You've just had a mole removed. The procedure went smoothly, and now you're waiting for something called a "pathology report."
Maybe your doctor mentioned it briefly, or perhaps you received a call saying your results are in. Either way, you're probably wondering: what does a pathology report mean after mole removal, and why does it matter?
Here's the truth: a pathology report is one of the most important documents you'll receive after any mole removal. It tells you exactly what that mole was made of, whether it poses any health risks, and what (if anything) you need to do next.
At The Minor Surgery Center, we understand that waiting for medical results can feel unsettling. That's why our experienced surgical team believes in clear communication every step of the way—from your initial consultation through your pathology results and beyond. We're here to help you understand what these reports mean and get back to your life with confidence.
When a surgeon removes a mole, they don't just toss it away. That small piece of tissue goes straight to a pathology laboratory, where a specialized doctor called a pathologist examines it under a microscope.
Think of it like this: your mole is telling a story at the cellular level. The pathologist reads that story and translates it into a report that answers critical questions.
Your pathology report provides answers to several important questions:
These aren't just academic questions. The answers directly impact your health and determine your next steps.
At The Minor Surgery Center, we believe that removing a mole is only half the job. Understanding what that mole was—through thorough pathology analysis—completes the picture.
Our comfort-first approach means we never rush through explanations. When your pathology report arrives, we take the time to walk you through the findings, answer your questions, and create a personalized treatment plan if needed.
This commitment to transparency is what sets expert outpatient care apart from rushed appointments where you're left wondering what your results really mean.
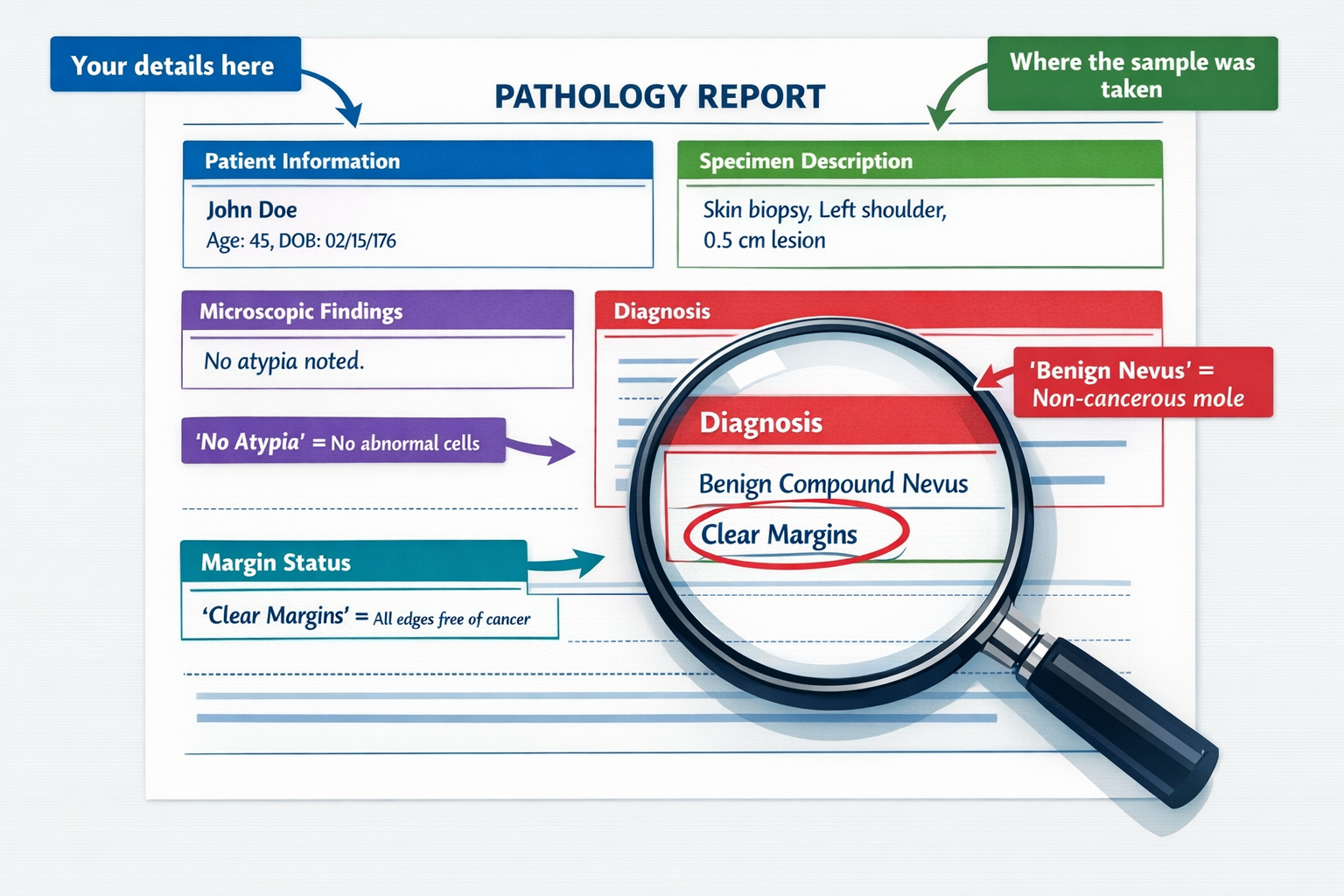
Let's break down what you'll actually see when you look at a pathology report. These documents can seem intimidating at first—they're filled with medical terminology and technical descriptions. But once you understand the basic structure, they become much easier to navigate.
