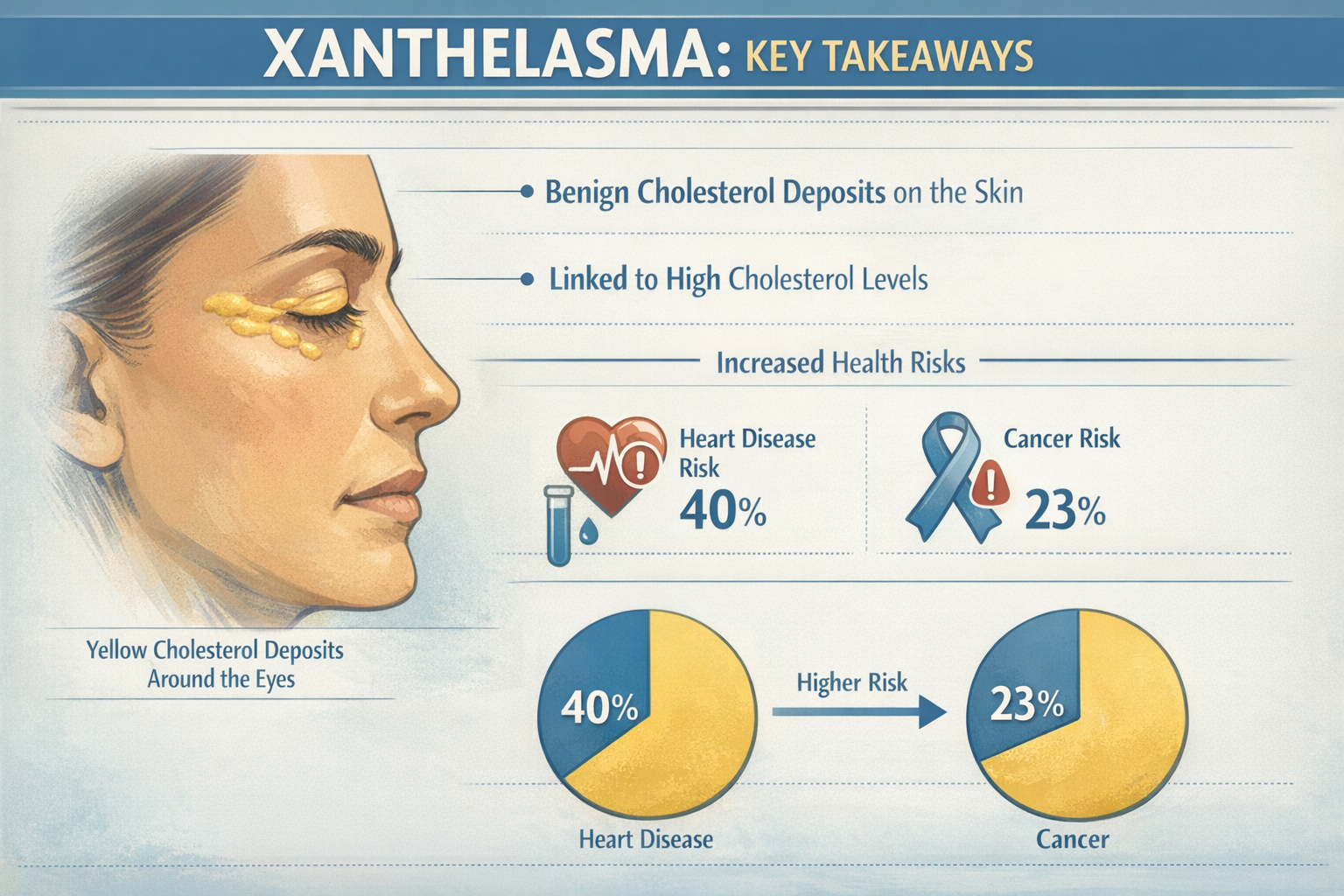
When small, yellowish bumps appear on the eyelids, many people dismiss them as harmless cosmetic concerns. However, these deposits—known as xanthelasma—may signal something far more serious happening inside the body. The connection between cancer xanthelasma, cardiovascular disease, and cholesterol disorders has captured the attention of medical researchers worldwide, revealing that these seemingly innocent skin lesions could be warning signs of life-threatening conditions.
