Molluscum contagiosum is a viral skin infection caused by the molluscum contagiosum virus (MCV), a member of the poxvirus family. Unlike many skin conditions, this one is highly recognizable once you know what to look for.
The virus spreads through direct skin-to-skin contact, contaminated objects (like towels or toys), or sexual contact in adults. It's particularly common in children aged 1-10 years, people with weakened immune systems, and sexually active adults [1].
What makes molluscum unique? The characteristic appearance of the bumps—small, firm, dome-shaped lesions with a pearly quality and a distinctive central indentation called umbilication. This tiny dimple or crater in the center is the hallmark feature that distinguishes molluscum from other skin lesions.
The infection is generally benign and self-limiting, meaning your immune system will eventually clear it without intervention. However, the timeline varies significantly—from a few months to several years.
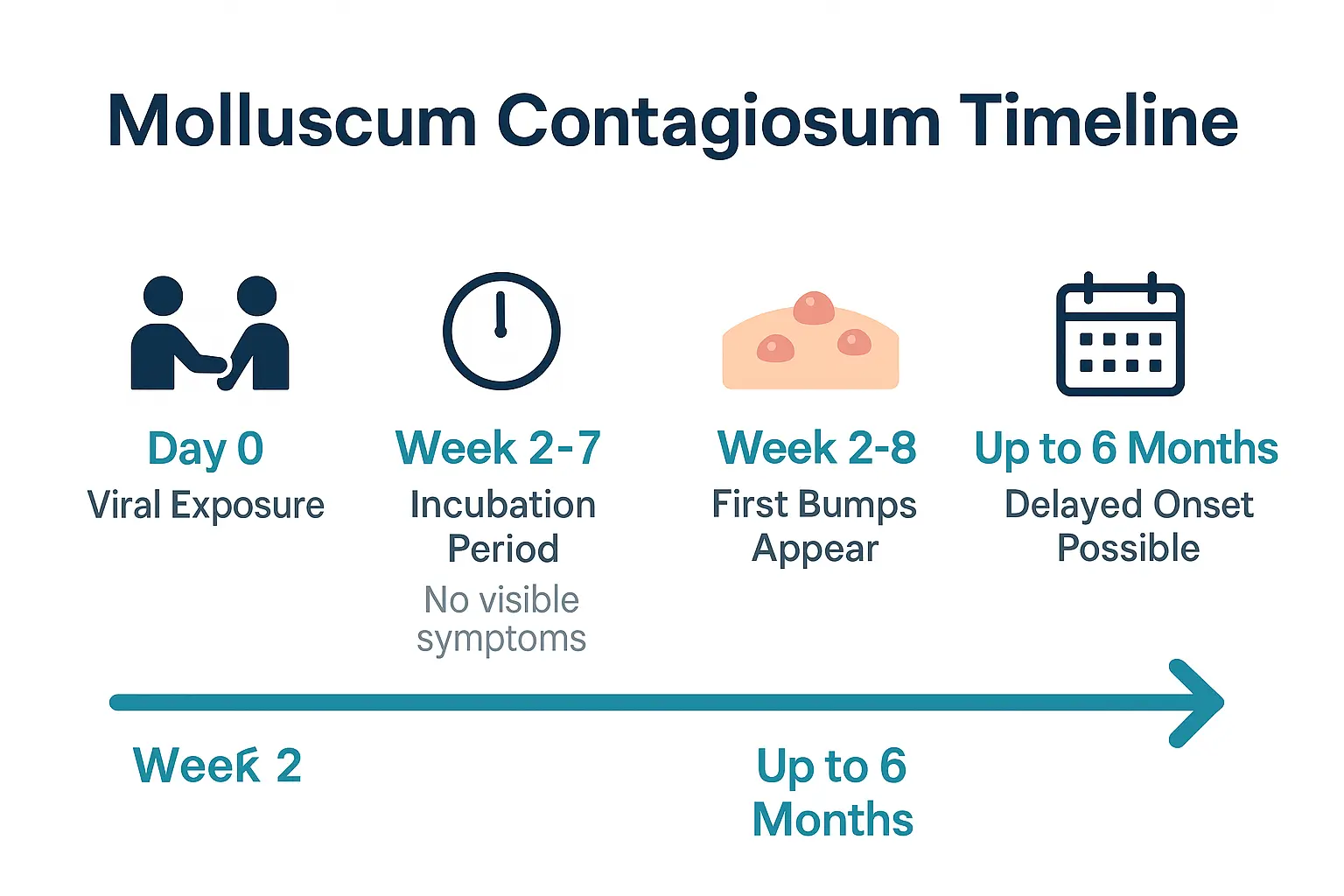
Before any visible signs appear, the molluscum virus has an incubation period—the time between when you're exposed to the virus and when symptoms first show up.
