When it comes to skin cancer, early detection can literally be a matter of life and death. Among all skin cancers, melanoma stands as the most dangerous, yet it's also one of the most treatable when caught early. Understanding what melanoma looks like empowers individuals to take control of their health and seek timely medical attention when necessary.
Melanoma develops in melanocytes, the cells responsible for producing melanin, which gives skin its color. While this form of skin cancer accounts for only about 1% of all skin cancer cases, it causes the majority of skin cancer deaths. The good news? When people know what to look for, melanoma can often be detected before it spreads to other parts of the body.
This comprehensive guide will walk readers through the visual characteristics of melanoma, helping them distinguish between normal moles and potentially dangerous lesions. From the famous ABCDE rule to understanding different types of melanoma, this article provides the knowledge needed to protect oneself and loved ones from this serious condition.
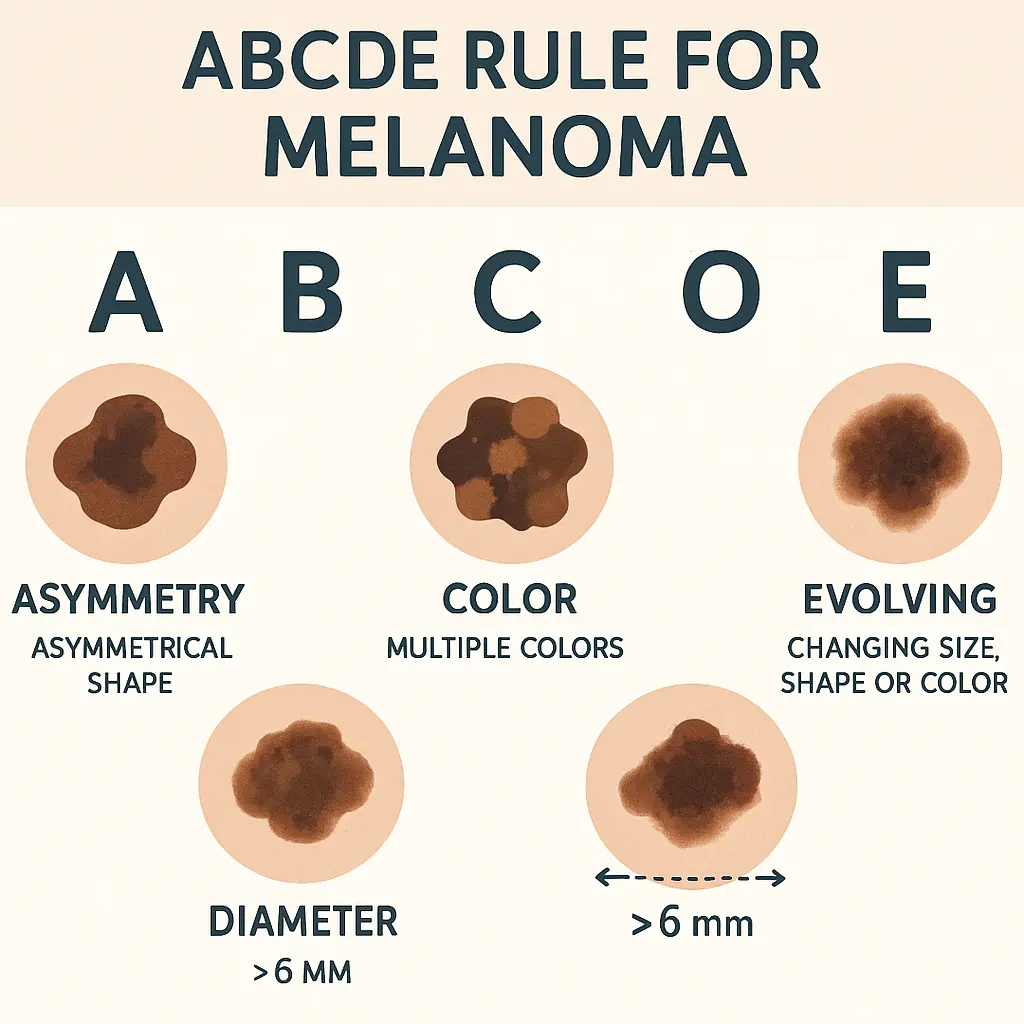
• The ABCDE rule (Asymmetry, Border, Color, Diameter, Evolving) remains the gold standard for identifying suspicious moles that could be melanoma
• Melanoma can appear anywhere on the body, not just sun-exposed areas, and can develop in existing moles or as new growths • Early-stage melanoma is highly treatable with a 99% five-year survival rate when caught before spreading • Regular self-examinations combined with professional skin checks are crucial for early detection • Any changing, unusual, or concerning skin lesion should be evaluated by a healthcare professional immediately
Before diving into what melanoma looks like, it's essential to understand what this cancer actually is. Melanoma begins in melanocytes, specialized cells that produce melanin - the pigment that gives skin, hair, and eyes their color. When these cells become damaged, typically by ultraviolet (UV) radiation from the sun or tanning beds, they can grow uncontrollably and form malignant tumors.
