. The surrounding skin has likely experienced similar sun damage—a phenomenon called "field cancerization."
This means:
Think of it like weeds in a garden. Pulling one weed doesn't mean others won't sprout nearby, because the conditions that created the first weed still exist throughout the garden bed.
Given the progression risk, treating solar keratosis offers several advantages:
✅ Prevention: Stopping progression before it starts ✅ Simplicity: Early lesions require simpler, less invasive treatments ✅ Peace of mind: Eliminating the worry about cancer development ✅ Cosmetic benefit: Removing rough, unsightly patches ✅ Monitoring: Establishing a baseline for future skin checks
Our experienced surgical team at The Minor Surgery Center specializes in identifying and treating solar keratoses before they become more serious concerns. We provide personalized treatment plans that address your specific situation with minimally invasive solutions.
Accurate diagnosis is the foundation of effective treatment. Here's what happens when you seek professional evaluation for a suspicious skin lesion.
Most solar keratoses can be diagnosed through visual and tactile examination by a qualified healthcare provider. During your appointment, expect:
Visual Inspection: Your provider will carefully examine the lesion under good lighting, looking at:
Dermoscopy: Many providers use a dermoscope—a specialized magnifying device with polarized light that reveals structures beneath the skin's surface. This non-invasive tool helps distinguish solar keratosis from other conditions with greater accuracy.
Palpation: Your provider will gently feel the lesion, assessing:
While many solar keratoses can be diagnosed clinically, a biopsy may be recommended if:
Types of biopsy procedures:
Shave Biopsy:
Punch Biopsy:
Excisional Biopsy:
At The Minor Surgery Center, we perform these procedures with a comfort-first approach, ensuring you understand each step and feel at ease throughout the process.
Your provider will also consider other conditions that can mimic solar keratosis:
Accurate differentiation ensures you receive the right treatment for your specific condition. Learn more about actinic keratosis explained in our detailed resource.
When you present with solar keratosis, your provider should perform a complete skin examination. Why? Because:
This comprehensive approach is part of expert outpatient care—looking beyond the immediate concern to protect your overall skin health.
The good news about solar keratosis is that multiple effective treatments exist. Your provider will recommend the best approach based on the number of lesions, their location, your skin type, and your overall health.
For multiple lesions or field treatment, topical medications offer a non-invasive first-line option.
5-Fluorouracil (5-FU):
Imiquimod:
Diclofenac Gel:
Ingenol Mebutate:
Cryotherapy remains one of the most common treatments for individual solar keratoses.
How it works:
What to expect:
Advantages:
Considerations:
This surgical approach combines scraping and cauterization.
The procedure:
Best for:
Benefits:
PDT combines a photosensitizing medication with specific light wavelengths to destroy abnormal cells.
The process:
Advantages:
Considerations:
Medical-grade chemical peels can treat widespread solar keratoses, particularly on the face.
Common agents:
How they work:
Best suited for:
Various laser systems can effectively treat solar keratosis:
CO2 Laser:
Erbium Laser:
Benefits:
Your personalized treatment plan depends on several factors:
Lesion Characteristics:
Patient Factors:
Practical Considerations:
At The Minor Surgery Center, we develop a personalized treatment plan that considers all these factors. Our experienced surgical team explains each option clearly, helping you make informed decisions about your care. We specialize in safe and efficient surgery with minimally invasive solutions that get you back to your life quickly.
For information about our comprehensive skin lesion services, visit our pages on mole, cyst, and skin tag removal in Ajax and Barrie.
Understanding the treatment process helps you prepare mentally and practically for your procedure. Here's what typically happens from consultation through recovery.
Initial Consultation: During your first visit, your provider will:
Pre-Treatment Preparation: Depending on your chosen treatment, you may need to:
For Office Procedures (Cryotherapy, Curettage):
The actual treatment is typically quick:
For Topical Treatments:
You'll receive:
Pain and Discomfort:
Most treatments involve minimal discomfort:
Our comfort-first approach means we prioritize your experience, using appropriate anesthesia and taking time to ensure you're at ease throughout the procedure.
Immediate Post-Treatment (First 24-48 Hours):
Expect:
Care instructions typically include:
Days 3-14:
During this healing phase:
Important: Let crusts fall off naturally. Picking can cause scarring or infection.
Weeks 2-8:
Final healing occurs:
While generally safe, solar keratosis treatments can have side effects:
Common (Usually Temporary):
Less Common:
When to Contact Your Provider:
Seek medical attention if you experience:
Short-Term Follow-Up:
Most treatments require a follow-up visit:
Long-Term Monitoring:
Because solar keratosis indicates sun damage and cancer risk:
Think of solar keratosis treatment as the beginning of a long-term skin health partnership, not a one-time fix.
Treatment addresses existing solar keratoses, but prevention stops new ones from forming. Since you can't undo past sun damage, the focus shifts to preventing additional damage.