The typical incubation period ranges from 2 to 7 weeks, though it can extend up to 6 months in some cases [2]. This variability depends largely on individual immune system response. Someone with a robust immune system might see bumps appear sooner as their body responds to the infection, while others may not notice anything for months.
During this incubation phase, the virus is quietly replicating in skin cells. You won't see or feel anything unusual. This silent period is one reason molluscum spreads so easily—people don't realize they're infected and continue normal activities, including swimming, sharing towels, or close contact with others.
Understanding the incubation period helps you:
Children in group settings like daycare or school are particularly vulnerable during this time. The virus spreads easily through shared toys, wrestling, or any skin-to-skin contact during play.
The first stage is when you finally see something visible. These initial lesions are the earliest form of molluscum contagiosum bumps.
Small, firm bumps appear on the skin, typically 2-8 weeks after viral exposure. These early lesions have several distinctive characteristics:
At this early stage, the characteristic central dimple (umbilication) may not yet be visible. This can make initial identification challenging, as the bumps might resemble other common skin conditions like warts or small cysts.
In children, molluscum bumps most commonly appear on:
In adults, lesions frequently develop on:
These location patterns reflect the typical transmission routes—children through general play and contact, adults through sexual activity.
During stage one, the bumps are usually painless and don't cause significant discomfort. However, they may be:
This is the optimal time to seek evaluation if you're uncertain about what you're seeing. Early identification can help prevent spreading the infection to other body areas or to other people.
As molluscum contagiosum progresses, the bumps become more distinctive and easier to identify. Stage two is when the classic features fully develop.
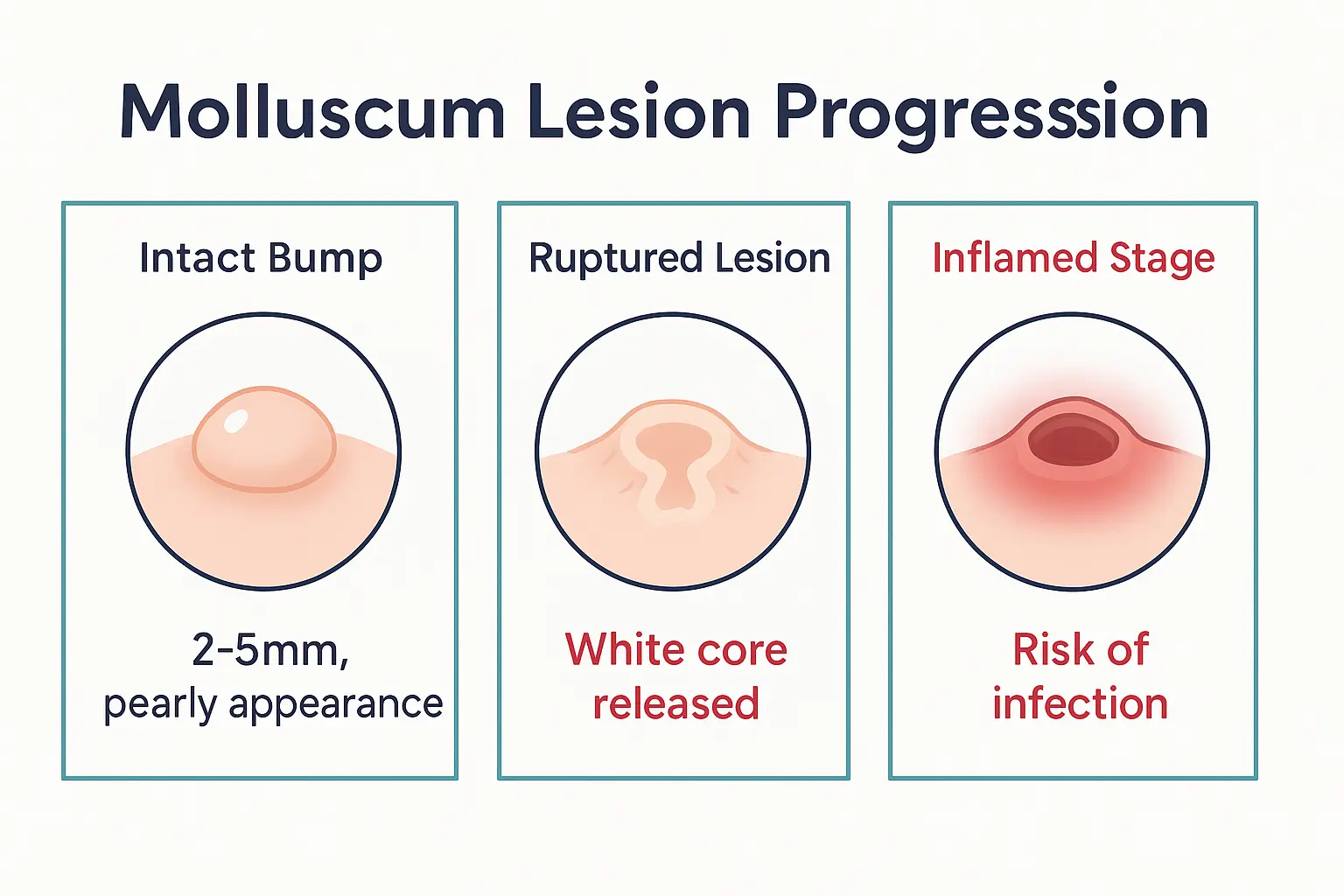
The bumps enlarge from their initial pinhead size to approximately 2-5mm in diameter, though some can grow as large as 30mm (about the size of a pencil eraser or larger) [3].
The central dimple appears—this is the hallmark sign. The umbilication looks like a tiny crater or belly button in the center of each bump. It's this feature that gives molluscum its distinctive appearance and helps differentiate it from other skin conditions.
A whitish core develops inside the bump. This waxy, cheese-like material is actually a collection of virus particles and dead skin cells. You might see this white substance through the thin skin covering the bump, especially as it matures.
The mature molluscum lesion has a very specific appearance:
Medical professionals classify molluscum infections based on the number of lesions [4]:
ClassificationNumber of LesionsTypical PresentationMildFewer than 10Isolated bumps, easily manageableModerate10-50 lesionsMultiple clusters, more noticeableSevereMore than 50 lesionsWidespread distribution, may indicate immune concerns
Severe cases are more common in individuals with compromised immune systems and may require professional evaluation and treatment.
During stage two, autoinoculation becomes a significant concern. This occurs when you scratch or touch an infected bump, then touch another area of your body. The virus transfers to the new location, creating additional lesions.
You might notice bumps appearing in a straight line pattern—this is a telltale sign of autoinoculation. The line represents the path your finger took across your skin after touching an infected area.
Prevention strategies include:
Not all molluscum bumps rupture, but when they do, it marks a distinct stage in the infection's progression. Understanding what happens during rupture helps you manage the situation appropriately.
The mature molluscum bump contains that whitish, waxy core material we mentioned earlier. As the bump continues to grow or if it's irritated by scratching, rubbing against clothing, or accidental trauma, the thin skin covering can break open.
When this happens:
The white core material is released. This substance is highly contagious and contains millions of virus particles. Any contact with this material can spread the infection.
A small crater forms where the bump used to be. This crater may be shallow or somewhat deeper, depending on the size of the original lesion.
The area becomes vulnerable to secondary bacterial infection, especially if not kept clean.
After rupture, the crater site often shows signs of inflammation:
Important distinction: Some redness and inflammation is normal as your immune system responds to the virus. However, increasing pain, spreading redness, warmth to the touch, or yellow/green pus suggests a bacterial infection that may require medical attention.
Medical professionals strongly advise against manually popping or squeezing molluscum lesions [5]. Here's why:
Spreading risk increases dramatically. The viral material inside can spread to your fingers, then to other body parts or surfaces you touch.
Secondary infection becomes more likely. Breaking the skin barrier with non-sterile methods introduces bacteria into the wound.
Scarring potential increases. Aggressive manipulation of the bumps can damage deeper skin layers, leading to permanent scarring.
Pain and discomfort worsen. Squeezing inflamed tissue hurts and can cause unnecessary trauma.
If bumps burst naturally, the best approach is to:
While some inflammation is expected, certain signs warrant professional evaluation:
At The Minor Surgery Center, our experienced surgical team can evaluate inflamed lesions and provide a personalised treatment plan that addresses both the viral infection and any secondary complications.