Unlike other forms of skin cancer that tend to grow slowly and rarely spread, melanoma has an aggressive nature. It can:
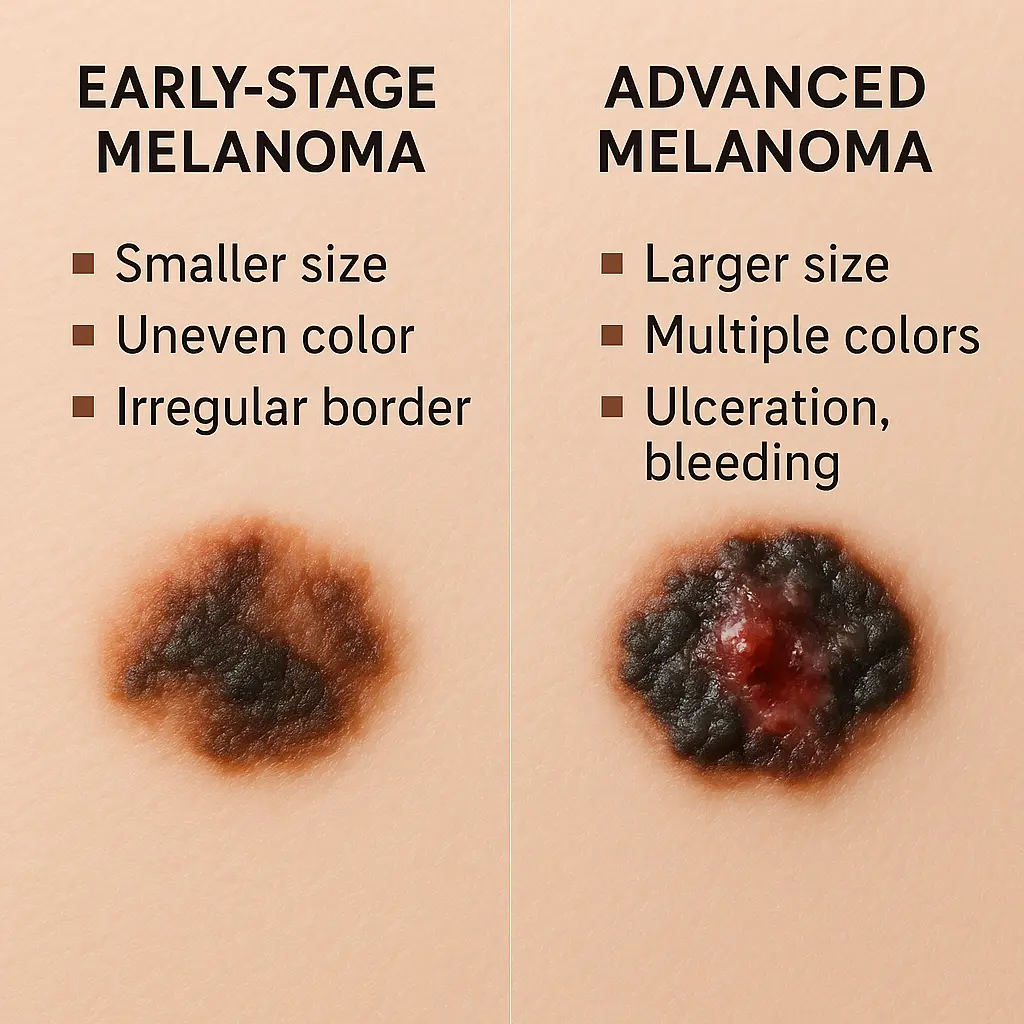
The key to survival lies in early detection. When melanoma is caught in its earliest stages, before it has penetrated deeply into the skin, the five-year survival rate exceeds 99%. However, once it spreads to distant organs, this rate drops dramatically to around 27%.
