Have you ever noticed a new dark spot on your skin and wondered where it came from? You're not alone. Many people experience the sudden appearance of moles throughout their lives, often causing concern and confusion. While most new moles are harmless, understanding what causes moles to suddenly appear can help individuals make informed decisions about their skin health and know when to seek medical attention.
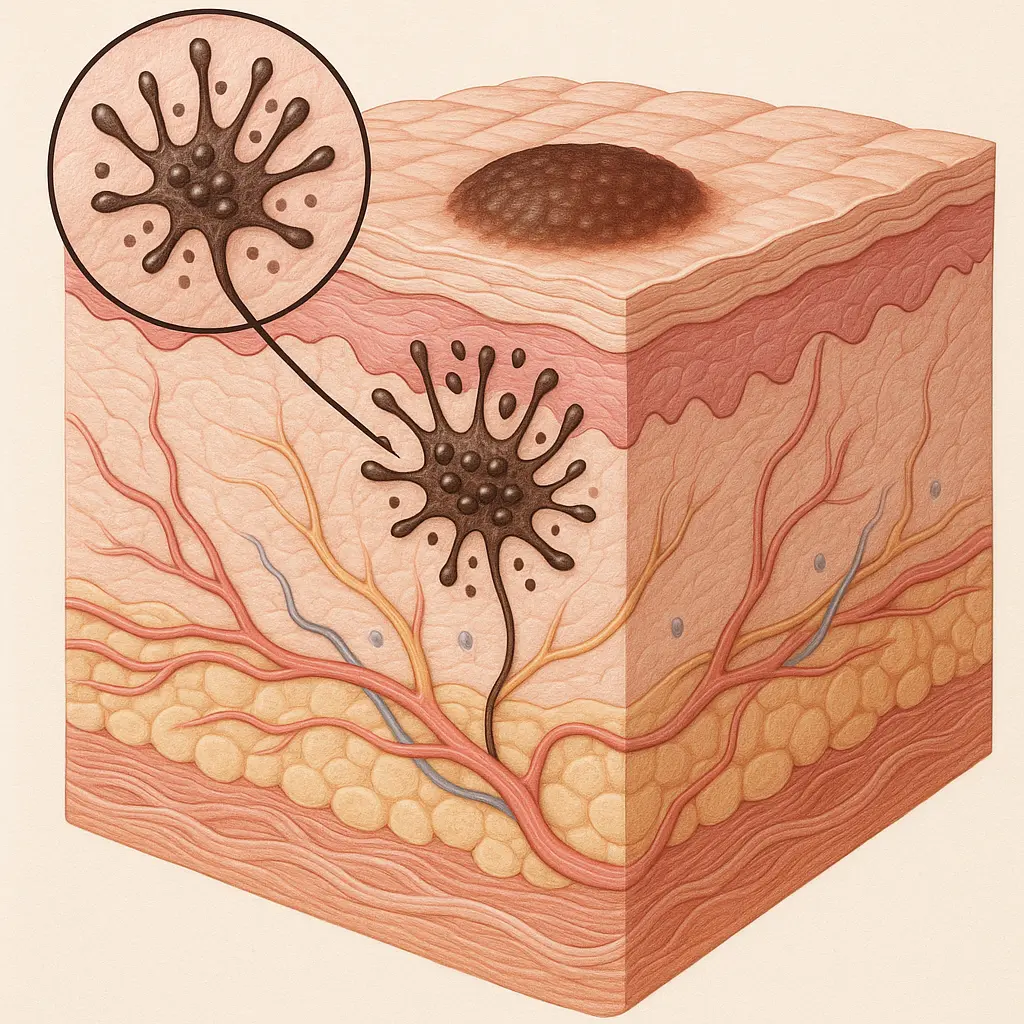
Moles, medically known as nevi, are common skin growths that can develop at any stage of life. These pigmented spots result from clusters of melanocytes—the cells responsible for producing melanin, the pigment that gives skin its color. While some people are born with moles, others develop them gradually or notice their sudden appearance, particularly during certain life stages or following specific triggers.
The phenomenon of new mole development is more common than many realize, with the average person developing between 10 to 40 moles throughout their lifetime. However, the sudden appearance of moles can be influenced by various factors, ranging from genetic predisposition and hormonal changes to environmental exposures and aging processes.