The final stage of molluscum contagiosum is resolution—when your immune system successfully fights off the virus and the bumps begin to disappear.
Resolution can take anywhere from a few months to several years [6]. The wide variability depends on several factors:
Immune system strength plays the biggest role. Children and adults with healthy immune systems typically clear the infection within 6-18 months. Those with compromised immunity may struggle with persistent lesions for years.
Number of lesions affects timeline. A few isolated bumps often resolve faster than widespread infections with dozens of lesions.
Location matters. Lesions in areas subject to frequent friction or irritation may take longer to heal.
Age influences resolution. Children's immune systems often mount a robust response, leading to faster clearance compared to some adults.
As your body fights off the virus, you'll notice gradual changes:
Bumps begin to shrink. The dome-shaped profile flattens, and the overall size decreases.
Color changes occur. The pearly, flesh-colored appearance may shift to pink or red as inflammation increases (a sign your immune system is actively working).
The central dimple becomes less pronounced as the bump deflates.
Eventually, bumps fade completely, leaving behind normal-looking skin in most cases.
Most people heal without any lasting marks. However, some may experience:
Temporary hyperpigmentation (darker spots) or hypopigmentation (lighter spots) where bumps used to be. This is more common in people with darker skin tones and usually fades over time.
Mild scarring may occur if lesions were scratched, picked at, or became infected. These scars are typically small and may improve with time.
Textural changes are rare but can happen with larger lesions or those that became significantly inflamed.
Once your immune system clears the virus from your body, those specific lesions won't return. However, you can be reinfected if exposed to the virus again. There's no lasting immunity to molluscum contagiosum.
Reinfection is more common in:
While waiting for natural resolution, you can support the process:
For many patients, the waiting period feels frustrating. If you're looking to get back to your life without the extended wait, professional treatment options can significantly accelerate the process.
One critical aspect often overlooked in medical resources is how molluscum contagiosum appears across different skin tones. Visual guides frequently show lesions on lighter skin, leaving people with darker complexions uncertain about what to look for.
In lighter skin (Fitzpatrick types I-III):
In darker skin (Fitzpatrick types IV-VI):
Misidentification is more common in people with darker skin tones because:
If you're uncertain whether bumps on your skin match molluscum contagiosum descriptions, professional evaluation is essential. Our team at The Minor Surgery Center has experience identifying and treating skin lesions across all skin types with a comfort-first approach.
Regardless of skin tone, certain characteristics stay the same:
When examining bumps on your skin, several conditions might look similar at first glance. Understanding the visual differences helps with accurate identification.
Warts are also caused by a virus (HPV), but they look quite different:
FeatureMolluscum ContagiosumWartsSurface textureSmooth, pearlyRough, cauliflower-likeCentral featureDimple (umbilication)Black dots (thrombosed capillaries)ShapeDome-shaped, roundedIrregular, raisedColorFlesh-colored, white, pinkGrayish, brown, flesh-coloredPainUsually painlessCan be painful (especially plantar warts)
Skin tags are benign growths that might initially be confused with molluscum:
Skin tags are typically:
Molluscum bumps are:
Milia are tiny white bumps containing keratin:
Acne lesions can sometimes resemble molluscum, especially in early stages:
Acne characteristics:
Molluscum characteristics:
If you're uncertain about what you're seeing, professional evaluation provides clarity. This is especially important when:
The experienced surgical team at The Minor Surgery Center can provide accurate diagnosis and discuss treatment options tailored to your situation.
Understanding how molluscum spreads helps you recognize risk patterns and take preventive measures.
While anyone can contract molluscum, certain groups are at higher risk:
Children aged 1-10 years represent the largest affected group [8]. The infection spreads easily in:
Sexually active adults can contract molluscum through intimate contact. In adults, the infection is often considered a sexually transmitted infection (STI) when lesions appear in the genital area.
People with weakened immune systems are particularly vulnerable, including those with:
Athletes participating in contact sports face increased risk through:
Direct skin-to-skin contact is the primary transmission route. The virus passes from one person's lesions to another person's skin during:
Indirect contact through contaminated objects (fomites) also spreads the virus:
Autoinoculation spreads the virus across your own body when you:
Water-related transmission occurs in:
The virus survives on surfaces for extended periods, making environmental contamination a concern in:
Regular cleaning of shared surfaces, toys, and equipment helps reduce transmission risk.
