Discovering a bump on your scalp can be concerning. While most scalp lumps are harmless, understanding what they are brings peace of mind and helps determine the right course of action. Among the most common scalp growths are cysts—fluid-filled or semi-solid sacs that develop beneath the skin's surface. The types of scalp cysts pilar trichilemmal epidermoid represent the three most frequently diagnosed benign growths on the scalp, each with distinct characteristics, causes, and treatment approaches.
These scalp cysts affect millions of people worldwide, yet many individuals remain unaware of the differences between them. While pilar cysts (also called trichilemmal cysts) and epidermoid cysts may appear similar on the surface, they have unique cellular origins and behaviors that influence how medical professionals diagnose and treat them. This comprehensive guide explores everything needed to understand these common scalp conditions, from their biological foundations to modern treatment options available in 2026.

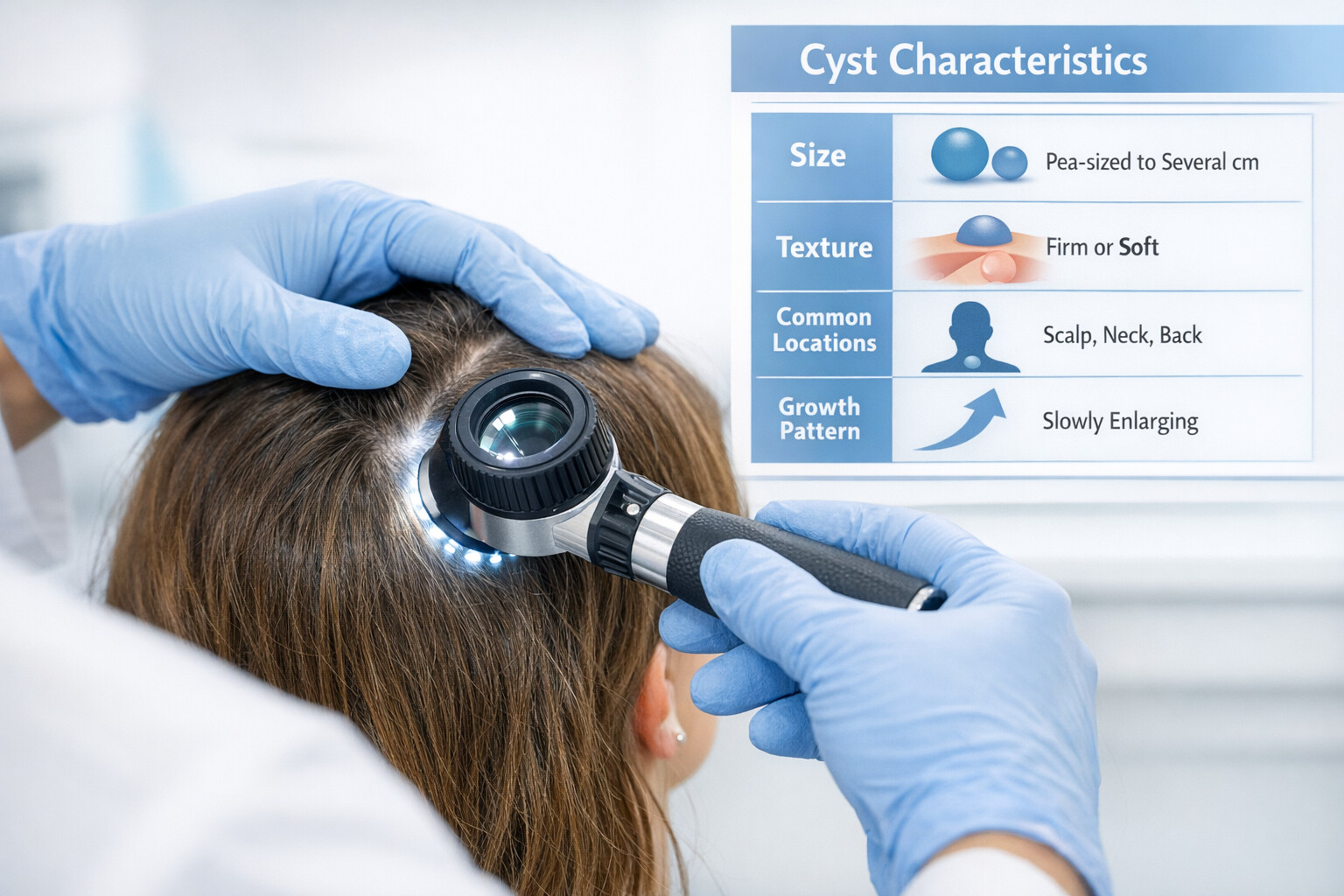
Scalp cysts are closed sac-like structures that develop beneath the skin of the scalp. These growths contain semi-solid material, typically keratin protein, dead skin cells, or other cellular debris. Unlike cancerous tumors, cysts have a distinct wall that separates their contents from surrounding tissue.