• Hormonal fluctuations during puberty, pregnancy, and menopause are primary triggers for sudden mole appearance
• Sun exposure and UV radiation significantly increase the likelihood of developing new moles at any age • Genetic factors play a crucial role in determining an individual's predisposition to mole development • Most new moles are benign, but changes in existing moles or unusual characteristics warrant medical evaluation • Regular skin monitoring and professional dermatological assessments are essential for early detection of concerning changes
Moles are benign skin growths that form when melanocytes cluster together instead of spreading evenly throughout the skin. These specialized cells produce melanin, which determines skin, hair, and eye color. When melanocytes accumulate in concentrated areas, they create the characteristic dark spots known as moles.
The formation process involves several cellular mechanisms:
Understanding the different types of moles helps explain why some appear suddenly while others develop gradually:
Congenital Moles 🎯
Acquired Moles ✨
Atypical Moles (Dysplastic Nevi) ⚠️
Hormonal fluctuations represent one of the most significant factors in understanding what causes moles to suddenly appear. The endocrine system's impact on skin cell behavior is profound and multifaceted.
Puberty and Adolescence 🌱 During puberty, dramatic hormonal changes trigger various skin transformations. Increased levels of growth hormones, estrogen, and testosterone can stimulate melanocyte activity, leading to new mole formation. This explains why many teenagers notice an increase in mole development during their adolescent years.
Pregnancy-Related Changes 🤱 Pregnancy brings significant hormonal shifts that can cause existing moles to darken and new ones to appear. Elevated levels of estrogen and progesterone during pregnancy can stimulate melanin production, making moles more prominent and encouraging new growth. Many women report noticing new moles during their second and third trimesters.
Menopause Transitions 🌸 The hormonal fluctuations associated with menopause can also trigger new mole development. As estrogen levels decline and fluctuate, some women experience changes in their skin's pigmentation patterns, including the appearance of new moles.
For comprehensive information about skin conditions and their treatments, individuals can explore resources at The Minor Surgery Center's conditions page.
Ultraviolet (UV) radiation serves as a primary environmental trigger for sudden mole appearance. Understanding this relationship is crucial for prevention and early detection strategies.
Acute Sun Exposure Events ☀️ Intense, short-term sun exposure—such as severe sunburns—can trigger cellular changes that lead to mole development weeks or months later. The DNA damage caused by UV radiation can alter melanocyte behavior, causing them to cluster and form new moles.
Cumulative UV Damage 📊 Long-term sun exposure creates cumulative cellular damage that may manifest as new moles years after the initial exposure. This explains why some individuals notice new moles appearing in areas that were frequently exposed to sunlight during their youth.
Artificial UV Sources 💡 Tanning beds and other artificial UV sources can trigger the same cellular responses as natural sunlight, potentially causing new moles to develop. The concentrated nature of artificial UV radiation may even accelerate this process compared to natural sun exposure.
Genetic factors significantly influence an individual's likelihood of developing new moles throughout their lifetime. Understanding these hereditary components helps explain why moles suddenly appear in some people more than others.
Inherited Susceptibility 🧬 Certain genetic variations affect melanocyte behavior and sensitivity to environmental triggers. Individuals with family histories of numerous moles or skin cancer often have genetic predispositions that make them more likely to develop new moles throughout their lives.
Skin Type Considerations 🎨 Genetic factors that determine skin type, hair color, and eye color also influence mole development patterns. People with lighter skin tones, red or blonde hair, and blue or green eyes typically have genetic variants that increase their susceptibility to UV-induced mole formation.
The relationship between age and mole development follows predictable patterns that help explain when and why new moles are most likely to appear.
Early Childhood (Ages 2-10) 👶 Most children begin developing their first acquired moles during early childhood. This period typically sees the gradual appearance of small, round moles that may seem to appear suddenly to observant parents.
Adolescent Growth Spurts (Ages 11-18) 🌟 The teenage years represent the peak period for new mole development. Hormonal changes, combined with accumulated sun exposure, create ideal conditions for sudden mole appearance. It's not uncommon for teenagers to develop 10-20 new moles during this period.
Young Adulthood (Ages 19-30) 💪 While mole development typically slows after adolescence, young adults may still notice occasional new moles, particularly following significant sun exposure or hormonal changes such as pregnancy.
Middle Age Considerations (Ages 31-50) 🎯 New mole development generally decreases during middle age, making sudden mole appearance more noticeable and potentially concerning. Any new moles developing after age 30 warrant closer attention and professional evaluation.
Senior Years (Ages 50+) 👴 While new mole development is less common in seniors, age-related skin changes can make existing moles more prominent or cause new pigmented lesions to appear. These changes require careful monitoring to distinguish between benign moles and potentially concerning growths.