Most pathology reports follow a standard format. Here's what you'll typically find:
This section confirms your identity and includes basic information about why the mole was removed. It might mention:
This describes what the pathologist received in the lab. It includes:
For example: "The specimen consists of a 0.6 cm tan-brown skin lesion with surrounding normal skin."
This is where the real detective work happens. The pathologist describes what they see when examining thin slices of your mole tissue under a microscope.
They look at:
This is the most important section—the pathologist's conclusion about what your mole actually was. Common diagnoses include:
This tells you whether the mole was completely removed. You'll see terms like:
The pathologist may include notes about:
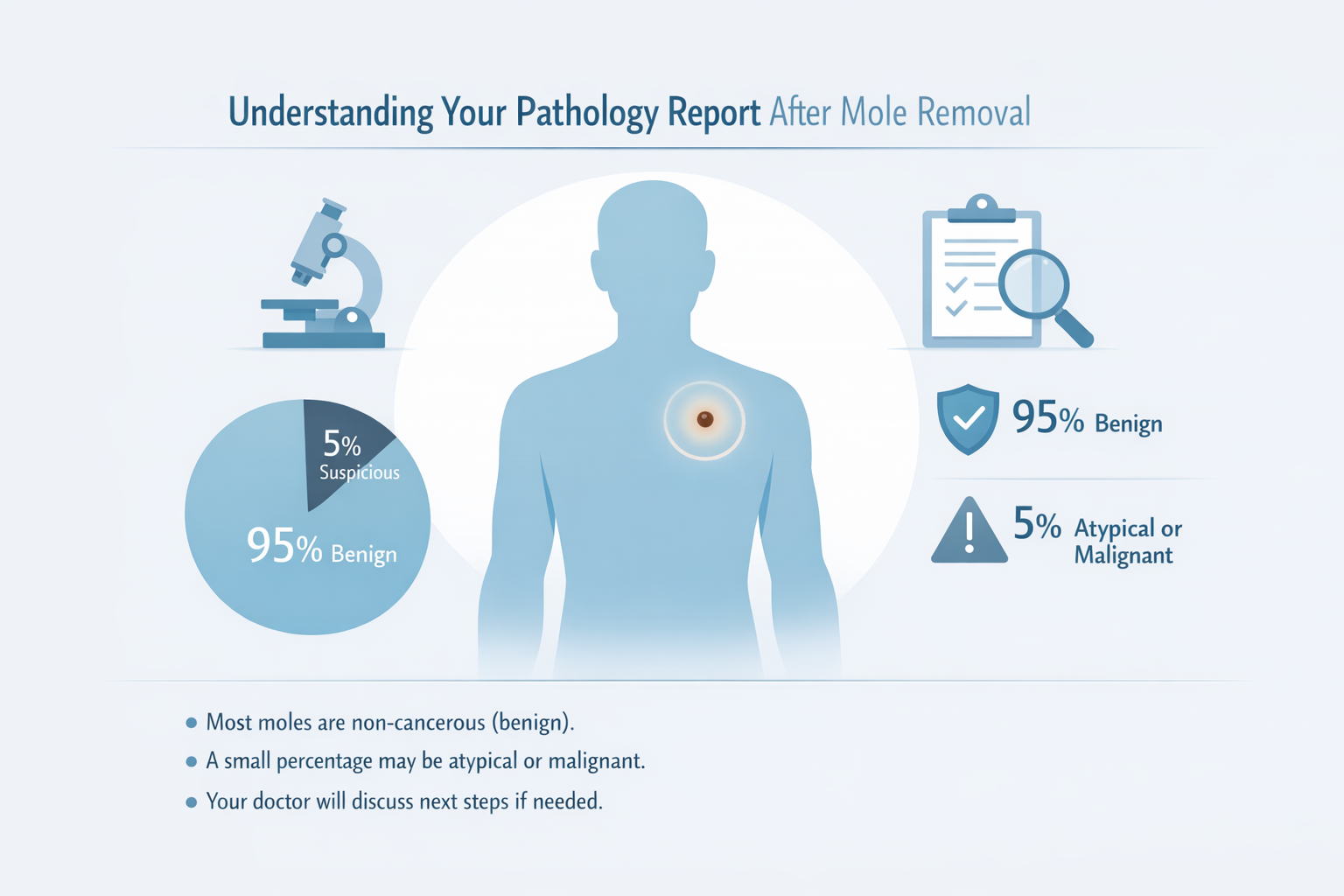
Now that you understand the structure, let's dive into what different diagnoses actually mean. Remember: most moles are benign. But understanding the full spectrum helps you interpret your specific results.
