Waking up with yellowish patches around your eyelids can be alarming, and when those cholesterol deposits—known as xanthelasma—require surgical removal, understanding what comes next becomes crucial. The xanthelasma surgery recovery time is a common concern for patients preparing for this delicate eyelid procedure, and knowing what to expect can significantly reduce anxiety while promoting optimal healing outcomes.
Whether you're considering surgical excision, laser treatment, or another removal method, the recovery process follows predictable patterns that can help you plan your schedule, manage discomfort, and achieve the best cosmetic results. This comprehensive guide explores every aspect of healing after xanthelasma removal, from the first 24 hours through complete recovery.
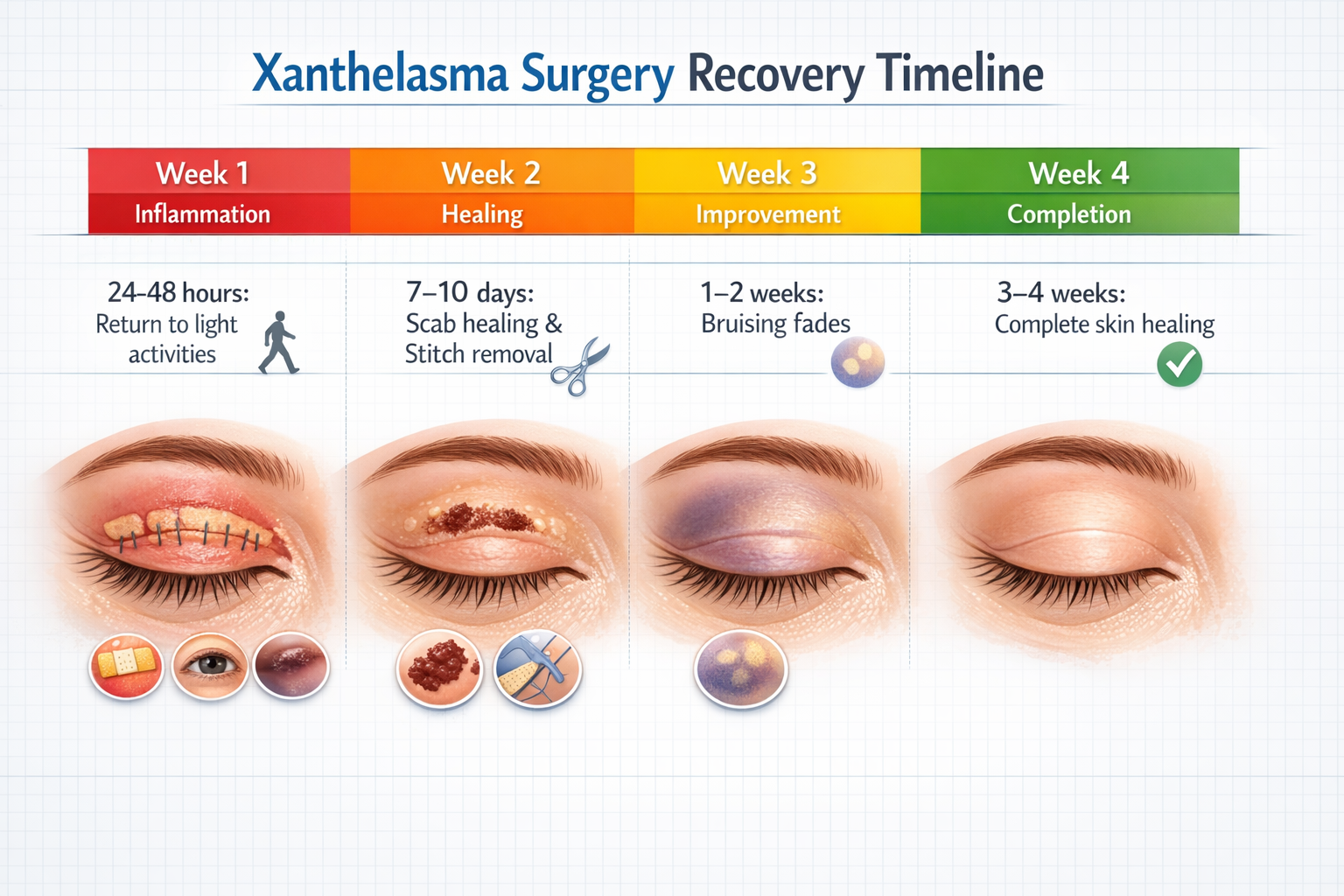
✅ Quick return to activities: Most patients resume light activities within 24-48 hours after xanthelasma surgery, with minimal downtime required[4]
✅ Visible healing timeline: Scabs and crusting typically heal within 7-10 days, while bruising improves significantly within 1-2 weeks[1][2][6]
✅ Complete recovery: Full skin healing generally occurs within 3-4 weeks, though individual healing rates may vary[5]
✅ Manageable discomfort: Mild pain is common but usually controlled with simple over-the-counter pain medication like paracetamol[2][3][7]
✅ Simple aftercare routine: Following basic wound care instructions—including antibiotic ointment application three times daily—promotes optimal healing and minimizes complications[7]
Xanthelasma palpebrarum represents one of the most common forms of cutaneous xanthoma, appearing as soft, yellowish plaques typically located on the medial aspects of the upper and lower eyelids. These cholesterol-rich deposits develop when lipid-laden macrophages accumulate in the dermis, creating visible cosmetic concerns that many patients find distressing.
While xanthelasma can occur in individuals with normal lipid profiles, approximately 50% of patients have associated dyslipidemia or elevated cholesterol levels. Other contributing factors include:
The deposits themselves are benign and painless, but they rarely resolve spontaneously and tend to grow larger over time, making surgical intervention the most effective treatment option for permanent removal.
Before discussing recovery, it's worth noting that several treatment modalities exist for xanthelasma removal:
