Imagine waking up one morning and struggling to button your shirt, grip your coffee mug, or turn a doorknob—simple tasks you've done thousands of times without a second thought. For millions living with hand osteoarthritis (OA), this isn't just a bad day; it's everyday life. The aching, stiffness, and swelling in your fingers and thumbs can steal your independence and leave you searching for relief that actually works.
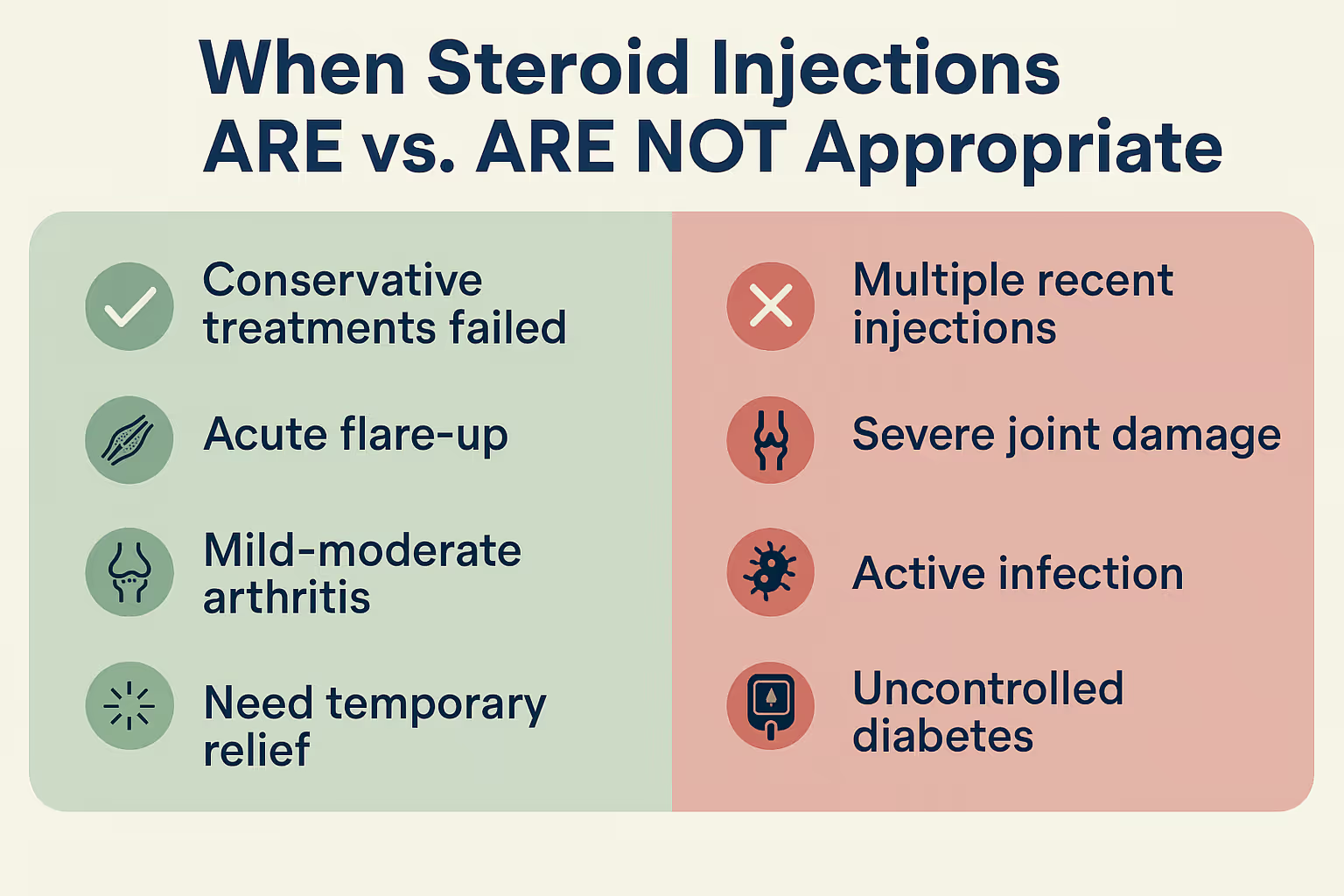
When over-the-counter pain relievers and hand exercises aren't cutting it anymore, you might wonder: Are steroid injections the answer? They're one of the most common treatments doctors recommend for hand OA, but they're not right for everyone or every situation. Understanding when these injections make sense—and when they don't—can help you make informed decisions about your care and get back to doing the things you love.