While molluscum contagiosum often resolves on its own, treatment can speed up the process, prevent spreading, and address cosmetic concerns.
Watchful waiting (no active treatment) is appropriate when:
Active treatment makes sense when:
Several effective treatments are available through expert outpatient care:
Cryotherapy (freezing) uses liquid nitrogen to destroy infected tissue:
Curettage (scraping) physically removes the lesion:
Laser therapy targets and destroys infected tissue:
Topical medications can be prescribed for home application:
Chemical treatments applied by healthcare providers:
At The Minor Surgery Center, we specialize in safe and efficient surgery for skin lesions, including molluscum contagiosum. Our approach focuses on:
Personalized treatment plans tailored to your specific situation—number of lesions, location, age, and preferences all factor into the recommended approach.
Comfort-first procedures using appropriate anesthesia and gentle techniques to minimize discomfort during treatment.
Expert execution by our experienced surgical team who understand the nuances of treating molluscum across different skin types and body locations.
Efficient service that respects your time—we know you want to get back to your life without prolonged treatment courses.
Clear communication about what to expect during and after treatment, including realistic timelines for healing and resolution.
Children require special consideration:
Adults often prioritize:
You'll find numerous home remedies suggested online—from tea tree oil to duct tape. While some people report success, medical evidence for most home remedies is limited or lacking [9].
Risks of home treatment include:
If you prefer a conservative approach, watchful waiting under medical supervision is safer than experimenting with unproven remedies.
Prevention focuses on breaking the transmission chain and protecting uninfected skin.
Hand washing is your first line of defense:
Don't scratch or pick at bumps:
Cover lesions when appropriate:
Avoid sharing personal items:
Clean and disinfect:
Pool and water safety:
Childcare and school:
Sexual health:
Sports and activities:
When one family member has molluscum:
These measures aren't about isolation or shame—they're practical steps to protect others while supporting the infected person through resolution.
People with weakened immune systems face unique challenges with molluscum contagiosum.
Your immune system is ultimately responsible for clearing the molluscum virus. When immune function is compromised, several problems can arise:
More lesions develop—often hundreds instead of the typical few dozen.
Bumps grow larger—sometimes reaching 15-30mm (giant molluscum).
Resolution takes much longer—years instead of months.
Atypical presentations occur—lesions may look different or appear in unusual locations.
Higher recurrence rates—even after treatment, new lesions continue appearing.
HIV/AIDS patients, particularly those with low CD4 counts, often experience severe molluscum infections. The number and size of lesions can serve as a clinical marker of immune status.
Cancer patients undergoing chemotherapy have temporarily suppressed immune systems, making them vulnerable to molluscum and other opportunistic infections.
Organ transplant recipients taking immunosuppressive medications to prevent rejection face increased molluscum risk.
Autoimmune disease patients on immune-modulating therapies (biologics, corticosteroids) may develop more extensive infections.
Genetic immunodeficiencies create lifelong susceptibility to molluscum and other viral skin infections.
Managing molluscum in immunocompromised individuals requires a different approach:
More aggressive treatment is often necessary:
Immune system support when possible:
Regular monitoring for:
Specialist involvement may include:
At The Minor Surgery Center, we coordinate care with your other healthcare providers to ensure a comprehensive, personalized treatment plan that addresses both the molluscum infection and your overall health needs.
While molluscum contagiosum is medically benign, its psychological and social effects can be significant.
Children with visible molluscum may experience:
Self-consciousness about their appearance, especially if bumps are on the face, arms, or other visible areas.
Teasing or bullying from peers who don't understand the condition.
Activity restrictions that feel unfair—being excluded from swimming or sports while friends participate.
Anxiety about medical treatments, particularly if procedures are uncomfortable.
Frustration with the long resolution timeline—months feel like forever to a child.
Parents often struggle with:
Guilt about not preventing the infection or uncertainty about how their child contracted it.
Worry about spreading to siblings or other family members.
Decision fatigue about whether to treat or wait for natural resolution.
Social pressure from other parents, schools, or activity programs.
Information overload from conflicting advice found online.
Adults face different concerns:
Dating and intimacy become complicated when lesions are in genital areas.
Professional appearance matters in careers where image is important.
Gym and fitness activities may need modification or temporary pause.
Disclosure decisions—who needs to know, and how to explain the condition.
Education is empowering:
Open communication helps:
Support systems matter:
Focus on what you can control:
Remember—molluscum is temporary. The bumps will eventually resolve, and you'll get back to your life without this concern.