Each method has different recovery characteristics, though surgical excision remains the gold standard for larger lesions and offers the lowest recurrence rates. Similar to other facial cyst removal techniques, the approach selected impacts healing time and cosmetic outcomes.
Understanding the xanthelasma surgery recovery time requires breaking down the healing process into distinct phases, each with characteristic symptoms and milestones. This timeline helps patients set realistic expectations and recognize normal healing versus potential complications.
The first day after xanthelasma removal is critical for establishing proper healing patterns. Patients typically experience:
Expected Symptoms:
Activity Restrictions: Patients should not drive themselves home after the procedure and should arrange for transportation via taxi or a friend[7]. The combination of local anesthesia effects, potential vision blur from ointment application, and the delicate nature of the surgery makes driving unsafe during this initial period[2].
Immediate Care Requirements:
This week represents the most visible healing period, when patients notice daily improvements but must remain vigilant about wound care.
What to Expect:
Day RangeTypical SymptomsCare RequirementsDays 2-3Peak swelling, crusting beginsContinue ointment 3x daily[7]Days 4-5Scab formation, reduced swellingGentle cleansing, no pickingDays 6-7Scabs start looseningPrepare for suture removal
Scab and Crust Development: Scabs or crusting are completely normal and typically heal within 7-10 days[1][2]. These protective coverings should never be picked or forcibly removed, as premature disruption can lead to scarring or infection.
Suture Removal: For patients who received traditional stitches, removal typically occurs 7-10 days after surgery[7]. Many modern procedures use dissolving sutures that eliminate the need for this appointment[4]. The removal process is quick and causes minimal discomfort.
By the second week, most patients experience significant improvement in appearance and comfort levels.
Bruising Resolution: Bruising often improves significantly within 1-2 weeks[2][6], transitioning from purple-blue tones to yellowish-green before fading completely. The thin, delicate skin around the eyes makes bruising more visible but also allows for faster reabsorption.
Resuming Normal Activities:
Similar to cyst removal recovery time, individual healing rates vary based on factors like age, overall health, and adherence to aftercare instructions.
Full skin healing is typically complete within 3-4 weeks[5], though subtle changes in pigmentation or texture may continue improving for several months.