Comprehensive sun protection is non-negotiable if you've had solar keratosis:
Daily Sunscreen Use:
Choose a broad-spectrum sunscreen with these characteristics:
Application guidelines:
Protective Clothing:
Physical barriers offer excellent protection:
☀️ Recommended items:
Shade and Timing:
Strategic sun avoidance reduces exposure:
Avoiding Tanning Beds:
Tanning beds emit concentrated UV radiation and significantly increase skin cancer risk. If you've had solar keratosis, tanning beds are absolutely off-limits—no exceptions.
For comprehensive sun protection guidance, check out our complete UV index guide.
Between professional visits, monthly self-checks help you catch changes early.
How to perform a thorough self-exam:
While sun protection is paramount, certain nutritional strategies may support skin health:
Antioxidant-Rich Foods:
Omega-3 Fatty Acids:
Adequate Hydration:
Note: Nutrition supports but doesn't replace sun protection. No food or supplement can undo UV damage or eliminate skin cancer risk.
Sun avoidance raises questions about vitamin D, which your body produces during sun exposure. Here's the balanced approach:
The skin cancer risk from UV exposure far outweighs the benefits of sun-derived vitamin D, especially when dietary sources and supplements are readily available.
Prevention works best when integrated into daily life:
At Home:
At Work:
During Recreation:
If you've been diagnosed with solar keratosis, you're beginning a journey of ongoing skin health management. Here's how to approach this proactively.
Solar keratosis indicates you're at higher risk for:
This doesn't mean you'll definitely develop skin cancer—it means vigilance and prevention are especially important for you.
Effective long-term management often involves:
Primary Care Provider:
Dermatologist or Skin Specialist:
Surgical Specialists:
At The Minor Surgery Center, our experienced surgical team provides comprehensive evaluation and treatment for solar keratosis and related skin concerns. We work collaboratively with your other providers to ensure coordinated, expert outpatient care.
Your follow-up frequency depends on your risk level:
Lower Risk (1-2 lesions, successfully treated, good sun protection):
Higher Risk (multiple lesions, history of skin cancer, ongoing sun exposure):
Very High Risk (immunosuppressed, genetic conditions, multiple skin cancers):
Your provider will recommend the appropriate schedule for your situation.
Receiving a diagnosis of a "pre-cancerous" condition can be emotionally challenging. Common reactions include:
Healthy coping strategies:
✓ Educate yourself about the condition and treatments ✓ Focus on what you can control (prevention, treatment adherence) ✓ Reframe the diagnosis as an early warning that allows intervention ✓ Connect with others who have similar experiences ✓ Practice stress-reduction techniques (meditation, exercise, hobbies) ✓ Seek professional support if anxiety becomes overwhelming
Remember: solar keratosis is highly treatable, and your diagnosis gives you the opportunity to take proactive steps to protect your health.
Managing solar keratosis involves costs that vary based on treatment and insurance coverage:
Typical Expenses:
Insurance Coverage:
Cost-Saving Strategies:
Our team at The Minor Surgery Center provides transparent pricing and works with you to develop a personalized treatment plan that fits your budget and insurance situation.
Certain groups face unique challenges or considerations regarding solar keratosis.
People with compromised immune systems face dramatically higher risks:
High-Risk Groups:
Increased Risks:
Management Modifications:
Solar keratosis prevalence increases dramatically with age, creating specific considerations:
Challenges:
Adaptations:
While less common in darker-skinned individuals, solar keratosis does occur:
Unique Aspects:
Treatment Considerations:
Location significantly impacts solar keratosis risk and management:
High-Risk Locations:
For Toronto-Area Residents:
While Canada's northern latitude provides some UV protection compared to southern regions, solar keratosis remains common due to:
Year-round sun protection is essential, even in our climate. Winter sun reflecting off snow can be particularly intense.

Occasionally, yes—some solar keratoses spontaneously resolve without treatment. However, this is uncommon (less than 20% of lesions), and you can't predict which ones will disappear. More importantly, spontaneous regression doesn't eliminate your underlying sun damage or cancer risk. Professional evaluation and treatment remain the recommended approach.
Most solar keratoses aren't painful. They're typically asymptomatic or mildly uncomfortable. You might notice:
If a lesion becomes significantly painful, it may indicate inflammation, infection, or progression—warranting prompt evaluation.
There's no predictable timeline. Some lesions remain stable for years or decades, while others progress more quickly. Factors influencing progression include:
This unpredictability is precisely why early treatment makes sense—it eliminates the risk before progression occurs.
You can't reverse existing sun damage, but you can absolutely prevent new solar keratoses from forming and reduce the risk of progression in existing lesions. Comprehensive sun protection starting today makes a significant difference in your long-term skin health.
Scarring potential depends on the treatment method:
Your provider can discuss expected cosmetic outcomes for your specific situation and lesion location.
Costs vary widely based on:
Approximate ranges (without insurance):
Most insurance plans cover medically necessary treatment. Contact our office for specific pricing information.