While molluscum often doesn't require medical intervention, certain situations warrant professional evaluation.
Signs of infection:
Rapid spreading:
Lesions in sensitive areas:
Uncertain diagnosis:
Quality of life impact:
A thorough evaluation typically includes:
Visual examination of the lesions—most cases are diagnosed by appearance alone.
Medical history covering:
Dermoscopy (magnified examination) if diagnosis is uncertain.
Biopsy in rare cases where diagnosis can't be confirmed visually—this is uncommon but may be necessary for atypical presentations.
Discussion of treatment options tailored to your specific situation, preferences, and goals.
For molluscum evaluation and treatment, you might see:
Primary care physicians who can diagnose and treat straightforward cases.
Dermatologists specializing in skin conditions, ideal for complex or extensive infections.
Pediatricians experienced in managing molluscum in children.
Minor surgery centers like The Minor Surgery Center that offer specialized procedures for lesion removal with expert outpatient care.
Look for providers who:
If you're in the waiting period—whether for natural resolution or between treatment sessions—daily management strategies help maintain comfort and prevent complications.
Gentle cleansing:
Moisturizing:
Avoid irritation:
Over-the-counter options:
Behavioral strategies:
Swimming:
Exercise and sports:
Clothing choices:
Maintain perspective:
Stay connected:
Plan for resolution:
The medical understanding of molluscum contagiosum continues to evolve, with researchers exploring new treatment approaches and prevention strategies.
Topical immunomodulators are being studied for their effectiveness in stimulating local immune responses to clear the virus more quickly.
Photodynamic therapy uses light-activated compounds to target and destroy infected cells with minimal damage to surrounding tissue.
Combination approaches that use multiple treatment modalities simultaneously show promise for faster resolution with fewer recurrences.
Improved delivery systems for existing medications aim to increase effectiveness while reducing side effects.
Unlike many viral infections, there's currently no vaccine for molluscum contagiosum. However, research is exploring:
Understanding immune responses that lead to natural clearance, which could inform vaccine development.
Cross-protection studies examining whether immunity to related poxviruses offers any protection.
Targeted immune therapies that could provide temporary immunity for high-risk populations.
Dermoscopy advances help differentiate molluscum from similar-looking conditions more accurately.
Artificial intelligence applications are being developed to assist in visual diagnosis through smartphone apps.
Molecular testing methods could provide rapid confirmation in uncertain cases.
Education initiatives aim to reduce stigma and improve understanding of transmission and prevention.
Screening programs in high-risk settings (childcare, schools) could identify and treat cases earlier.
Policy development around activity restrictions balances infection control with avoiding unnecessary exclusion.
While these advances are promising, the current standard of care remains effective for most people. Whether you choose watchful waiting or active treatment, molluscum contagiosum is manageable with expert outpatient care and a personalized treatment plan.
How long does each stage of molluscum contagiosum last?
The incubation period lasts 2-7 weeks (up to 6 months). Initial bumps appear and mature over 2-4 weeks. The mature stage can persist for months. Total infection duration ranges from 6-18 months on average, though some cases resolve faster and others persist for several years.
Can you have molluscum contagiosum without the central dimple?
Yes, especially in very early stages. The characteristic umbilication (central dimple) develops as bumps mature. Very small or newly-formed lesions may not yet show this feature. However, as lesions grow to 2-5mm, the dimple typically becomes visible.
Is molluscum contagiosum more contagious in certain stages?
Yes. The infection is most contagious when bumps burst and release the white core material containing viral particles. However, direct contact with intact bumps can also spread the virus. All stages carry some transmission risk.
How can you tell if molluscum is getting better or worse?
Getting better: Bumps shrink, flatten, become less pearly, decrease in number, and eventually fade. Getting worse: New bumps appear, existing lesions grow larger, spreading to new body areas, or signs of infection develop (increased redness, pain, pus).
Can molluscum contagiosum spread to internal organs?
No. Molluscum contagiosum is a skin infection only. It doesn't affect internal organs, even in immunocompromised individuals. However, people with severely weakened immune systems may develop extensive skin lesions.
Should you pop molluscum bumps to speed up healing?
No. Medical professionals strongly advise against popping or squeezing molluscum lesions. This increases spreading risk, raises infection potential, and can cause scarring. If treatment is desired, seek professional removal methods.
Can adults get molluscum contagiosum from their children?