For expert evaluation of new or changing moles, individuals should consider consulting with healthcare professionals at The Minor Surgery Center.
Environmental conditions play a significant role in determining what causes moles to suddenly appear in different populations and geographic regions.
High-Altitude Environments 🏔️ Living at high altitudes exposes individuals to increased UV radiation due to thinner atmospheric protection. This enhanced exposure can trigger more frequent mole development compared to sea-level environments.
Tropical and Subtropical Climates 🌴 Year-round sun exposure in tropical regions creates consistent environmental pressure for mole development. Individuals living in these climates often develop more moles throughout their lives compared to those in temperate regions.
Seasonal Exposure Patterns 🗓️ Many people notice new moles appearing several months after intense summer sun exposure. This delayed response reflects the time required for UV-induced cellular changes to manifest as visible moles.
Certain medications and chemical exposures can influence mole development by affecting melanocyte behavior or increasing photosensitivity.
Photosensitizing Medications 💊 Some medications increase skin sensitivity to UV radiation, potentially accelerating mole development. These include certain antibiotics, diuretics, and anti-inflammatory drugs.
Hormonal Medications 🔬 Birth control pills, hormone replacement therapy, and other hormonal treatments can influence mole development by altering the body's hormonal balance.
Chemical Exposures ⚗️ Occupational or environmental exposure to certain chemicals may influence skin cell behavior and contribute to mole development, though this relationship requires further research.
While most new moles are benign, certain characteristics warrant immediate medical attention. Understanding these warning signs helps individuals distinguish between normal mole development and potentially concerning changes.
The ABCDE Rule 📋 Medical professionals use the ABCDE criteria to evaluate concerning mole characteristics:
Rapid Development ⚡ Moles that appear and grow quickly over weeks rather than months may require professional evaluation. While rapid appearance doesn't automatically indicate malignancy, it warrants medical assessment.
Unusual Locations 🎯 New moles appearing in unusual locations—such as palms, soles, or nail beds—require special attention, particularly in individuals with darker skin tones where these locations are more commonly affected by certain types of skin cancer.
New Moles After Age 40 🔍 The appearance of new moles after age 40 is less common and may warrant closer evaluation. While many of these new growths are benign, the decreased frequency of normal mole development in this age group makes professional assessment advisable.
Multiple New Moles 📈 The sudden appearance of multiple new moles, particularly in adults, may indicate underlying factors that require medical evaluation. This pattern could suggest hormonal changes, medication effects, or other systemic influences.
Understanding when to consult healthcare professionals about new moles is crucial for maintaining optimal skin health. Professional evaluation becomes particularly important when certain patterns or characteristics emerge.
Immediate Consultation Scenarios 🚨
Routine Monitoring Guidelines 📅 Regular skin examinations, both self-performed and professional, play vital roles in early detection of concerning changes. Dermatologists typically recommend annual skin checks for most adults, with more frequent monitoring for high-risk individuals.
For professional mole evaluation and treatment options, patients can schedule consultations at The Minor Surgery Center's clinic.
Dermoscopy and Digital Imaging 🔬 Modern dermatological practices employ advanced diagnostic tools to evaluate moles more accurately. Dermoscopy allows detailed examination of mole structures invisible to the naked eye, while digital imaging systems track changes over time.
Biopsy Procedures 🧪 When moles exhibit concerning characteristics, dermatologists may recommend biopsy procedures to determine their nature. These minimally invasive procedures provide definitive diagnoses and guide appropriate treatment decisions.
Mapping and Tracking Systems 📊 Some medical practices use comprehensive mole mapping systems to document and track all moles on a patient's body. These systems excel at detecting subtle changes that might otherwise go unnoticed.
Implementing comprehensive sun protection strategies represents the most effective approach to preventing unnecessary mole development while maintaining healthy skin.
Daily Sun Protection Habits ☀️
Sunscreen Application Techniques 🧴 Proper sunscreen application requires attention to coverage, timing, and reapplication schedules. Most people apply insufficient amounts of sunscreen, reducing its effectiveness significantly.
Protective Clothing Considerations 👕 UV-protective clothing with UPF (Ultraviolet Protection Factor) ratings provides reliable protection without the need for frequent reapplication. Dark colors and tightly woven fabrics typically offer superior protection.
Dietary Considerations 🥗 While diet doesn't directly prevent mole formation, certain nutrients support overall skin health and may provide protective benefits:
Stress Management 🧘 Chronic stress can affect hormonal balance and immune function, potentially influencing skin health. Implementing stress reduction techniques may support overall skin wellness.