Steroid injections for hand osteoarthritis involve injecting corticosteroids—powerful anti-inflammatory medications—directly into the affected joint. Think of it as delivering medicine right to the source of your pain, rather than taking a pill that has to travel through your entire body first.
When you have hand OA, the protective cartilage cushioning your joints breaks down over time. Your body responds to this damage with inflammation—swelling, warmth, and pain that can make even gentle movements uncomfortable. Corticosteroids work by:
The most commonly used corticosteroids for hand injections include triamcinolone, methylprednisolone, and betamethasone. Your doctor might also mix the steroid with a local anesthetic like lidocaine to provide immediate numbing relief while the steroid takes effect over the following days.
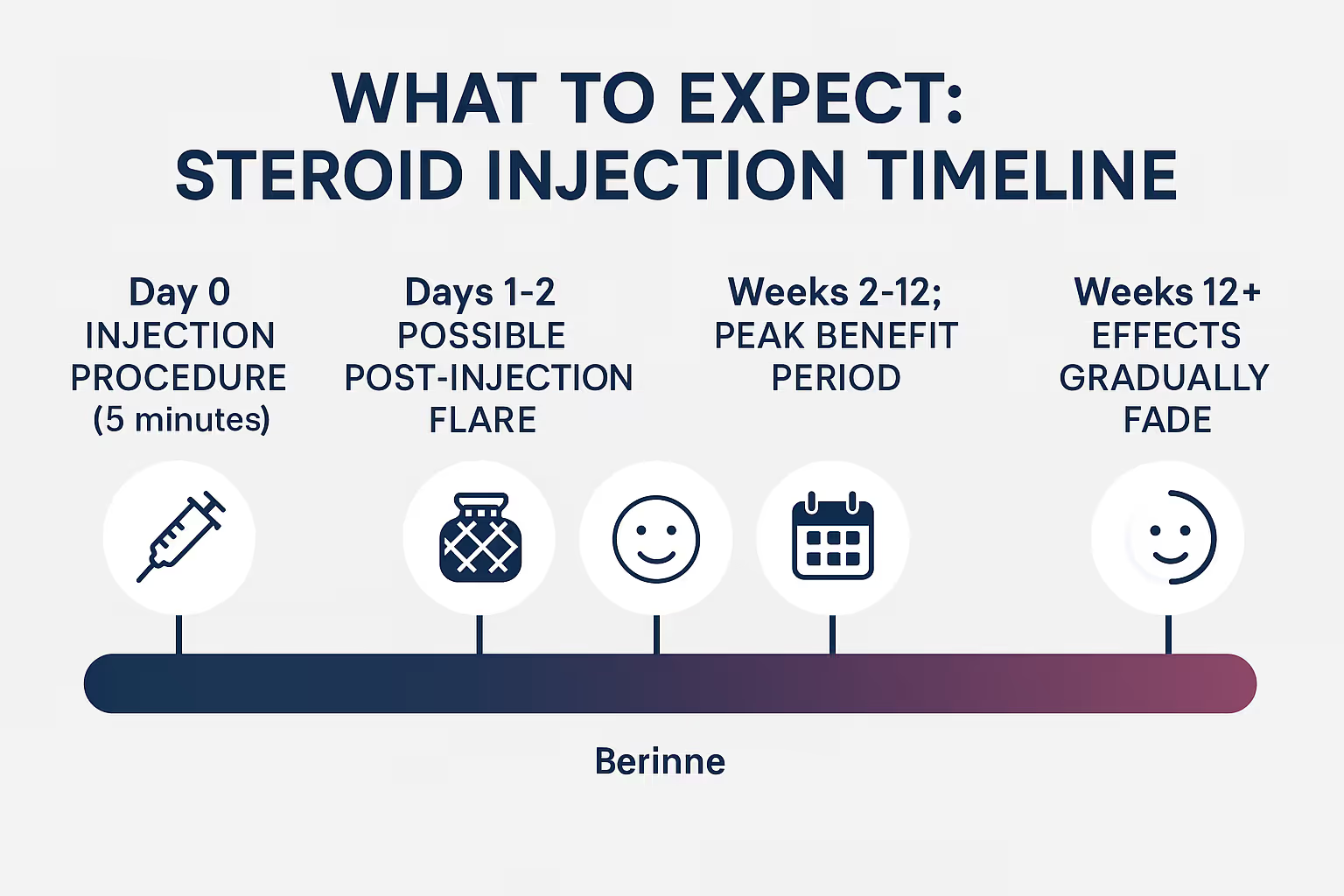
If you've never had a joint injection before, you might be nervous—and that's completely normal. Here's what typically happens:
Most patients describe the sensation as a brief pinch followed by pressure as the medication enters the joint. The entire process usually takes less than five minutes, and you can go home immediately afterward.
Not all hand joints are created equal when it comes to steroid injections. Hand OA typically affects three main areas, and each responds differently to treatment.
The carpometacarpal (CMC) joint at the base of your thumb is the most common site of hand OA. This joint allows the unique range of motion that makes human hands so versatile—but all that movement comes at a cost. The CMC joint bears tremendous force during gripping and pinching activities.
Why steroid injections work well here:
The distal interphalangeal (DIP) joints are closest to your fingertips, while the proximal interphalangeal (PIP) joints are the middle knuckles. These smaller joints can develop painful bony enlargements called Heberden's nodes (DIPs) and Bouchard's nodes (PIPs).
Injection considerations for finger joints:
The metacarpophalangeal (MCP) joints—your main knuckles—are less commonly affected by osteoarthritis (they're more often involved in rheumatoid arthritis). When OA does occur here, steroid injections can be effective, though this presentation is relatively rare.

Knowing whether steroid injections are right for you depends on several factors. Let's explore the situations where they make the most sense.
Steroid injections aren't typically the first line of defense against hand OA. They're most appropriate when you've already tried:
If you've given these conservative approaches a fair trial—usually 3-6 months—without sufficient improvement, it's reasonable to discuss injections with your healthcare provider.
Hand OA isn't always consistent. You might have periods where symptoms are manageable, followed by sudden flare-ups with increased pain, swelling, and stiffness. These acute episodes are ideal candidates for steroid injections because:
Think of it like using a fire extinguisher on a small fire before it spreads—you're intervening at the right moment to prevent bigger problems.
Life doesn't stop because you have arthritis. Maybe you're:
Steroid injections can provide a strategic window of relief—typically 6-12 weeks—allowing you to participate fully in important life events. This isn't about masking symptoms indefinitely; it's about thoughtfully timing treatment to align with your life needs.
X-rays and other imaging can help determine whether steroid injections are likely to help. The ideal candidate shows:
If imaging shows severe end-stage arthritis with bone-on-bone contact, complete cartilage loss, and significant deformity, steroid injections are less likely to provide meaningful relief. At that point, surgical options might be more appropriate.
For some patients, steroid injections serve as a bridge treatment—buying time before more invasive interventions become necessary. This approach makes sense when:
While injections won't cure the underlying arthritis or permanently halt its progression, they can extend the period where you maintain acceptable function without surgical intervention.
Just as important as knowing when injections can help is understanding when they're not the right choice.