What "Complete Healing" Means:
Long-Term Scar Appearance: When performed by experienced surgeons, xanthelasma removal typically results in minimal scarring that follows the natural eyelid creases. The scars continue to fade and soften for up to a year after surgery.
Not all patients heal at the same rate. Several variables significantly impact how quickly you recover from xanthelasma removal surgery.
The specific removal method directly affects healing time:
Surgical Excision:
Laser Ablation:
Chemical or Cryotherapy:
Larger deposits require more extensive tissue removal, which naturally extends healing time. Lesions located near the inner corner of the eye (medial canthus) may take slightly longer to heal due to:
🧬 Age: Younger patients generally heal faster due to more robust cellular regeneration and collagen production.
💊 Overall Health Status: Conditions like diabetes, autoimmune disorders, or vascular disease can significantly slow healing.
🚬 Smoking: Tobacco use constricts blood vessels and impairs oxygen delivery to healing tissues, potentially doubling recovery time.
💊 Medications: Blood thinners, immunosuppressants, and certain supplements can affect healing rates.
🍎 Nutrition: Adequate protein, vitamin C, zinc, and other nutrients support tissue repair. Learn more about foods and micronutrients that speed healing after minor skin surgery.
Perhaps the most controllable factor, adherence to aftercare instructions dramatically influences outcomes. Patients who consistently:
...typically experience faster, complication-free healing compared to those who neglect these guidelines.
For patients who prefer detailed daily guidance, this section breaks down the typical experience during xanthelasma surgery recovery time.
Morning/Procedure Time:
Afternoon/Evening:
Vision Considerations: Temporary vision blur may occur if ointment is applied near the eye[2]. This is normal and resolves as the ointment is absorbed or naturally cleared by blinking.
What You'll Notice:
Your Care Routine:
Activity Level: Most patients can return to light activities within 24-48 hours[4], including:
Physical Changes:
Psychological Adjustment: This phase can be challenging cosmetically, as the area may look worse before it looks better. Patients should remember this is completely normal and temporary.
Continuing Care:
Healing Milestones:
Expanding Activities: By the end of this period, many patients feel comfortable resuming most normal activities, though strenuous exercise should still wait.
Appearance:
Makeup and Cosmetics: Once the skin surface is completely closed (typically 1-2 weeks post-procedure)[2][4], patients can resume makeup application. Use gentle, non-irritating products and avoid pulling or tugging at the delicate eyelid skin.
By one month post-surgery, full skin healing is typically complete[5]. The area may still appear slightly pink or have subtle texture differences, but these continue to improve over the following months.
Long-Term Scar Maturation: Scars continue to fade and soften for 6-12 months after surgery. Proper sun protection during this period is essential to prevent hyperpigmentation of healing tissue.
One of the most common concerns patients express is: "How much will it hurt?" The good news is that xanthelasma surgery recovery time is typically associated with only mild discomfort[2][3][7].
Expected Discomfort:
Effective Pain Management:
💊 Over-the-Counter Options: Simple pain tablets like paracetamol (acetaminophen) are usually sufficient to control discomfort[2][3][7]. These should be taken as directed on the package or as prescribed by your surgeon.
❄️ Cold Therapy: Applying cold compresses for 10-15 minutes several times daily during the first 48-72 hours helps reduce both pain and swelling. Use a clean cloth barrier between the ice pack and skin.
🛏️ Elevation: Keeping your head elevated, especially while sleeping, minimizes swelling and associated discomfort.
Certain pain medications should be avoided unless specifically approved by your surgeon:
Always consult your surgical team before taking any medication during recovery, similar to guidelines for basal cell carcinoma recovery.
While mild discomfort is normal, certain pain patterns warrant immediate medical attention:
🚨 Contact your surgeon if you experience:
These symptoms may indicate infection or other complications requiring prompt treatment.
Following proper aftercare protocols is the single most important factor you can control to ensure smooth healing during your xanthelasma surgery recovery time.
Antibiotic Ointment Application: Apply antibiotic ointment three times daily for one week[7] to prevent infection and keep the area moist for optimal healing. Common options include:
Application Technique:
Cleansing Protocol:
Understanding what you can and cannot do during recovery prevents complications and promotes healing.