Good news: this is what most pathology reports show.
When your report says "benign," it means the mole was harmless. Common benign diagnoses include:
This is the medical term for a regular mole. It contains melanocytes (pigment-producing cells) in both the outer layer (epidermis) and deeper layer (dermis) of skin.
What it means for you: Nothing to worry about. The mole was normal, and you don't need any further treatment.
Similar to a compound nevus, but the melanocytes are only in the junction between the epidermis and dermis.
What it means for you: Also benign and requires no further action.
The melanocytes are entirely within the dermis (deeper skin layer). These moles are often flesh-colored or slightly raised.
What it means for you: Completely harmless. You're good to go.
This isn't technically a mole—it's a different type of benign skin growth that can look similar to a mole. They're extremely common, especially as we age.
What it means for you: Totally harmless. These are sometimes called "wisdom spots" because they're so common in adults.
An atypical or dysplastic mole sits in a gray area. It's not cancer, but it has some unusual features under the microscope.
What it means for you:
Atypical moles deserve attention because:
Your next steps:
Think of an atypical mole like a yellow traffic light—not an emergency, but a signal to proceed with caution and stay alert.
If your pathology report shows melanoma or another type of skin cancer, it's understandably concerning. But here's what's important to know: early detection makes all the difference.
This is the most serious type of skin cancer, but when caught early, it's highly treatable.
Your report will include important details:
What it means for you:
Your next steps:
This is the most common type of skin cancer. It grows slowly and rarely spreads to other parts of the body.
What it means for you: While it's cancer, BCC is highly treatable and rarely life-threatening. Complete removal usually solves the problem.
This is the second most common skin cancer. It can occasionally spread if not treated, but early treatment is very effective.
What it means for you: You'll need to ensure complete removal and may need regular monitoring.
Pathology reports are written in medical language. Here's a quick translation guide for common terms you might encounter:
Medical TermWhat It Means in Plain EnglishNevusMoleBenignNot cancerous; harmlessMalignantCancerousDysplastic/AtypicalUnusual appearance; not normal but not cancerMarginsThe edges of the removed tissueClear/Negative marginsThe entire mole was removed with healthy tissue around itPositive marginsSome mole cells extend to the edge of what was removedBreslow thicknessHow deep a melanoma goes into the skinMitotic figuresCells that are actively dividing (higher numbers can indicate more aggressive growth)AtypiaAbnormal cell featuresJunctional activityCell activity at the junction between skin layersUlcerationA break or erosion in the skin surfacePigmentationColor or darkness of the cells
Medical terminology can sound scary even when describing something completely harmless. A "compound melanocytic nevus with junctional activity" sounds alarming—but it's just a regular mole.
This is why discussing your report with your doctor is so important. At The Minor Surgery Center, our experienced surgical team translates medical jargon into clear, understandable language so you know exactly what your results mean.
Understanding what does a pathology report mean after mole removal is just the first step. What matters next is taking the right action based on your results.
Congratulations! This is the outcome for most people.
Your next steps:
Think of it like resetting the clock on this particular worry. You took the right step by having the mole evaluated, and now you can move forward with confidence.
You're in the "watch and monitor" category.
Your next steps:
Your personalized treatment plan might include more frequent check-ups or a lower threshold for removing other suspicious spots.
This requires prompt action, but remember: early detection is powerful.
Your next steps:
Here's what's important to understand: Modern treatment for skin cancer—especially when caught early—is highly effective. The five-year survival rate for melanoma caught in its earliest stage is over 99%.