Xanthelasma palpebrarum represents one of the most visible manifestations of lipid metabolism disorders. While these cholesterol-filled plaques themselves are benign, their presence raises important questions about overall health status. Understanding the relationship between xanthelasma, heart disease risk, elevated cholesterol levels, and potential cancer associations empowers individuals to take proactive steps toward better health outcomes.
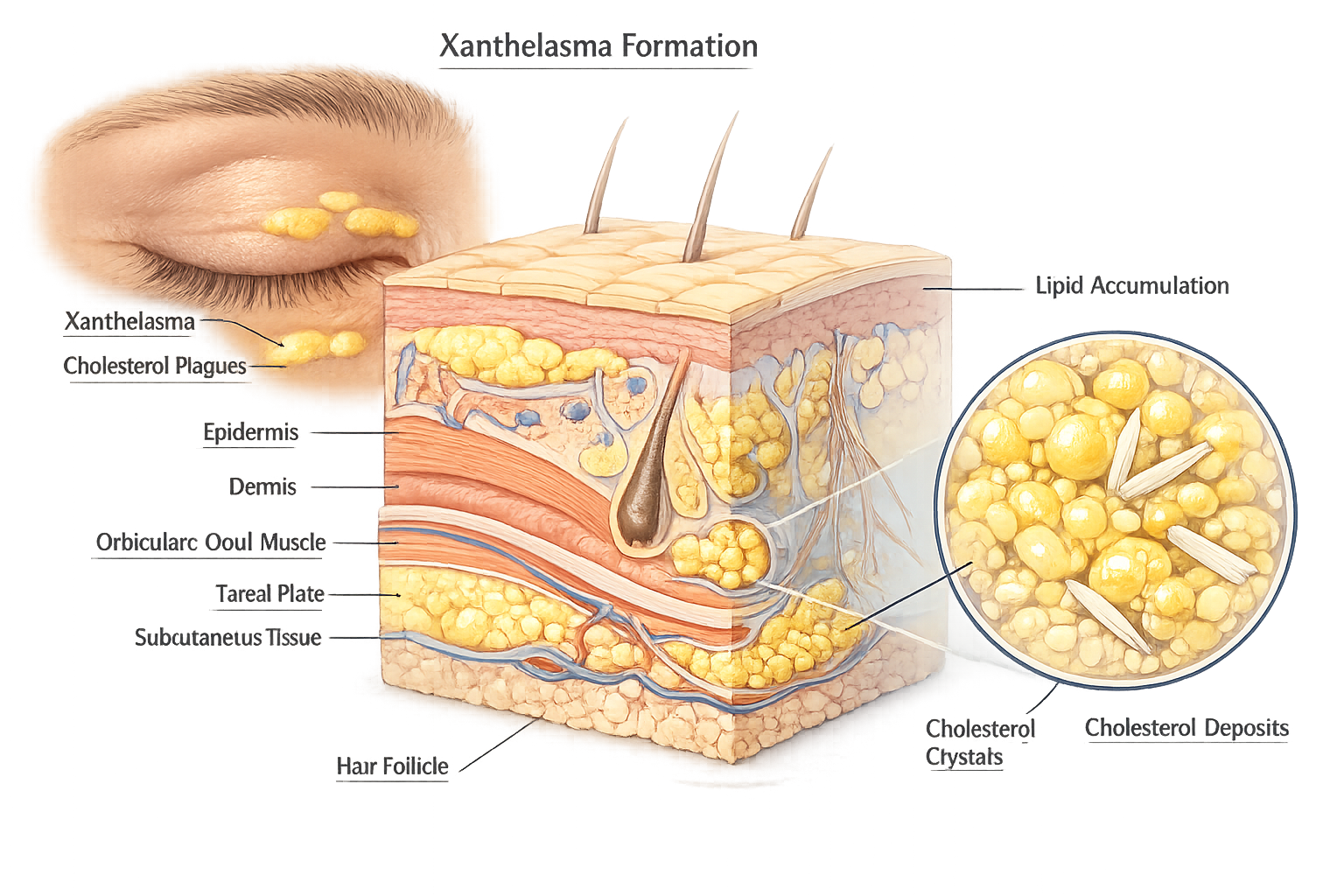
Xanthelasma palpebrarum consists of yellowish plaques that develop on or around the eyelids, typically appearing near the inner corner of the eye (medial canthus). These soft, flat or slightly raised deposits range in size from a few millimeters to several centimeters. The term "xanthelasma" derives from Greek words meaning "yellow" (xanthos) and "plate" (elasma), perfectly describing their characteristic appearance [2].