The scalp provides an ideal environment for certain types of cysts due to its high concentration of hair follicles and sebaceous glands. These structures can become blocked or damaged, leading to cyst formation. Understanding the types of scalp cysts pilar trichilemmal epidermoid helps distinguish between these common growths and more serious conditions.
Most scalp cysts share several features:
While these characteristics apply broadly, each cyst type has specific features that help medical professionals make accurate diagnoses.
Pilar cysts, also known as trichilemmal cysts or isthmus-catagen cysts, represent the predominant type of cyst found on the scalp. These benign growths account for 5-10% of all cutaneous cysts but comprise approximately 90% of cysts specifically located on the scalp [1].
Pilar cysts originate from the outer root sheath of hair follicles, specifically at the isthmus region where the hair follicle narrows. This anatomical origin explains why they occur almost exclusively on hair-bearing areas, particularly the scalp.
The term "trichilemmal" comes from the Greek words "tricho" (hair) and "lemma" (sheath), directly referencing their hair follicle origin. These cysts contain densely packed keratin that differs from the keratin found in epidermoid cysts. The keratin in pilar cysts undergoes a process called trichilemmal keratinization, which occurs without the granular layer formation seen in normal skin [2].
CharacteristicDescriptionLocation90% occur on the scalp; rarely found elsewhereAppearanceSmooth, firm, mobile lumps under the skinSizeTypically 0.5-5 cm in diameterNumberOften multiple (70% of cases)GenderMore common in women (2:1 ratio)Age of onsetUsually middle-aged adults (40-60 years)InheritanceAutosomal dominant pattern in 50% of cases
The exact trigger for pilar cyst formation remains unclear, but several factors contribute to their development:
✅ Genetic predisposition: Family history significantly increases risk, with inheritance following an autosomal dominant pattern
✅ Hair follicle trauma: Minor injuries to the scalp may damage hair follicle structures
✅ Hormonal factors: Higher prevalence in women suggests hormonal influences
✅ Age-related changes: Hair follicle changes over time may contribute to cyst formation
Patients with pilar cysts typically notice one or more firm, round bumps on their scalp. These growths:
Unlike epidermoid cysts, pilar cysts rarely have a central punctum (visible pore) and typically don't discharge material spontaneously.
The terms "pilar cyst" and "trichilemmal cyst" are completely interchangeable—they refer to the exact same condition. This dual nomenclature sometimes creates confusion, leading people to believe they represent different types of scalp cysts.
Medical terminology evolves over time, and different naming conventions coexist in the literature:
In 2026, dermatologists and pathologists use both terms freely, though "trichilemmal cyst" appears more frequently in pathology reports due to its specificity regarding the keratinization process.
Under microscopic examination, trichilemmal/pilar cysts display distinctive features:
🔬 Cyst wall composition: Stratified squamous epithelium without a granular layer
🔬 Keratin content: Dense, eosinophilic (pink-staining) keratin
🔬 Calcification: Common in long-standing cysts
🔬 Cholesterol clefts: May be present in cyst contents
These histological characteristics allow pathologists to definitively distinguish pilar/trichilemmal cysts from other cyst types, particularly epidermoid cysts.
While epidermoid cysts can occur on the scalp, they differ fundamentally from pilar/trichilemmal cysts in their cellular origin and characteristics. Understanding these differences helps explain why the types of scalp cysts pilar trichilemmal epidermoid require different diagnostic and treatment approaches.