Multiple lesions are common and indicate field cancerization—widespread sun damage to your skin. While this increases your overall skin cancer risk, it's manageable with:
Think of it as a wake-up call to take your skin health seriously, not a cause for panic.
At The Minor Surgery Center, we understand that discovering a pre-cancerous skin lesion can be concerning. That's why we've built our practice around clear communication, personalized care, and effective treatment that gets you back to your life quickly.
Expert Evaluation: Our experienced surgical team has extensive training in identifying and treating solar keratosis and related skin conditions. We use advanced diagnostic tools and techniques to ensure accurate assessment.
Comprehensive Treatment Options: We offer multiple treatment modalities under one roof, allowing us to recommend the best approach for your specific situation—not just the one we happen to offer.
Personalized Treatment Plans: No two patients are identical. We consider your:
Comfort-First Philosophy: We know medical procedures can be anxiety-inducing. Our team prioritizes your comfort through:
Efficient, Convenient Care: As an outpatient surgical center, we provide:
Ongoing Support: Your relationship with us doesn't end after treatment. We provide:
Initial Consultation:
Your first visit typically includes:
Treatment Visit:
If proceeding with in-office treatment:
Follow-Up Care:
We ensure continuity through:
We're committed to helping you achieve healthy, cancer-free skin through safe and efficient surgery and minimally invasive solutions. Our goal is simple: provide you with expert outpatient care that addresses your concerns and gets you back to your life with confidence.
Whether you have a single concerning spot or multiple lesions requiring treatment, our team is here to help. We combine medical expertise with genuine compassion, treating you as a person—not just a case.
To learn more about our comprehensive skin lesion services, visit our blog for educational resources and updates.
If you've discovered a rough, scaly patch on sun-exposed skin, or if you've been diagnosed with solar keratosis, taking action now protects your long-term health.
Don't wait and hope the lesion disappears. Schedule an appointment with a qualified healthcare provider who can:
Early evaluation means simpler treatment and better outcomes.
If treatment is recommended:
Treatment only works if you complete it properly.
Starting today:
Prevention is your most powerful tool for long-term skin health.
Solar keratosis requires ongoing attention:
Think of this as a lifelong commitment to your skin health.
Share what you've learned:
Your experience can help others catch problems early.
Solar keratosis represents a critical junction in your skin health journey—a warning sign that arrives while you still have time to act. These rough, scaly patches are your skin's way of telling you that cumulative sun damage has reached a threshold requiring attention.
The good news? You've caught it. You're informed. You can take action.
Understanding that solar keratosis is a pre-cancerous condition naturally raises concerns, but remember: "pre-cancerous" means you have the opportunity to intervene before cancer develops. With appropriate treatment and ongoing prevention, you can effectively manage these lesions and significantly reduce your skin cancer risk.
The key takeaways to remember:
✓ Solar keratosis is extremely common and highly treatable ✓ Multiple effective treatment options exist, from topical medications to minimally invasive procedures ✓ Early treatment is simpler and more effective than waiting ✓ Comprehensive sun protection prevents new lesions and protects overall skin health ✓ Regular monitoring catches changes early ✓ You're not alone—millions of people successfully manage this condition
At The Minor Surgery Center, we're here to support you through every step of this journey. Our experienced surgical team provides expert outpatient care with a comfort-first approach, offering personalized treatment plans that address your specific needs and concerns.
Whether you're dealing with your first solar keratosis or managing multiple lesions, we combine medical expertise with genuine compassion to help you achieve the best possible outcomes. We understand that these skin concerns can be worrying, and we're committed to providing clear communication, effective treatment, and ongoing support that gets you back to your life with confidence.
Don't let uncertainty or anxiety delay your care. Solar keratosis is most manageable when addressed promptly. Take that first step—schedule an evaluation, ask questions, understand your options, and make informed decisions about your skin health.
Your skin has been protecting you for years. Now it's time to return the favor.
Ready to address your solar keratosis concerns? Contact The Minor Surgery Center today to schedule a consultation with our experienced team. We're here to provide the expert, compassionate care you deserve.
[1] Criscione VD, Weinstock MA, Naylor MF, et al. Actinic keratoses: Natural history and risk of malignant transformation in the Veterans Affairs Topical Tretinoin Chemoprevention Trial. Cancer. 2009;115(11):2523-2530.
[2] American Academy of Dermatology. Actinic Keratosis: Overview. AAD.org. Updated 2024.
[3] Werner RN, Sammain A, Erdmann R, et al. The natural history of actinic keratosis: a systematic review. British Journal of Dermatology. 2013;169(3):502-518.
[4] Rossi R, Mori M, Lotti T. Actinic keratosis. International Journal of Dermatology. 2007;46(9):895-904.
[5] Thai KE, Fergin P, Freeman M, et al. A prospective study of the use of cryosurgery for the treatment of actinic keratoses. International Journal of Dermatology. 2004;43(9):687-692.
[6] Euvrard S, Kanitakis J, Claudy A. Skin cancers after organ transplantation. New England Journal of Medicine. 2003;348(17):1681-1691.