Healthcare professionals worldwide rely on the ABCDE rule when teaching patients what melanoma looks like. This simple acronym provides a systematic way to evaluate moles and skin lesions for signs of potential malignancy.
Normal moles are typically symmetrical, meaning if you draw a line through the middle, both halves match. Melanomas often display asymmetry, where one half looks different from the other half.
What to look for:
Benign moles usually have smooth, even borders. Melanomas frequently exhibit irregular, scalloped, or poorly defined borders.
Warning signs include:
Most normal moles are a single shade of brown. Melanomas often display multiple colors or unusual color variations.
Concerning colors include:
While melanomas can be any size, many are larger than 6 millimeters (about the size of a pencil eraser) when diagnosed. However, melanomas can be smaller, so size alone shouldn't be the determining factor.
Size considerations:
Perhaps the most important factor is change. Any mole that's evolving - changing in size, shape, color, elevation, or developing new symptoms like bleeding, itching, or crusting - should be examined by a healthcare professional.
Signs of evolution:
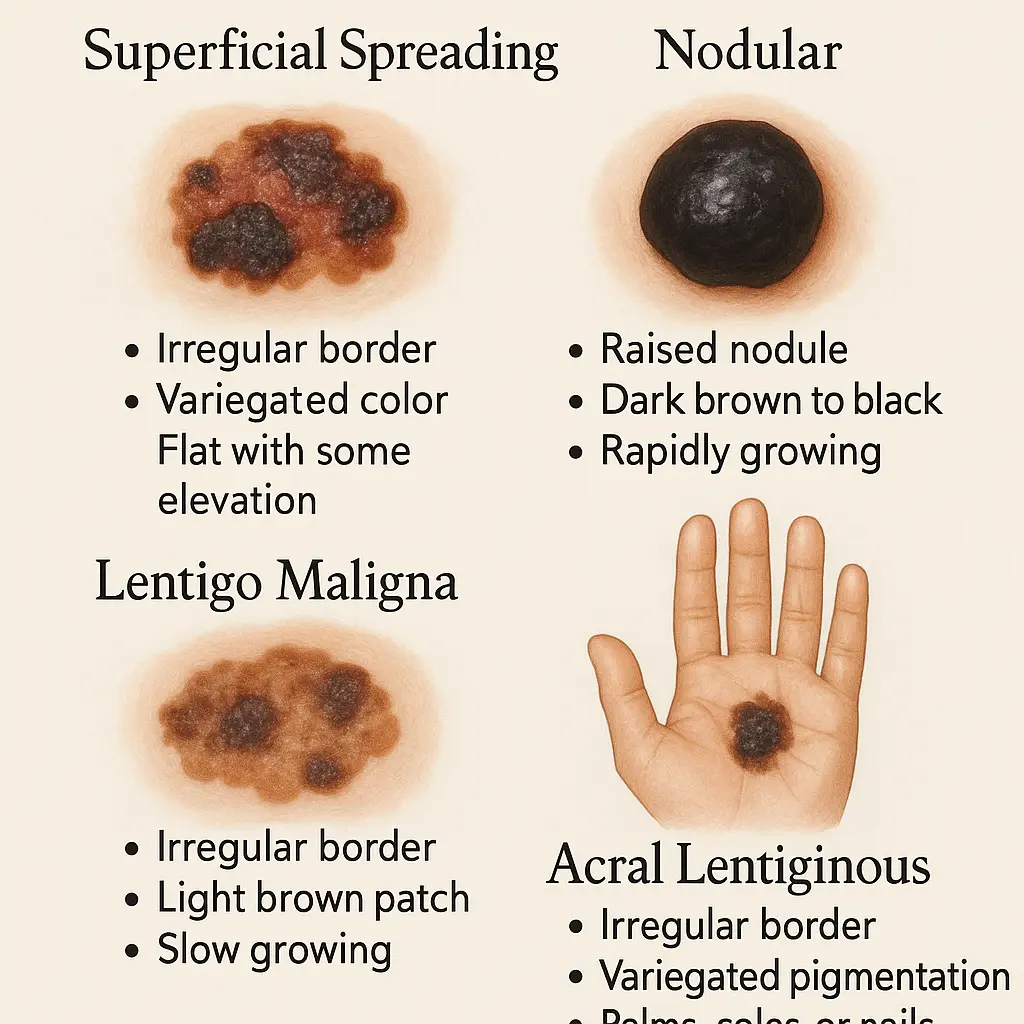
Understanding what melanoma looks like requires knowledge of its various types, as each can present differently. The four main types of melanoma each have distinct characteristics and patterns of growth.
This is the most common type, accounting for about 70% of all melanomas. It typically develops from existing moles and grows outward across the skin surface before penetrating deeper.
Appearance characteristics:
Common locations:
This aggressive form grows quickly and penetrates deep into the skin. It accounts for about 15-20% of melanomas and is often more advanced at diagnosis.
Distinctive features:
Warning signs:
This type typically develops in areas with chronic sun damage, particularly in older adults. It often starts as lentigo maligna (melanoma in situ) before becoming invasive.
Characteristic appearance:
Typical locations:
This rare form occurs on the palms, soles, or under the nails. It's the most common type of melanoma in people with darker skin tones.
Identifying features:
Special considerations:
One of the most important aspects of understanding what melanoma looks like involves knowing where it can appear. Contrary to popular belief, melanoma doesn't only develop in sun-exposed areas.