Epidermoid cysts, sometimes incorrectly called "sebaceous cysts," develop from epidermal cells (skin surface cells) rather than hair follicle structures. These cysts form when surface skin cells move deeper into the skin and multiply, creating a sac filled with keratin and lipid material [3].
FeatureEpidermoid CystPilar/Trichilemmal CystOriginEpidermal cellsHair follicle outer root sheathLocationFace, neck, trunk, scalpPredominantly scalp (90%)Central punctumOften presentRarely presentKeratin typeLaminated keratin with granular layerDense keratin without granular layerOdor when rupturedCharacteristic foul smellLess odorousMultiplicityUsually solitaryOften multipleGenetic patternSporadic (except in syndromes)Familial in 50% of cases
Several mechanisms can cause epidermoid cyst development:
💡 Follicular occlusion: Blocked hair follicles trap epidermal cells
💡 Trauma: Injuries that implant surface cells into deeper layers
💡 Surgical implantation: Rare complication of scalp procedures
💡 Developmental anomalies: Congenital inclusion of epidermal cells
Epidermoid cysts on the scalp present as:
When an epidermoid cyst ruptures or becomes infected, it may discharge thick, white, cheese-like material with a distinctly unpleasant odor—a characteristic that helps distinguish it from pilar cysts.
Understanding the types of scalp cysts pilar trichilemmal epidermoid requires recognizing both their similarities and differences. While all three terms describe benign scalp growths, the relationship between them is nuanced.
Think of it this way:
Pilar Cysts = Trichilemmal Cysts (same condition, two names)
Epidermoid Cysts = Different condition that can also occur on the scalp
Experienced dermatologists can often distinguish between these cyst types through physical examination:
Pilar/Trichilemmal Cysts:
Epidermoid Cysts:
Medical professionals use several methods to identify the types of scalp cysts pilar trichilemmal epidermoid:
Most scalp cysts remain asymptomatic for years, causing no discomfort beyond cosmetic concerns. However, certain symptoms warrant medical attention.
While rare, complications can occur with any of the types of scalp cysts pilar trichilemmal epidermoid:
⚠️ Infection: Bacterial invasion causing redness, warmth, pain, and pus formation
⚠️ Inflammation: Cyst rupture into surrounding tissue triggering immune response
⚠️ Rapid growth: Sudden enlargement may indicate inflammation or rare malignant transformation
⚠️ Rupture: Spontaneous or trauma-induced breaking of the cyst wall
⚠️ Calcification: Long-standing cysts may develop calcium deposits
⚠️ Proliferating trichilemmal cyst: Rare variant with aggressive local growth (0.1% of pilar cysts)
Malignant transformation of benign scalp cysts is extremely rare but documented in medical literature. Proliferating trichilemmal tumors represent a low-grade malignant variant that can develop from long-standing pilar cysts, occurring in less than 0.1% of cases [4].
Warning signs include:
Any of these changes warrant immediate medical evaluation.
Accurate diagnosis of the types of scalp cysts pilar trichilemmal epidermoid ensures appropriate treatment and rules out more serious conditions.
The diagnostic process typically begins with:
Visual inspection: Assessing size, color, and surface characteristics
Palpation: Evaluating texture, mobility, and tenderness
Medical history: Family history, duration, and symptom progression
Dermatoscopy: Magnified examination of surface features
When clinical examination is inconclusive, imaging provides additional information:
Ultrasound: First-line imaging showing cyst structure, wall thickness, and internal echogenicity
MRI: Reserved for complex cases or suspected deep extension
CT scan: Useful when calcification is present or bone involvement suspected
Definitive diagnosis requires microscopic examination:
Pathologists examine the keratinization pattern, cyst wall structure, and cellular composition to distinguish between pilar/trichilemmal and epidermoid cysts definitively.
Treatment approaches for the types of scalp cysts pilar trichilemmal epidermoid range from conservative observation to surgical removal, depending on several factors.
Observation is appropriate when:
Treatment is recommended when:
While surgical removal is the only definitive cure, some approaches may help manage symptoms:
Intralesional corticosteroid injection: Reduces inflammation in inflamed cysts
Antibiotics: Treats secondary bacterial infection
Warm compresses: Provides symptomatic relief during inflammation
Drainage: Temporary measure for infected cysts (high recurrence rate)
Complete surgical excision remains the most effective treatment for the types of scalp cysts pilar trichilemmal epidermoid, offering the lowest recurrence rates.