These lesions develop when cholesterol accumulates in macrophages (immune cells) beneath the skin's surface, creating visible deposits. The affected skin maintains normal texture and doesn't cause pain, itching, or other symptoms. Xanthelasma can appear on one or both eyelids, and multiple deposits may develop over time.
Xanthelasma affects approximately 0.3% to 1.1% of the general population, with higher prevalence in certain demographic groups [3]. Key risk factors include:
Important distinction: While xanthelasma represents the most common form of cutaneous xanthoma, other types exist throughout the body. Understanding various types of skin lesions helps differentiate xanthelasma from other conditions.
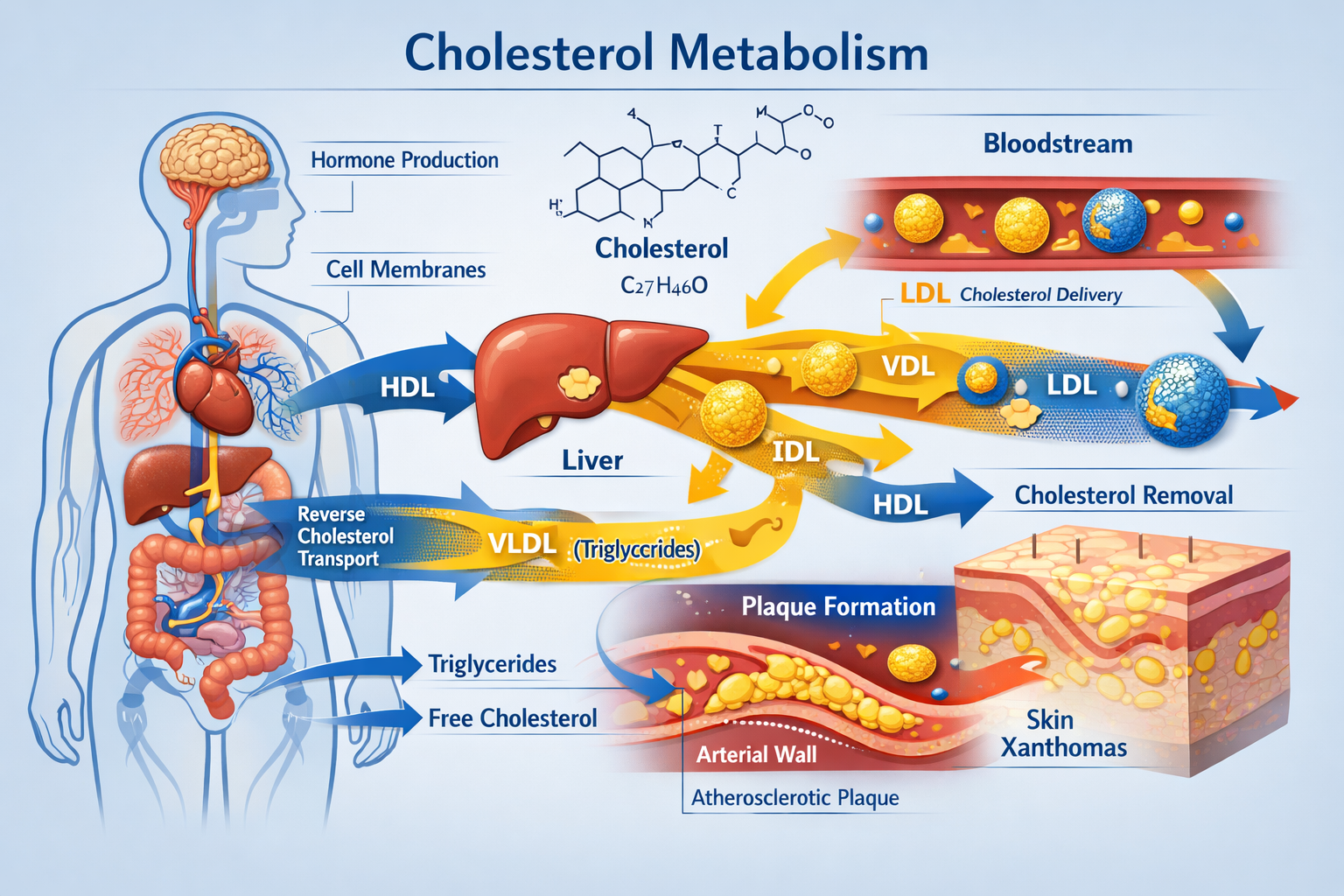
The development of xanthelasma involves complex interactions between lipid metabolism, immune response, and skin biology:
This process mirrors early atherosclerotic plaque formation in blood vessels, explaining why xanthelasma serves as a potential marker for cardiovascular disease risk.
The relationship between xanthelasma and cholesterol abnormalities represents one of the most significant clinical associations. Research indicates that approximately 50% of individuals with xanthelasma have dyslipidemia—abnormal blood lipid levels [4]. However, the remaining 50% demonstrate normal cholesterol levels, complicating the diagnostic picture.
Common lipid abnormalities associated with xanthelasma include:
Lipid ParameterAssociation with XanthelasmaClinical SignificanceTotal CholesterolElevated in 40-50% of casesGeneral cardiovascular risk markerLDL CholesterolOften significantly elevatedPrimary atherogenic lipoproteinHDL CholesterolFrequently decreasedProtective factor when adequateTriglyceridesMay be elevatedAssociated with metabolic syndromeApolipoprotein BOften increasedSuperior cardiovascular risk predictorLipoprotein(a)Sometimes elevatedIndependent risk factor for heart disease