First Week:
Weeks 2-4:
The healing skin is extremely vulnerable to sun damage, which can cause permanent hyperpigmentation or interfere with proper healing.
Essential Protection Measures:
Continue diligent sun protection for at least 6-12 months after surgery to allow scars to mature without discoloration.
Head Elevation: Sleep with your head elevated on 2-3 pillows for the first week to minimize swelling. This position promotes proper drainage and reduces morning puffiness.
Side Sleeping: If you typically sleep on your side, try to avoid putting pressure on the surgical side for at least the first week. Back sleeping is ideal during early recovery.
When to Resume: Makeup can typically be applied 1-2 weeks post-procedure once the skin surface is completely closed[2][4]. Starting too early risks introducing bacteria into healing wounds.
Product Selection:
Application Tips:
Attending scheduled follow-up visits allows your surgeon to:
Don't skip these appointments, even if you feel everything is healing well.
While xanthelasma surgery is generally safe with a high success rate, understanding potential complications helps you recognize problems early and seek appropriate care.
Prolonged Swelling: Some patients experience swelling that persists beyond the typical 1-2 week timeframe. This is more common in individuals who:
Management: Continue cold compresses, maintain elevation, and give your body more time. Consult your surgeon if swelling worsens or persists beyond 3-4 weeks.
Hyperpigmentation: Darkening of the skin at the surgical site can occur, particularly in individuals with darker skin tones or those who don't protect the area from sun exposure.
Prevention:
Mild Asymmetry: Slight differences in healing between both eyes are normal, especially if xanthelasma was removed from both upper eyelids. Most asymmetry resolves as healing completes.
Infection: Though rare when proper aftercare is followed, infection can occur. Signs include:
Action: Contact your surgeon immediately. Infections typically respond well to oral antibiotics when caught early.
Excessive Bleeding: Minor oozing is normal in the first 24-48 hours, but active bleeding requires attention.
When to Seek Help:
Ectropion (Eyelid Malposition): In rare cases, excessive tissue removal can cause the lower eyelid to turn outward. This is more common when large xanthelasma deposits are removed from the lower lid.
Symptoms:
This complication requires surgical correction and should be evaluated promptly.
Xanthelasma can recur even after successful surgical removal, particularly if underlying lipid abnormalities aren't addressed. Recurrence rates vary by treatment method:
Reducing Recurrence Risk:
Understanding how xanthelasma surgery recovery time compares to similar procedures provides helpful context and realistic expectations.
ProcedureReturn to Light ActivitiesVisible HealingComplete HealingScarring RiskXanthelasma Removal24-48 hours[4]7-10 days[1][2]3-4 weeks[5]Low (follows natural creases)Lipoma Removal1-2 days7-14 days2-4 weeksLow to moderateCyst Removal1-3 days7-14 days2-6 weeksVaries by locationMole RemovalImmediate to 1 day5-10 days2-3 weeksLow with proper techniqueSkin Tag RemovalImmediate3-7 days1-2 weeksMinimal
The periorbital region (around the eyes) has unique characteristics that influence healing:
Advantages:
Challenges:
Despite these challenges, xanthelasma removal typically offers a favorable recovery profile compared to procedures in areas with thicker skin or poorer blood supply.
Patients who have undergone other minor skin surgeries may notice familiar patterns during xanthelasma recovery. The healing process shares similarities with lipoma removal surgery recovery, including:
Beyond basic aftercare instructions, these expert recommendations can help you achieve the best possible outcome during your xanthelasma surgery recovery time.
Two Weeks Before:
One Week Before:
Day Before:
Certain nutrients are particularly important for tissue repair and immune function:
Protein Sources:
Vitamin C:
Zinc:
Vitamin A:
For comprehensive guidance, review our article on foods and micronutrients that speed healing.
Water Intake: Aim for at least 8-10 glasses of water daily to support cellular function and toxin removal. Proper hydration keeps tissues supple and promotes efficient healing.