At The Minor Surgery Center, we never leave you wondering what comes next. When your pathology report arrives:
✅ We contact you promptly with results
✅ We explain what the findings mean in clear, everyday language
✅ We answer all your questions (no matter how small they seem)
✅ We create a personalized treatment plan if further action is needed
✅ We coordinate referrals to specialists when appropriate
This transparent approach is part of our commitment to expert outpatient care that puts your understanding and comfort first.
One of the most important parts of understanding what does a pathology report mean after mole removal is grasping the concept of "margins."
When a surgeon removes a mole, they don't just cut out the visible spot. They also remove a small border of normal-looking skin around it. This border is called the "margin."
Think of it like cutting a stain out of fabric. You wouldn't cut exactly along the stain's edge—you'd cut a little beyond it to make sure you got everything.
The margin status tells you whether the entire mole was removed:
This means healthy tissue surrounds the mole on all sides. No mole cells extend to the edge of what was removed.
What it means: The mole was completely removed. For benign moles, you're done. For malignant lesions, this is excellent news and may mean no further surgery is needed.
This means mole cells extend to the edge of the removed tissue. Some of the mole may still remain in your skin.
What it means:
Sometimes the margins are clear but narrow—the healthy tissue border is very thin.
What it means: Technically complete removal, but your doctor might recommend additional removal depending on the diagnosis and location.
Pathology reports often include specific measurements, like "margins clear by 2mm" or "margins clear by 0.5mm."
These numbers tell you how much healthy tissue surrounds the mole. For melanoma, wider margins are important—sometimes 1-2 centimeters of healthy tissue is recommended depending on the thickness of the melanoma.
Most pathology reports come back within 5-10 business days after your mole removal. Some complex cases might take slightly longer if special stains or additional testing is needed.
At The Minor Surgery Center, we process pathology efficiently and contact you as soon as results are available. We know waiting can be stressful, so we work to minimize that uncertainty.
First, take a breath. Unexpected findings don't automatically mean bad news—sometimes it just means the mole was different than it appeared visually.
Your doctor will contact you to discuss the findings and next steps. This is where our commitment to clear communication really matters. We'll explain what was found, what it means for your health, and what (if anything) needs to happen next.
For benign findings, a second opinion usually isn't necessary. But if your report shows:
...then seeking a second pathology opinion can be valuable. Some patients send their slides to a specialized dermatopathologist for review.
Pathology is highly accurate, but like all medical tests, it's not 100% perfect. Errors are rare but can happen due to:
This is why choosing a facility with experienced professionals and quality control measures matters. At The Minor Surgery Center, we work with accredited pathology laboratories that maintain the highest standards.
This is completely normal. Pathology reports aren't written for patients—they're written for doctors.
Never hesitate to ask questions. Our experienced surgical team is here to translate medical terminology into language that makes sense. We encourage you to:
Understanding your health information is your right, and we're committed to making sure that happens.
Here's something many people don't realize: the quality of your pathology report starts with the quality of your mole removal.
When a mole is removed correctly:
Poor removal technique can lead to:
At The Minor Surgery Center, our minimally invasive solutions are designed with pathology in mind from the start.
Our experienced surgical team:
✅ Uses appropriate removal techniques based on the mole's appearance and location
✅ Removes adequate tissue to ensure complete excision and clear pathology
✅ Handles specimens carefully to preserve tissue quality
✅ Provides detailed clinical information to the pathologist
✅ Works with accredited laboratories that maintain high standards
This attention to detail—from the first incision through the final pathology report—is what safe and efficient surgery looks like.
Our goal isn't just to remove a mole. It's to provide you with clear answers, peace of mind, and the ability to move forward confidently.
Whether your pathology report shows a benign mole or something that requires further attention, you'll have the information and support you need to take the right next steps.
Understanding what does a pathology report mean after mole removal is important—but so is knowing when to have a mole evaluated in the first place.
Remember the ABCDE rule for concerning moles:
You should also have a mole evaluated if it:
Sometimes a mole stands out because it looks different from all your others. Even if it doesn't meet the ABCDE criteria, a mole that looks like the "ugly duckling" in your flock deserves evaluation.
You should be extra attentive to mole changes if you have:
Sometimes people choose to remove moles even when they're not obviously concerning:
All of these are valid reasons. And the benefit is that removal gives you pathology confirmation—turning "probably fine" into "definitely fine."
If you're considering mole removal, here's what to expect throughout the process:
Your consultation includes:
At The Minor Surgery Center, this consultation is part of our comfort-first approach. We want you to feel informed and at ease before any procedure.
Mole removal is typically quick and straightforward:
Our experienced surgical team performs these procedures daily, combining technical expertise with a gentle, reassuring manner.