This modern approach minimizes scarring:
Advantages:
For larger or complicated cysts:
Advantages:
CO2 laser and erbium laser techniques offer alternatives for select cases:
Recurrence depends on treatment method:
Treatment MethodRecurrence RateComplete excision with intact wall1-3%Minimal excision5-10%Simple drainage80-100%Laser ablation10-20%
While genetic factors in pilar cyst development cannot be modified, certain strategies may reduce risk or complications:
✓ Gentle scalp care: Avoid aggressive brushing or trauma
✓ Prompt treatment of scalp conditions: Address folliculitis or dermatitis early
✓ Sun protection: Prevents skin damage that may contribute to cyst formation
✓ Avoid squeezing or manipulating cysts: Reduces infection and inflammation risk
✓ Regular scalp examination: Early detection of changes
For families with multiple affected members:
For individuals choosing observation over immediate treatment, several practical tips enhance quality of life:
Keep track of:
📝 Size changes: Measure periodically with a ruler
📝 Symptom development: Note any pain, redness, or drainage
📝 Growth rate: Sudden changes warrant medical evaluation
📝 Number of cysts: New lesions may indicate familial pattern
Contact a healthcare provider if:
Certain groups require special consideration regarding the types of scalp cysts pilar trichilemmal epidermoid.
Scalp cysts are less common in children but can occur:
Pregnancy considerations include:
Individuals with weakened immune systems face higher risks:
Medical science continues advancing understanding and management of scalp cysts.
High-resolution ultrasound: Improved imaging distinguishes cyst types non-invasively
Artificial intelligence: Machine learning algorithms assist in image interpretation
Optical coherence tomography: Emerging technology for real-time tissue imaging
Molecular markers: Research identifying genetic signatures of different cyst types
Minimally invasive techniques: Continued refinement of small-incision methods
Laser technology: New wavelengths and protocols improving outcomes
Tissue adhesives: Reducing need for sutures in select cases
Scar reduction protocols: Advanced wound care minimizing visible scarring
Current research focuses on:
The vast majority of scalp cysts are completely benign. Malignant transformation is extremely rare (less than 0.1% of cases) but can occur in long-standing pilar cysts. Any rapidly growing or changing cyst should be evaluated by a healthcare professional.
No—attempting to pop or squeeze scalp cysts is strongly discouraged. This can:
Scalp cysts rarely resolve spontaneously. While they may remain stable for years, the cyst wall persists unless surgically removed. Observation is appropriate for asymptomatic cysts, but spontaneous resolution should not be expected.
Signs of infection include:
Surgical removal is performed under local anesthesia, making the procedure virtually painless. Post-operative discomfort is typically mild and well-controlled with over-the-counter pain medication. Most patients report minimal pain during recovery.
While this guide provides comprehensive information about the types of scalp cysts pilar trichilemmal epidermoid, it cannot replace professional medical evaluation. Self-diagnosis carries risks, as other scalp conditions may mimic cysts:
Lipomas: Fatty tumors that feel soft and mobile
Dermoid cysts: Congenital cysts containing multiple tissue types
Abscesses: Infected collections of pus
Seborrheic keratoses: Benign skin growths
Skin cancer: Basal cell carcinoma, squamous cell carcinoma, or melanoma
Metastatic lesions: Rare spread of cancer from other sites
Only qualified healthcare professionals can accurately diagnose scalp lesions through examination and, when necessary, biopsy.
Understanding the financial aspects of scalp cyst treatment helps patients make informed decisions.
Initial consultation: $150-$300
Imaging (if needed): $200-$500
Surgical excision: $500-$2,500 depending on complexity
Pathology examination: $150-$400
Follow-up visits: $100-$200
Most insurance plans cover scalp cyst removal when:
Cosmetic removal of asymptomatic cysts may not be covered, requiring out-of-pocket payment.
Before proceeding with treatment:
✅ Is scalp cyst removal covered under my plan?