Anti-Inflammatory Foods:
Foods to Limit:
Psychological stress can impair wound healing by affecting immune function and increasing inflammation. Consider:
Once initial healing is complete (typically after 2-3 weeks), you can begin scar care:
Silicone Products: Silicone gel sheets or ointments have strong evidence for reducing scar visibility. Apply consistently for 3-6 months for best results.
Massage: Gentle massage of mature scars (after 4-6 weeks) can improve texture and flexibility. Use circular motions with light pressure for 5 minutes daily.
Continued Sun Protection: UV exposure can permanently darken healing scars. Continue diligent sun protection for at least one year post-surgery.

Knowing when to seek professional guidance versus managing symptoms at home is crucial for safe recovery.
✅ Expected and Manageable:
🚨 Requires Professional Evaluation:
Infection Signs:
Bleeding Issues:
Vision Changes:
Wound Healing Problems:
Allergic Reactions:
Call 911 or Go to Emergency:
Contact Surgeon Same Day:
Schedule Follow-Up Appointment:
Understanding what to expect months and years after xanthelasma removal helps set realistic goals and maintain satisfaction with results.
1-3 Months:
3-6 Months:
6-12 Months:
Even after successful removal, patients should monitor for recurrence, particularly if underlying lipid disorders persist.
Self-Monitoring:
Medical Follow-Up:
Research indicates high satisfaction rates among xanthelasma removal patients, particularly when:
Certain patient populations require modified approaches or additional precautions during xanthelasma surgery recovery time.
Diabetes can significantly impact wound healing through multiple mechanisms:
Challenges:
Recommendations:
Anticoagulant medications increase bleeding risk but are often medically necessary.
Common Blood Thinners:
Management Approach:
Never stop blood thinners without explicit approval from the physician who prescribed them, as this can increase stroke or heart attack risk.
Age-related changes affect healing but don't preclude successful outcomes:
Considerations:
Adaptations:
Individuals prone to keloid or hypertrophic scarring require special attention:
Risk Factors:
Preventive Strategies:
The surgeon's skill and experience directly impact both cosmetic results and xanthelasma surgery recovery time.
Board Certification: Seek surgeons certified by recognized boards in:
Specific Experience: Ask potential surgeons:
Facility Accreditation: Ensure procedures are performed in accredited facilities with:
📋 Preparation Questions:
🔍 Technique Questions:
⏰ Recovery Questions:
💰 Financial Questions:
🔄 Follow-Up Questions:
⚠️ Warning Signs:
Understanding the financial aspects of xanthelasma removal helps with planning and decision-making.
Xanthelasma removal costs vary based on:
Procedure Factors:
Average Costs (2026):
Multiple lesions or bilateral (both eyes) treatment typically cost more than single lesion removal.
Cosmetic vs. Medical Necessity:
Most insurance companies consider xanthelasma removal cosmetic and therefore not covered. However, coverage may be possible if:
Documentation Requirements: If seeking insurance coverage, you'll typically need:
Pre-Authorization: Always obtain pre-authorization before assuming insurance will cover the procedure. Denial rates are high for xanthelasma removal.
Payment Plans: Many practices offer:
Health Savings Accounts (HSA) / Flexible Spending Accounts (FSA): Even if insurance doesn't cover the procedure, you may be able to use pre-tax HSA or FSA funds if the procedure is deemed medically necessary by your physician.
For cost estimation specific to your situation, consider using a minor surgery cost estimator tool.
Most patients can resume makeup application 1-2 weeks post-procedure once the skin surface is completely closed[2][4]. Wait until all scabs have fallen off naturally and no open wounds remain. Use gentle, hypoallergenic products and clean applicators to minimize infection risk.
Light walking is typically fine within 24-48 hours, but strenuous exercise should be avoided for at least 1-2 weeks. Activities that increase blood pressure (heavy lifting, running, intense cardio) can promote bleeding and swelling. Gradually resume exercise as healing progresses, starting with low-impact activities.
Recurrence is possible, with rates ranging from 10-50% depending on the removal method and whether underlying lipid abnormalities are addressed. Surgical excision offers the lowest recurrence rates. Working with your physician to manage cholesterol levels significantly reduces recurrence risk.