Primary hyperlipidemia refers to genetic disorders affecting lipid metabolism. Several hereditary conditions strongly associate with xanthelasma:
Secondary hyperlipidemia results from other medical conditions or lifestyle factors:
Perhaps the most intriguing aspect of xanthelasma involves cases occurring with completely normal cholesterol levels—termed normolipidemic xanthelasma. This phenomenon affects approximately half of all xanthelasma patients and raises important questions about underlying mechanisms [5].
Several theories explain normolipidemic xanthelasma:
Critical insight: Even with normal cholesterol levels, xanthelasma still indicates increased cardiovascular risk, suggesting these deposits reflect subtle metabolic disturbances not captured by conventional lipid testing.
The straightforward answer is no—xanthelasma itself does not cause cancer and is not a cancerous condition. These cholesterol deposits are benign lesions composed of lipid-laden macrophages without malignant transformation potential. Xanthelasma does not spread, invade surrounding tissues, or metastasize like cancer.
However, the relationship between cancer xanthelasma becomes more nuanced when examining indirect associations through shared risk factors and metabolic pathways.
Emerging research suggests complex relationships between cholesterol metabolism, lipid disorders, and certain cancer types. Several mechanisms potentially link these conditions:
Cholesterol and cancer cell metabolism: Cancer cells require substantial cholesterol for rapid membrane synthesis during cell division. Some malignancies upregulate cholesterol synthesis pathways or increase cholesterol uptake from circulation [6].
Inflammatory pathways: Both xanthelasma formation and cancer development involve chronic inflammation. Inflammatory mediators released during lipid accumulation may create environments conducive to cellular transformation.