✅ What documentation is required for coverage?
✅ What is my deductible and co-pay?
✅ Are there preferred providers I should use?
✅ Is pre-authorization required?
Selecting an experienced provider ensures optimal outcomes for scalp cyst management.
Dermatologists: Skin specialists with extensive cyst experience
Plastic surgeons: Expertise in cosmetic outcomes and complex cases
General surgeons: Can perform excisions, especially for larger cysts
Family physicians: May handle simple cases or provide referrals
When consulting about the types of scalp cysts pilar trichilemmal epidermoid:
Seek a second opinion if a provider:
Proper post-operative care optimizes healing and minimizes complications.
Wound care:
Activity restrictions:
Pain management:
Wound monitoring:
Hair care:
Activity resumption:
Suture removal:
Scar management:
Follow-up:
While medically benign, scalp cysts can affect emotional well-being and quality of life.
Body image issues: Visible bumps affecting self-perception
Social anxiety: Worry about others noticing cysts
Fear of cancer: Despite reassurance, some anxiety persists
Frustration with recurrence: Emotional toll of repeated cysts
Decision-making stress: Uncertainty about treatment choices
💚 Education: Understanding the benign nature reduces anxiety
💚 Support groups: Connecting with others who have similar experiences
💚 Professional counseling: For significant distress
💚 Practical solutions: Hairstyling adaptations while deciding on treatment
💚 Proactive management: Taking control through informed decisions
Scalp cyst prevalence and management vary across populations and cultures.
Research indicates some differences in scalp cyst occurrence:
Access to diagnosis and treatment varies worldwide:
Developed countries: Advanced imaging and surgical techniques readily available
Developing regions: Limited access to specialists and surgical facilities
Traditional medicine: Some cultures prefer alternative approaches
Cost barriers: Significant factor in treatment decisions globally
The types of scalp cysts pilar trichilemmal epidermoid represent common, typically benign growths that affect millions of people worldwide. Understanding that pilar and trichilemmal cysts are the same condition—accounting for the vast majority of scalp cysts—while epidermoid cysts represent a different entity that can also occur on the scalp, provides clarity in an often confusing topic.
🎯 Most scalp cysts are harmless and require treatment only if symptomatic or cosmetically concerning
🎯 Accurate diagnosis distinguishes between cyst types and rules out other conditions
🎯 Multiple treatment options exist, from observation to surgical removal
🎯 Complete excision offers the lowest recurrence rates and definitive treatment
🎯 Professional evaluation is essential for any scalp growth, especially those that change rapidly
If you've discovered a scalp cyst or want to address an existing one:
Step 1: Schedule an evaluation with a dermatologist or qualified healthcare provider
Step 2: Discuss your symptoms, concerns, and family history thoroughly
Step 3: Understand your diagnosis and all available treatment options
Step 4: Make an informed decision based on your individual circumstances
Step 5: Follow through with chosen treatment and aftercare recommendations
Step 6: Monitor for any changes and maintain regular follow-up as recommended
Understanding the types of scalp cysts pilar trichilemmal epidermoid empowers individuals to:
While scalp cysts may seem concerning when first discovered, the vast majority are completely benign conditions with excellent treatment outcomes. Armed with knowledge about these common growths, individuals can approach their healthcare with confidence and achieve optimal results.
Remember that every scalp cyst is unique, and individualized medical advice from a qualified healthcare professional should guide all treatment decisions. This comprehensive guide serves as an educational resource, but cannot replace the personalized care that comes from a thorough medical evaluation.
[1] Satyaprakash AK, Sheehan DJ, Sangueza OP. Proliferating trichilemmal tumors: a review of the literature. Dermatol Surg. 2007;33(9):1102-1108.
[2] Brownstein MH, Arluk DJ. Proliferating trichilemmal cyst: a simulant of squamous cell carcinoma. Cancer. 1981;48(4):1207-1214.
[3] Zuber TJ. Minimal excision technique for epidermoid (sebaceous) cysts. Am Fam Physician. 2002;65(7):1409-1412.
[4] Ye J, Nappi O, Swanson PE, Patterson JW, Wick MR. Proliferating pilar tumors: a clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J Clin Pathol. 2004;122(4):566-574.