Sun-exposed areas:
Hidden areas:
Men: Most commonly develop melanoma on the back, chest, and head Women: Most frequently affected on the legs and back People with darker skin: More likely to develop acral lentiginous melanoma on palms, soles, and nail beds Elderly individuals: Higher risk on the face and other chronically sun-exposed areas
For those seeking professional evaluation of suspicious lesions, specialized clinics offer comprehensive skin cancer screening and treatment options.
Understanding the progression of melanoma helps in recognizing what to look for at different stages of the disease.
Stage 0 (Melanoma in situ):
Stage I (Early invasive):
Stage II and beyond:
Certain characteristics of skin lesions require urgent medical evaluation. These red flags indicate potentially dangerous melanoma that needs immediate attention.
Immediate medical attention needed for:
Dermatologists often refer to the "ugly duckling" sign - a mole that looks different from all the others on a person's body. This outlier mole often warrants closer examination, even if it doesn't follow the traditional ABCDE rules.
Characteristics of "ugly duckling" moles:
Healthcare professionals at specialized treatment centers can provide expert evaluation of concerning lesions and recommend appropriate treatment options.
Regular self-examination is crucial for early melanoma detection. Performing monthly skin checks helps individuals become familiar with their normal moles and spot changes early.
Step 1: Preparation
Step 2: Systematic Examination
Step 3: Documentation
Week 1: Upper body (head, neck, arms, chest, back) Week 2: Lower body (abdomen, legs, feet) Week 3: Hidden areas (scalp, between digits, genital area) Week 4: Review documentation and schedule professional checks
While self-examination is important, professional medical evaluation remains the gold standard for melanoma diagnosis. Healthcare providers use various tools and techniques to accurately identify suspicious lesions.
Dermatoscopy allows doctors to see details invisible to the naked eye:
Digital imaging systems:
When a lesion appears suspicious, doctors may recommend a biopsy:
Types of biopsies:
The choice of biopsy method depends on the lesion's size, location, and suspected depth of invasion.