Metabolic syndrome connections: The cluster of conditions associated with xanthelasma—obesity, diabetes, dyslipidemia—independently increase risk for several cancer types, including:
Several epidemiological studies have examined cancer incidence in populations with xanthelasma or related lipid disorders:
A Danish cohort study following over 12,000 individuals with xanthelasma found modest increases in certain cancer types compared to the general population, though results varied by cancer site and didn't establish causation [7].
Research on familial hypercholesterolemia patients—who frequently develop xanthelasma—shows conflicting results regarding cancer risk. Some studies suggest slightly reduced cancer rates, possibly due to cholesterol-lowering statin therapy, while others find no significant difference [8].
Important context: Any observed associations likely reflect shared underlying metabolic disturbances rather than xanthelasma directly causing cancer. The lipid abnormalities, inflammatory states, and metabolic syndrome features that promote xanthelasma formation may also influence cancer development through separate pathways.
While discussing cancer xanthelasma connections, it's crucial to distinguish these benign cholesterol deposits from actual skin cancers that may occasionally appear on eyelids:
Basal cell carcinoma (BCC): The most common eyelid malignancy, typically appearing as a pearly nodule with visible blood vessels. Learn more about different types of skin cancer and their characteristics.
Squamous cell carcinoma (SCC): Less common, may present as scaly patches or non-healing sores on the eyelid.
Sebaceous gland carcinoma: Rare but aggressive eyelid cancer, sometimes mimicking benign conditions like chalazion.
Melanoma: Extremely rare on eyelids but possible, appearing as pigmented lesions with irregular borders.
Key differentiating features:
✅ Xanthelasma: Soft, yellow, flat or slightly raised, bilateral, painless, stable or slowly growing
⚠️ Skin cancer: Variable colors (flesh, red, brown, black), firm texture, may ulcerate or bleed, typically unilateral, progressively growing
When in doubt, seek evaluation at a specialized skin cancer clinic for definitive diagnosis through examination and possible biopsy.
For individuals with xanthelasma, particularly those with associated metabolic conditions, comprehensive cancer screening becomes important:
The association between xanthelasma and cardiovascular disease represents one of the most clinically significant aspects of these cholesterol deposits. Multiple large-scale studies have documented alarming risk elevations:
Copenhagen General Population Study (12,745 participants followed for decades) revealed that individuals with xanthelasma experienced [9]:
Framingham Heart Study data demonstrated that xanthelasma independently predicted cardiovascular events even after adjusting for traditional risk factors including cholesterol levels [10].
Critical finding: These cardiovascular risks persist even in individuals with normal cholesterol levels, suggesting xanthelasma indicates metabolic disturbances beyond what standard lipid panels detect.
Xanthelasma and atherosclerosis (arterial plaque buildup) share remarkable pathophysiological similarities:
Common cellular mechanisms:
Parallel progression: Both conditions develop through similar stages involving endothelial dysfunction, lipid infiltration, immune cell recruitment, and progressive accumulation of cholesterol-rich deposits.
"Xanthelasma can be viewed as a visible window into the invisible process of atherosclerosis occurring throughout the vascular system. The same metabolic disturbances creating yellow deposits on eyelids are simultaneously building dangerous plaques in coronary arteries." - Cardiovascular Research Findings
When xanthelasma is discovered, comprehensive cardiovascular evaluation becomes essential:
Recommended diagnostic workup:
Risk stratification tools: Healthcare providers use calculators incorporating xanthelasma presence alongside traditional risk factors (age, sex, smoking, blood pressure, cholesterol) to estimate 10-year cardiovascular event probability.
The cardiovascular risks associated with xanthelasma necessitate aggressive risk factor management:
Lipid-lowering therapy:
Lifestyle modifications:
Additional cardiovascular medications (as indicated):
Important consideration: Treating underlying lipid disorders and cardiovascular risk factors represents the medical priority, while cosmetic xanthelasma removal addresses aesthetic concerns separately.
Xanthelasma diagnosis typically occurs through visual examination by healthcare providers. The characteristic yellow appearance and eyelid location make clinical diagnosis straightforward in most cases.