Regular Exercise Benefits 🏃 Physical activity promotes healthy circulation and immune function, supporting the skin's natural repair and maintenance processes.
Pregnancy represents a unique period when hormonal fluctuations significantly impact skin characteristics, including mole development and changes.
Trimester-Specific Changes 🤱
Postpartum Considerations 👶 Many pregnancy-related skin changes, including new moles, persist after delivery. Some may fade gradually as hormone levels normalize, while others remain permanent.
Breastfeeding Impact 🍼 Hormonal changes associated with breastfeeding can continue to influence skin characteristics and mole development for months after delivery.
The hormonal transitions of menopause create another period of increased skin changes and potential mole development.
Perimenopausal Fluctuations 🌊 The irregular hormone levels during perimenopause can trigger various skin changes, including new pigmentation patterns and mole development.
Post-Menopausal Stability 🌸 After menopause, hormonal stability typically reduces the likelihood of hormone-induced mole development, making any new growths more noteworthy.
Understanding normal mole development patterns in children helps parents distinguish between typical growth and concerning changes.
Infant and Toddler Patterns 👶 Most babies are born with few or no moles, with initial mole development typically beginning around age 2-3. Early mole development usually follows predictable patterns and characteristics.
School-Age Development 📚 Children between ages 5-12 often experience steady mole development, with new moles appearing gradually. This period requires balance between monitoring and avoiding excessive concern about normal development.
Adolescent Considerations 🌟 Teenage years bring the most dramatic mole development, with hormonal changes and accumulated sun exposure creating ideal conditions for new mole formation.
For comprehensive information about skin conditions across all age groups, families can reference The Minor Surgery Center's frequently asked questions.
Immunocompromised Individuals 🛡️ People with compromised immune systems may experience different mole development patterns and require more frequent monitoring due to increased skin cancer risks.
Occupational Exposures 🔧 Individuals with jobs requiring significant outdoor exposure or contact with certain chemicals may face elevated risks for mole development and skin changes.
Geographic Considerations 🌍 People living in high-UV environments, such as tropical regions or high altitudes, often experience more frequent mole development throughout their lives.
The process behind what causes moles to suddenly appear involves complex cellular interactions and genetic expressions that scientists continue to study.

Melanocyte Behavior 🧬 Normal melanocytes distribute evenly throughout the skin, producing melanin in response to UV exposure. Mole formation occurs when these cells cluster together, often triggered by genetic signals or environmental factors.
Growth Factor Influences 📈 Various growth factors and cellular signaling pathways influence melanocyte behavior and clustering. Understanding these mechanisms helps explain why moles develop at specific times and locations.
Genetic Expression Changes 🔬 Environmental triggers can activate or suppress specific genes that control melanocyte behavior, leading to sudden mole appearance even in previously unaffected skin areas.
Emerging Technologies 🔍 New diagnostic technologies continue to improve mole evaluation accuracy and early detection capabilities. Artificial intelligence and machine learning applications show promise for enhancing diagnostic precision.
Genetic Testing Applications 🧪 Advanced genetic testing may eventually help predict individual mole development patterns and skin cancer risks, enabling more personalized prevention strategies.
Treatment Innovations 💡 Research into mole removal techniques and prevention strategies continues to evolve, offering improved options for patients with concerning or cosmetically bothersome moles.
Developing effective long-term monitoring strategies helps individuals track their mole development patterns and identify concerning changes early.
Self-Examination Techniques 🪞 Regular self-examinations should follow systematic approaches to ensure comprehensive coverage and consistent monitoring. Monthly self-checks allow individuals to become familiar with their normal mole patterns.
Photography Documentation 📸 Taking periodic photographs of moles can help track subtle changes over time that might otherwise go unnoticed. This documentation proves particularly valuable for individuals with numerous moles.
Professional Assessment Scheduling 📅 Establishing regular dermatological check-up schedules based on individual risk factors ensures appropriate professional monitoring without excessive medical visits.
Mobile Applications 📱 Various smartphone applications now offer mole tracking and monitoring capabilities, though these should supplement rather than replace professional medical evaluation.
Telemedicine Options 💻 Remote dermatological consultations provide accessible options for initial mole assessments, particularly valuable for individuals in underserved geographic areas.
Digital Health Records 💾 Maintaining comprehensive digital records of mole characteristics and changes supports continuity of care and enables better long-term tracking.
While most new moles require only monitoring, certain circumstances warrant removal procedures for medical or cosmetic reasons.