Understanding personal risk factors helps individuals know what to watch for and how melanoma might appear on their specific skin type.
Genetic factors:
Environmental factors:
Fair-skinned individuals:
Darker-skinned individuals:
For comprehensive information about various skin conditions and their management, patients can explore detailed condition resources that provide expert guidance on recognition and treatment options.
Several myths persist about what melanoma looks like, potentially delaying diagnosis and treatment. Dispelling these misconceptions is crucial for proper recognition.
Myth: "Melanoma is always black or very dark" Reality: Melanoma can be pink, red, white, or skin-colored (amelanotic melanoma)
Myth: "Melanoma only occurs in sun-exposed areas" Reality: Melanoma can develop anywhere on the body, including areas never exposed to sun
Myth: "Small moles can't be melanoma" Reality: Some melanomas are smaller than 6mm when first detected
Myth: "Melanoma always develops from existing moles" Reality: About 70% of melanomas arise in normal skin, not from pre-existing moles
Myth: "Young people don't get melanoma" Reality: Melanoma is one of the most common cancers in young adults, particularly women aged 25-29
"It doesn't hurt, so it's not cancer"
"It's been there for years, so it's fine"
Modern technology has revolutionized melanoma detection, providing tools that enhance both professional diagnosis and patient awareness.
Advantages of technology-assisted detection:
Limitations to remember:
Artificial Intelligence (AI) systems:
Multispectral imaging:
While understanding what melanoma looks like is crucial, prevention remains the best strategy for reducing melanoma risk.
Daily protection habits:
Special considerations:
Recommended frequency:
High-risk individuals should see dermatologists more frequently:
For those seeking expert evaluation and care, professional medical teams provide specialized expertise in skin cancer detection and treatment.
Understanding what melanoma looks like naturally leads to questions about treatment and outcomes. Early detection dramatically improves prognosis and treatment options.
Surgical options:
Success rates:
Immunotherapy:
Targeted therapy:
Traditional treatments:
For individuals at high risk or those who have had melanoma, ongoing vigilance becomes a way of life.
Follow-up care includes:
Lifestyle modifications:
Genetic counseling may be recommended for:
For additional information and frequently asked questions about melanoma and skin cancer, patients can access comprehensive FAQ resources that address common concerns and provide detailed guidance.
Public education about what melanoma looks like saves lives. The more people understand the warning signs, the earlier dangerous lesions can be detected and treated.
Educational initiatives include:
Target populations:
Continuing medical education focuses on:
Understanding what melanoma looks like empowers individuals to take control of their health and potentially save their lives. The ABCDE rule provides a systematic approach to evaluating suspicious moles, while knowledge of different melanoma types helps recognize various presentations of this dangerous cancer.
Key points to remember include the importance of regular self-examinations, professional skin checks, and immediate medical attention for any concerning changes. Melanoma can appear anywhere on the body and may not always follow typical patterns, making vigilance and education crucial for early detection.
The prognosis for melanoma depends heavily on early recognition and treatment. When caught in its earliest stages, melanoma is highly curable, with survival rates exceeding 99%. However, delayed diagnosis can lead to metastasis and significantly reduced survival rates.
Prevention through sun protection remains the best strategy, but for those at high risk or with suspicious lesions, professional medical evaluation is essential. Modern diagnostic tools and treatment options continue to improve outcomes for melanoma patients.
Immediate steps to protect yourself and your loved ones:
Don't wait for symptoms to develop - early melanoma rarely causes pain or discomfort. The visual changes described in this guide are often the only warning signs available.
For professional evaluation, expert treatment, and comprehensive skin cancer care, contact specialized medical centers that offer state-of-the-art diagnostic and treatment services.
Remember: When it comes to melanoma, early detection saves lives. Armed with knowledge about what melanoma looks like, individuals can be their own first line of defense against this serious but treatable form of cancer. The investment in regular skin checks and professional evaluation is minimal compared to the potential life-saving benefits of early detection and treatment.
Stay vigilant, stay protected, and don't hesitate to seek professional medical advice when in doubt. Your skin health is worth the attention and care that proper melanoma awareness provides.