Diagnostic confirmation may involve:
Biopsy is rarely necessary for typical xanthelasma but may be performed if:
Histopathological examination reveals foam cells (lipid-laden macrophages) in the dermis, confirming the diagnosis.
Once xanthelasma is identified, extensive laboratory evaluation investigates underlying causes and associated conditions:
Standard lipid panel:
Advanced lipid testing:
Metabolic screening:
Additional testing based on clinical suspicion:
Depending on findings, several specialists may become involved in xanthelasma management:
Cardiologist: For cardiovascular risk assessment, advanced imaging, and aggressive lipid management in high-risk patients.
Endocrinologist: When diabetes, thyroid disorders, or complex metabolic conditions require specialized management.
Lipidologist: Specialist focusing specifically on lipid disorders, particularly for severe or treatment-resistant dyslipidemia.
Dermatologist: For xanthelasma removal procedures and evaluation of other skin manifestations. Consider visiting specialized clinics for expert assessment.
Genetic counselor: When hereditary lipid disorders are suspected, particularly familial hypercholesterolemia affecting family members.
Ophthalmologist: If xanthelasma interferes with vision or eyelid function, or if removal near the eye requires specialized surgical expertise.
Xanthelasma requires ongoing surveillance even after initial evaluation:
Lipid monitoring:
Cardiovascular surveillance:
Xanthelasma progression tracking:
Metabolic condition monitoring:
Addressing the root cause represents the first priority in xanthelasma management. While treating dyslipidemia may not always eliminate existing deposits, it prevents new lesion formation and reduces cardiovascular risk.
Statin therapy (HMG-CoA reductase inhibitors):
Combination therapy for inadequate statin response:
Case reports suggest that aggressive lipid-lowering therapy occasionally leads to partial xanthelasma regression, though complete resolution through medical management alone remains uncommon [11].
Multiple techniques exist for xanthelasma removal, each with specific advantages and limitations:
Surgical excision:
Laser therapy:
Cryotherapy (freezing):
Chemical cauterization:
Electrodesiccation:
Radiofrequency ablation:
For expert removal procedures, consider consulting specialized removal clinics with experience in delicate eyelid lesions.
Xanthelasma recurrence represents a significant challenge following removal:
Strategies to minimize recurrence:
Eyelid skin's delicate nature makes cosmetic outcomes particularly important:
Minimizing scarring:
Camouflage options during healing or if removal is declined:
Realistic expectations:
Heart-healthy eating patterns form the foundation of lipid disorder management and xanthelasma prevention:
Mediterranean Diet:
DASH Diet (Dietary Approaches to Stop Hypertension):
Portfolio Diet:
Specific dietary recommendations:
✅ Foods to emphasize:
❌ Foods to limit:
Regular physical activity provides multiple benefits for lipid management and cardiovascular health:
Aerobic exercise effects:
Recommended activity levels:
Exercise intensity guide:
Special considerations:
Excess body weight, particularly abdominal obesity, significantly impacts lipid profiles and cardiovascular risk:
Weight loss benefits (5-10% body weight reduction):
Effective weight management strategies:
Metabolic syndrome (cluster of conditions including abdominal obesity, high triglycerides, low HDL, elevated blood pressure, insulin resistance) strongly associates with xanthelasma and cardiovascular disease. Comprehensive lifestyle modification targeting all components provides maximum benefit.
Often overlooked, psychological stress and sleep quality significantly influence metabolic health:
Chronic stress effects:
Stress management techniques:
Sleep optimization:
Research shows inadequate sleep (<6 hours) and poor sleep quality associate with:
While xanthelasma itself rarely constitutes a medical emergency, certain associated symptoms demand immediate attention:
🚨 Seek emergency care for:
These symptoms may indicate acute cardiovascular events requiring emergency treatment, regardless of xanthelasma presence.
📋 Schedule medical evaluation within days to weeks for:
Xanthelasma-specific concerns:
Associated symptoms suggesting metabolic or cardiovascular issues:
Concerning changes in known xanthelasma:
Proactive health monitoring becomes particularly important for individuals with xanthelasma:
Annual examinations should include:
Additional periodic testing based on individual risk factors:
Family screening considerations: When xanthelasma appears in younger individuals (<40 years) or with very high cholesterol levels, familial hypercholesterolemia should be considered. First-degree relatives (parents, siblings, children) require screening since this genetic condition affects 50% of offspring.