Yes. Adults can contract molluscum through contact with infected children, though it's less common than child-to-child transmission. Parents should practice good hygiene when caring for infected children, including handwashing and avoiding direct contact with lesions.
Does molluscum contagiosum leave permanent scars?
Most cases heal without scarring. However, scarring can occur if lesions are picked at, become infected, or are very large. People with darker skin tones may experience temporary hyperpigmentation that eventually fades. Professional treatment minimizes scarring risk.
Understanding molluscum contagiosum stages pictures empowers you to recognize this common skin infection, know what to expect, and make informed decisions about management and treatment.
From the initial incubation period through the appearance of those characteristic dome-shaped bumps with central dimples, to eventual resolution—each stage follows a predictable pattern. While the timeline varies, the outcome is ultimately the same: your immune system will clear the infection, and you'll get back to your life bump-free.
The key takeaways to remember:
✅ Early identification helps prevent spreading to other body areas and to other people through simple hygiene measures and activity modifications.
✅ Most cases resolve naturally within 6-18 months, though treatment can significantly accelerate this timeline when desired.
✅ Visual characteristics remain consistent across stages—dome shape, pearly appearance, central dimple—even though color may vary with skin tone.
✅ Professional treatment options are safe, effective, and available when watchful waiting doesn't align with your needs or lifestyle.
✅ Prevention focuses on breaking transmission chains through hygiene, covering lesions, and avoiding shared personal items.
If you're dealing with molluscum contagiosum—whether for yourself or a family member—you don't have to navigate this alone.
For mild cases with few lesions, watchful waiting with good hygiene practices may be appropriate. Monitor for signs of spreading or infection, and maintain open communication with your healthcare provider.
For more extensive infections, lesions in sensitive areas, or when you simply want faster resolution, professional treatment offers minimally invasive solutions with expert care.
At The Minor Surgery Center, our experienced surgical team specializes in treating skin lesions including molluscum contagiosum. We provide:
Whether you're in Toronto or surrounding areas, we're here to help you move past this temporary skin condition with confidence and minimal disruption to your daily activities.
Don't let molluscum contagiosum hold you back. With the right information, appropriate prevention measures, and access to professional treatment when needed, you can manage this infection effectively and look forward to clear, healthy skin.
For more information about skin lesion treatment or to schedule a consultation, visit our blog for additional resources or contact our team directly. We're committed to helping you achieve life-moving, pain-free outcomes with compassionate, expert care.
[1] Centers for Disease Control and Prevention. (2023). Molluscum Contagiosum. Retrieved from https://www.cdc.gov/poxvirus/molluscum-contagiosum/
[2] American Academy of Dermatology Association. (2024). Molluscum contagiosum: Diagnosis and treatment. Journal of the American Academy of Dermatology.
[3] Olsen, J. R., Gallacher, J., Piguet, V., & Francis, N. A. (2014). Epidemiology of molluscum contagiosum in children: a systematic review. Family Practice, 31(2), 130-136.
[4] van der Wouden, J. C., van der Sande, R., Kruithof, E. J., Sollie, A., van Suijlekom-Smit, L. W., & Koning, S. (2017). Interventions for cutaneous molluscum contagiosum. Cochrane Database of Systematic Reviews, 5(5).
[5] Leung, A. K., Barankin, B., & Hon, K. L. (2017). Molluscum contagiosum: an update. Recent Patents on Inflammation & Allergy Drug Discovery, 11(1), 22-31.
[6] Meza-Romero, R., Navarrete-Dechent, C., & Downey, C. (2019). Molluscum contagiosum: an update and review of new perspectives in etiology, diagnosis, and treatment. Clinical, Cosmetic and Investigational Dermatology, 12, 373-381.
[7] Gao, Y., Zhao, Y., & Zhang, H. (2020). Dermoscopy of molluscum contagiosum in different skin phototypes. Journal of the European Academy of Dermatology and Venereology, 34(8), 1789-1792.
[8] Chen, X., Anstey, A. V., & Bugert, J. J. (2013). Molluscum contagiosum virus infection. The Lancet Infectious Diseases, 13(10), 877-888.
[9] Hanna, D., Hatami, A., Powell, J., Marcoux, D., Maari, C., Savard, P., & McCuaig, C. (2006). A prospective randomized trial comparing the efficacy and adverse effects of four recognized treatments of molluscum contagiosum in children. Pediatric Dermatology, 23(6), 574-579.