When performed by experienced surgeons, xanthelasma removal typically results in minimal, barely visible scarring that follows natural eyelid creases. The thin skin around the eyes heals with fine scars that continue to fade for 6-12 months. Most patients report high satisfaction with cosmetic outcomes.
The procedure itself is performed under local anesthesia and is not painful. After surgery, most patients experience only mild discomfort that is easily controlled with over-the-counter pain medication like paracetamol[2][3][7]. Pain typically peaks in the first 24-48 hours and decreases rapidly thereafter.
Most patients with desk jobs can return to work within 24-48 hours[4], though some prefer to take 3-5 days off for cosmetic reasons while swelling and bruising are most visible. Jobs requiring heavy physical labor may require 1-2 weeks off. Discuss your specific occupation with your surgeon for personalized guidance.
Healing occurs at the same rate whether one or both eyes are treated, but having only one eye affected allows for easier comparison and may make asymmetry during healing more noticeable. This is temporary and resolves as healing completes.
Most surgeons recommend avoiding contact lenses for at least 1-2 weeks after xanthelasma removal, particularly if the lower eyelid was treated. Glasses are a safer option during the initial healing period. Consult your surgeon for specific guidance based on your procedure.
Pain levels are generally comparable to or less than other minor skin surgeries. The eyelid area is sensitive, but the procedures are typically quick and performed with excellent local anesthesia. Post-operative discomfort is usually mild and well-controlled with simple pain medication.
If a scab falls off naturally (without picking), simply continue your normal aftercare routine with gentle cleansing and antibiotic ointment application. If you accidentally remove a scab prematurely, apply gentle pressure if any bleeding occurs, then continue ointment application and monitor for signs of infection.
Understanding xanthelasma surgery recovery time empowers you to make informed decisions, prepare adequately, and achieve optimal outcomes. While individual experiences vary, most patients find the recovery process manageable with minimal disruption to daily life.
🎯 Timeline Expectations:
💊 Aftercare Essentials:
🚨 When to Seek Help:
If You're Considering Xanthelasma Removal:
If You've Recently Had Xanthelasma Removal:
Choosing an experienced surgeon significantly impacts both your recovery experience and final cosmetic outcome. Look for providers who:
The xanthelasma surgery recovery time is typically short and manageable, with most patients experiencing minimal disruption to their lives while achieving significant cosmetic improvement. By understanding what to expect, preparing adequately, and following expert guidance, you can navigate the recovery process with confidence and achieve results that enhance both your appearance and self-esteem.
Remember that every patient's healing journey is unique. While this guide provides comprehensive information based on typical experiences and clinical evidence, your individual recovery may vary. Always defer to your surgeon's specific instructions, which are tailored to your unique situation, and don't hesitate to reach out with questions or concerns throughout your healing process.
[1] Xanthelasma Removal Surgery - https://www.nuffieldhealth.com/treatments/xanthelasma-removal-surgery
[2] What To Expect After Xanthelasma Removal Surgery - https://bluefinvision.com/knowledge-base/topics/recovery-aftercare/what-to-expect-after-xanthelasma-removal-surgery/
[3] Recovery From Xanthelasma Surgery - https://simonpayne.co.uk/recovery-from-xanthelasma-surgery/
[4] Xanthelasma - https://www.drjessicalattman.com/medical/xanthelasma/
[5] What To Do After Xanthelasma Laser Treatment - https://www.yildizacarebcim.com/en/what-to-do-after-xanthelasma-laser-treatment/
[6] Xanthelasma Removal Recovery - https://bluefinvision.com/knowledge-base/topics/recovery-aftercare/xanthelasma-removal-recovery/
[7] Xanthelasma Removal - https://oleloclinic.com/condition/xanthelasma-removal/
[8] Removing Xanthelasma On The Upper Eyelids - https://contourderm.com/removing-xanthelasma-on-the-upper-eyelids/
[9] Xanthelasma Surgery - https://myrontanenbaummd.com/xanthelasma-surgery/
[10] Laser For Xanthelasma - https://aesthetic-solutions.com/treatments/laser-for-xanthelasma/