Coordinated care optimizes outcomes for individuals with xanthelasma and associated conditions:
Primary care physician: Coordinates overall care, manages multiple conditions, provides preventive services, and makes specialist referrals.
Cardiologist: Addresses cardiovascular risk, performs advanced testing, manages complex lipid disorders and heart disease.
Endocrinologist: Manages diabetes, thyroid disorders, and complex metabolic conditions affecting lipid metabolism.
Dermatologist or cosmetic surgeon: Provides expert xanthelasma removal when desired, evaluates other skin lesions. Consider specialized skin lesion removal services for comprehensive care.
Registered dietitian: Develops personalized nutrition plans for lipid management, weight control, and overall metabolic health.
Exercise physiologist or physical therapist: Creates safe, effective exercise programs tailored to individual capabilities and cardiovascular risk.
Mental health professional: Addresses stress, anxiety, depression, and behavioral change challenges affecting health outcomes.
The visible nature of xanthelasma creates unique psychological challenges beyond the medical implications:
Common emotional responses:
Coping strategies:
Social considerations: While xanthelasma is medically benign, its visibility on the face creates social awareness. Some individuals report questions or comments from others, while many people don't notice or recognize the deposits. Personal comfort levels vary widely.
Case example 1 - Lifestyle transformation: A 52-year-old woman developed xanthelasma with cholesterol of 280 mg/dL. Through comprehensive lifestyle changes (Mediterranean diet, daily walking, 25-pound weight loss), she reduced cholesterol to 190 mg/dL. While existing xanthelasma persisted, no new lesions appeared over 5 years. She underwent successful laser removal with no recurrence while maintaining lifestyle changes.
Case example 2 - Familial hypercholesterolemia diagnosis: A 38-year-old man with xanthelasma and LDL cholesterol of 220 mg/dL was diagnosed with familial hypercholesterolemia. Genetic testing confirmed the diagnosis, prompting family screening that identified two affected children. Aggressive statin therapy reduced his LDL to 70 mg/dL. His xanthelasma was surgically removed, and he avoided the early heart attack his father experienced at age 45.
Case example 3 - Normolipidemic xanthelasma: A 45-year-old woman developed bilateral xanthelasma despite completely normal cholesterol levels. Comprehensive evaluation revealed no underlying conditions. Advanced lipid testing showed elevated lipoprotein(a), an independent cardiovascular risk factor. She underwent chemical cauterization for xanthelasma removal and started aspirin therapy for cardiovascular protection. Regular monitoring continues with no recurrence after 3 years.
Reliable information sources:
Support communities:
Educational opportunities:
Advocacy and awareness:
For comprehensive information on various skin conditions and treatment options, visit The Minor Surgery Center blog for expert insights.
Xanthelasma represents far more than a cosmetic concern—these yellowish eyelid deposits serve as visible markers of potentially serious underlying metabolic and cardiovascular conditions. While the relationship between cancer xanthelasma remains an area of ongoing research without definitive direct causation established, the well-documented connections to heart disease and cholesterol disorders demand serious attention and proactive management.
The most important takeaways for anyone discovering xanthelasma include:
🔍 Comprehensive medical evaluation is essential: Don't dismiss these deposits as merely cosmetic. Complete lipid panels, cardiovascular risk assessment, and screening for underlying conditions like diabetes and thyroid disorders provide crucial health information.
❤️ Cardiovascular risk reduction takes priority: With up to 48% increased heart attack risk, addressing cholesterol levels, blood pressure, diabetes, and other cardiovascular risk factors through medication and lifestyle changes can be life-saving.
💊 Medical management addresses root causes: While xanthelasma removal treats the visible symptom, managing underlying lipid disorders through statins and other medications prevents new lesion formation and reduces serious cardiovascular events.