Immediate aftercare:
Waiting for results:
Receiving your results:
This entire process reflects our commitment to expert outpatient care that respects your time, addresses your concerns, and keeps you informed every step of the way.
Understanding what does a pathology report mean after mole removal empowers you to take an active role in your skin health.
Make skin self-exams a regular habit:
Think of it as a routine maintenance check—like changing the oil in your car or checking your smoke detectors.
Reduce your risk of new concerning moles:
These habits benefit everyone, but they're especially important if you've had atypical moles or skin cancer.
How often should you see a dermatologist or skin specialist?
Your doctor will recommend a schedule based on your individual risk factors.
Continuity of care matters. When you work with the same healthcare providers over time:
At The Minor Surgery Center, we value long-term relationships with our patients. We're not just here for a single procedure—we're here to support your ongoing health and well-being.
Let's look at a few examples of how pathology reports play out in real situations:
Sarah's story: Sarah, 34, had a dark mole on her shoulder that had been there for years. It hadn't changed, but she wanted it removed because it caught on her bra strap.
Pathology result: Benign compound nevus with clear margins.
What happened next: Sarah received a call with the good news. No further treatment needed. She was relieved to have confirmation that the mole was harmless and happy to have it gone.
Outcome: Sarah got back to her life immediately, minus the annoying mole.
James's story: James, 52, noticed a mole on his back that looked different from his others—larger and with irregular borders.
Pathology result: Moderately dysplastic nevus with clear margins.
What happened next: His doctor explained that while the mole wasn't cancer, it had atypical features. James scheduled a full-body skin check, which revealed two other suspicious moles. These were also removed and came back atypical. James now has skin checks every six months.
Outcome: James is being monitored carefully, and any future concerning spots will be caught early. His proactive approach is protecting his long-term health.
Linda's story: Linda, 61, had a small, changing mole on her calf. It had darkened and grown slightly over six months.
Pathology result: Melanoma in situ (confined to the top layer of skin) with close margins.
What happened next: Linda underwent a wider excision to ensure complete removal with adequate margins. The second pathology report showed clear margins and no remaining melanoma. She now has quarterly skin checks and is vigilant about sun protection.
Outcome: Because Linda acted quickly when she noticed changes, the melanoma was caught at the earliest possible stage. Her prognosis is excellent, and she's back to enjoying her life—including her favorite outdoor activities, now with better sun protection.
Let's acknowledge something important: waiting for medical test results is stressful.
Even though most moles are benign, it's completely natural to worry while waiting for your pathology report. You might find yourself:
This is a normal human response to medical uncertainty.
Try these approaches:
If the news is good:
Allow yourself to feel relief. You took the right step by having the mole evaluated, and now you can move forward with confidence.
If the news is concerning:
Remember that knowledge is power. A diagnosis—even an unexpected one—gives you the information you need to take appropriate action. Modern treatment for skin issues, including skin cancer, is highly effective, especially when caught early.
At The Minor Surgery Center, we understand that medical procedures involve emotions, not just tissues and test results. Our compassionate approach means:
You're not just a case number to us—you're a person with concerns, questions, and a life you want to get back to living fully.
So, what does a pathology report mean after mole removal?
It means clarity. It means answers. It means knowing exactly what that spot on your skin was and what (if anything) you need to do about it.
For most people, a pathology report brings welcome relief—confirmation that a concerning mole was actually harmless. For others, it provides early detection of something that needs attention, giving you the best possible chance for successful treatment.
Either way, understanding your pathology report empowers you to make informed decisions about your health and move forward with confidence.
If you have a mole that concerns you:
If you've already had a mole removed:
If you're looking for a partner in your skin health:
At The Minor Surgery Center, we're here to help. Our experienced surgical team provides minimally invasive solutions with a comfort-first approach. From your initial consultation through your pathology results and beyond, we're committed to clear communication, personalized care, and helping you get back to your life with confidence.
We believe that excellent medical care combines technical expertise with genuine compassion. That means:
✅ Taking time to explain things clearly
✅ Answering every question thoroughly
✅ Providing safe and efficient surgery
✅ Supporting you through every step of the process
Your skin health matters. Your peace of mind matters. And you deserve care that treats both with equal importance.
Ready to take the next step? Whether you have a concerning mole, questions about a pathology report, or simply want to discuss your skin health, we're here to help. Contact The Minor Surgery Center today to schedule a consultation with our experienced surgical team. Let's work together to create a personalized treatment plan that addresses your concerns and helps you move forward with confidence.
Because life is too short to spend it worrying about spots on your skin. Let's get you the answers you need so you can get back to living your life fully.