Medical Indications ⚕️
Cosmetic Considerations ✨ Many individuals choose mole removal for aesthetic reasons, particularly when moles appear in visible locations or affect self-confidence.
Preventive Removal 🛡️ Some high-risk individuals may benefit from preventive removal of atypical moles to reduce future cancer risks.
For expert mole evaluation and removal services, patients can consult with the experienced team at The Minor Surgery Center.
Shave Excision ✂️ This technique involves removing the mole at skin level and works well for raised moles without suspicious characteristics.
Punch Biopsy 🕳️ Circular cutting tools remove small, deep tissue samples for diagnostic purposes while minimizing scarring.
Elliptical Excision 🔄 Complete mole removal with surrounding tissue margins ensures thorough removal and provides adequate tissue for comprehensive pathological examination.
Laser Removal ⚡ Certain types of moles may respond to laser treatment, though this approach limits pathological examination capabilities.
The sudden appearance of new moles can create significant anxiety and concern, particularly for individuals with family histories of skin cancer or previous concerning diagnoses.
Anxiety Management 😰 Understanding normal mole development patterns helps reduce unnecessary anxiety while maintaining appropriate vigilance for concerning changes.
Body Image Considerations 🪞 New moles, particularly in visible locations, may affect self-perception and confidence. Open discussions with healthcare providers can address both medical and cosmetic concerns.
Family Communication 👨👩👧👦 Families with genetic predispositions to mole development benefit from open communication about monitoring strategies and medical evaluations.
Community Awareness Programs 📢 Public health initiatives focusing on skin cancer prevention and mole monitoring help educate communities about normal versus concerning skin changes.
School-Based Education 🏫 Teaching children and adolescents about sun protection and skin health establishes lifelong healthy habits during critical developmental periods.
Healthcare Provider Training 👩⚕️ Ongoing education for primary care providers enhances early detection capabilities and appropriate referral patterns for concerning moles.
Scientific understanding of what causes moles to suddenly appear continues to evolve through ongoing research in multiple disciplines.
Genetic Research 🧬 Advanced genetic studies are identifying specific gene variants that influence mole development patterns and skin cancer risks, potentially enabling personalized prevention strategies.
Environmental Health Studies 🌍 Research into environmental factors beyond UV exposure, including pollution and chemical exposures, may reveal additional triggers for mole development.
Hormonal Interaction Studies ⚗️ Detailed investigation of hormonal influences on skin cell behavior may lead to better understanding of mole development timing and prevention opportunities.
Artificial Intelligence Applications 🤖 Machine learning algorithms show promise for improving mole evaluation accuracy and predicting concerning changes before they become visually apparent.
Biomarker Development 🔬 Research into cellular and molecular markers may enable earlier detection of problematic moles and more precise risk assessment.
Preventive Interventions 💊 Future developments may include topical or systemic interventions that can prevent or reduce mole development in high-risk individuals.
Understanding what causes moles to suddenly appear empowers individuals to make informed decisions about their skin health while maintaining appropriate vigilance for concerning changes. The complex interplay of genetic, hormonal, environmental, and age-related factors creates unique risk profiles for each individual, making personalized approaches to monitoring and prevention essential.
The sudden appearance of moles represents a normal biological process for most people, particularly during periods of hormonal change or following significant sun exposure. However, staying informed about warning signs and maintaining regular monitoring routines ensures early detection of any concerning developments.
Key strategies for optimal mole management include:
🔍 Regular self-examinations to become familiar with normal mole patterns ☀️ Comprehensive sun protection to prevent unnecessary UV-induced mole development
👩⚕️ Professional evaluations based on individual risk factors and concerning changes 📚 Ongoing education about normal versus abnormal mole characteristics 🤝 Open communication with healthcare providers about concerns and family history
The field of dermatology continues advancing with new diagnostic technologies and treatment options, offering improved outcomes for individuals with concerning moles or high-risk profiles. By combining scientific understanding with practical prevention strategies, people can maintain healthy skin while addressing new mole development appropriately.
Remember that while most new moles are benign, professional evaluation provides peace of mind and ensures appropriate medical care when needed. The investment in preventive monitoring and sun protection pays dividends in long-term skin health and early detection of any concerning changes.
For comprehensive skin health evaluations and professional mole assessments, individuals are encouraged to consult with qualified dermatologists who can provide personalized recommendations based on individual risk factors and medical history. Taking proactive steps toward skin health today supports lifelong wellness and confidence in managing skin changes as they occur.
For more information about skin conditions, treatment options, and professional consultations, visit The Minor Surgery Center's blog for additional educational resources and expert insights.