🥗 Lifestyle modifications provide powerful benefits: Heart-healthy eating patterns, regular physical activity, weight management, stress reduction, and adequate sleep improve lipid profiles, reduce cardiovascular risk, and enhance overall health beyond what medications alone achieve.
🔬 Ongoing monitoring ensures optimal outcomes: Regular lipid testing, cardiovascular assessments, and health screenings detect changes early and guide treatment adjustments for maximum benefit.
If you have xanthelasma or suspect you might be developing these deposits, take these concrete steps:
Immediate actions (within 1-2 weeks):
Short-term goals (1-3 months):
Long-term commitments (ongoing):
Xanthelasma serves as a reminder that visible changes on the body's surface often reflect deeper processes occurring internally. Rather than viewing these deposits solely as cosmetic nuisances, recognizing them as potential health warnings empowers individuals to take control of their cardiovascular and metabolic health.
The good news: effective treatments exist for both xanthelasma removal and the underlying conditions that cause them. With proper medical care, lifestyle modifications, and ongoing monitoring, individuals with xanthelasma can minimize their cardiovascular risk, prevent disease progression, and maintain excellent quality of life.
Your health is your most valuable asset. Don't ignore the warning signs your body provides. Take action today to understand what xanthelasma means for your health, address any underlying conditions, and build a comprehensive plan for long-term wellness. The investment you make in your health today pays dividends for years to come.
For expert evaluation and treatment of xanthelasma and other skin lesions, consider consulting with specialized professionals who understand both the cosmetic and medical implications of these important conditions.
[1] Christoffersen M, Frikke-Schmidt R, Schnohr P, Jensen GB, Nordestgaard BG, Tybjærg-Hansen A. Xanthelasmata, arcus corneae, and ischaemic vascular disease and death in general population: prospective cohort study. BMJ. 2011;343:d5497.
[2] Bergman R. The pathogenesis and clinical significance of xanthelasma palpebrarum. Journal of the American Academy of Dermatology. 1994;30(2):236-242.
[3] Nair PA, Singhal R. Xanthelasma Palpebrarum. StatPearls Publishing. 2023.
[4] Watanabe A, Yoshimura A, Wakasugi T, et al. Serum lipids, lipoprotein lipids and coronary heart disease in patients with xanthelasma palpebrarum. Atherosclerosis. 1981;38(3-4):283-290.
[5] Rohrich RJ, Janis JE, Pownell PH. Xanthelasma palpebrarum: a review and current management principles. Plastic and Reconstructive Surgery. 2002;110(5):1310-1314.
[6] Kuzu OF, Noory MA, Robertson GP. The role of cholesterol in cancer. Cancer Research. 2016;76(8):2063-2070.
[7] Christoffersen M, Tybjærg-Hansen A. Visible aging signs as risk markers for ischemic heart disease: epidemiology, pathogenesis and clinical implications. Ageing Research Reviews. 2016;25:24-41.
[8] Mundal LJ, Igland J, Veierød MB, et al. Impact of age on excess risk of coronary heart disease in patients with familial hypercholesterolaemia. Heart. 2018;104(19):1600-1607.
[9] Christoffersen M, Frikke-Schmidt R, Schnohr P, et al. Visible age-related signs and risk of ischemic heart disease in the general population. Circulation. 2014;129(9):990-998.
[10] Kannel WB, Dawber TR, Thomas HE Jr, McNamara PM. Comparison of serum lipids in the prediction of coronary heart disease: Framingham Study indicates that cholesterol level and blood pressure are major factors in coronary disease. Annals of Internal Medicine. 1964;61:888-899.
[11] Segal P, Insull W Jr, Chambless LE, et al. The association of dyslipoproteinemia with corneal arcus and xanthelasma. Circulation. 1986;73(1):108-118.
[12] Raulin C, Schoenermark MP, Werner S, Greve B. Xanthelasma palpebrarum: treatment with the ultrapulsed CO2 laser. Lasers in Surgery and Medicine. 1999;24(2):122-127.
[13] Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. New England Journal of Medicine. 2018;378(25):e34.