Frequency matters. Most experts recommend limiting steroid injections to no more than 3-4 times per year in any single joint. Here's why:
Number of InjectionsPotential Concerns1-2 per yearGenerally safe; minimal risk of adverse effects3-4 per yearApproaching the upper limit; careful monitoring needed5+ per yearIncreased risk of cartilage damage, tendon weakening, and bone loss
Repeated steroid exposure can actually accelerate cartilage breakdown—the opposite of what you're trying to achieve. If you find yourself needing injections more frequently, it's time to reassess your overall treatment strategy.
Injecting steroids into or near an infected area can be dangerous. Corticosteroids suppress your immune system locally, which could allow an infection to spread rapidly. Your doctor will check for signs of infection before proceeding, including:
If there's any concern about infection, treatment focuses on addressing that first before considering injections.
Steroid injections can cause temporary spikes in blood sugar levels, which can last several days to weeks. If you have diabetes—especially if it's poorly controlled—this poses additional risks. You're not necessarily ruled out from receiving injections, but you'll need:
When X-rays reveal advanced arthritis with complete joint space loss, significant bone spurs, and severe deformity, steroid injections rarely provide meaningful or lasting relief. At this stage, you're dealing with mechanical problems—bone rubbing on bone—rather than primarily inflammatory issues.
Think of it this way: if your car's brake pads are completely worn down to metal-on-metal contact, adding brake fluid won't solve the problem. Similarly, anti-inflammatory medication can't cushion bones that have lost their protective cartilage.
Though rare, some people have allergies or sensitivities to corticosteroids or the preservatives and carriers used in injectable formulations. Always inform your doctor about:
Managing expectations is crucial for satisfaction with any medical treatment. Let's be honest about what steroid injections can and can't do.
Research shows that 60-80% of patients with hand OA experience meaningful pain reduction after steroid injections, particularly in the CMC joint. You might notice:
The relief typically begins within 3-7 days as the steroid takes effect, though some people notice improvement sooner, especially if local anesthetic was included.
Here's what the research tells us about duration:
Steroid injections are a symptom management tool, not a cure. They don't reverse cartilage damage, regrow tissue, or stop arthritis progression. They simply calm inflammation and provide a window of improved function.
Your response to steroid injections depends on multiple factors:
Factors associated with better outcomes:
Factors associated with poorer outcomes:
Like any medical procedure, steroid injections come with potential risks. Understanding these helps you make informed decisions and recognize problems if they occur.
Post-injection flare (10-15% of patients):
Skin changes at injection site:
Facial flushing:
Temporary blood sugar elevation:
Infection (rare, less than 1 in 1,000):
Tendon weakening or rupture (very rare):
Nerve damage (extremely rare):
Cartilage damage (with repeated injections):
You can reduce the likelihood of complications by:
If you're considering steroid injections and want to discuss your specific situation with experienced healthcare professionals, the team at The Minor Surgery Center can help you understand your options.
Steroid injections work best as part of a comprehensive treatment plan, not as a standalone solution. Think of managing hand OA like tending a garden—you need multiple approaches working together for the best results.
After a steroid injection provides relief, that's your golden window to:
The injection reduces pain and inflammation, making therapy more effective and tolerable. The therapy, in turn, helps maintain and extend the benefits you gained from the injection.
Custom or over-the-counter splints can:
For CMC arthritis, a thumb spica splint worn at night or during aggravating activities can significantly extend the relief from injections.
Small changes in how you do things can make a big difference:
Steroid injections complement rather than replace other medications:
Some patients find additional relief from:
While evidence varies for these approaches, they're generally safe and may provide complementary benefits when combined with conventional treatments.
Proper preparation can improve your experience and outcomes.
Questions to ask your doctor:
What to bring:
What to avoid:
First 24-48 hours:
First week:
Ongoing:
Steroid injections aren't your only option. Depending on your situation, alternatives might include:
Also called viscosupplementation, these injections use a gel-like substance that mimics natural joint fluid. While commonly used for knee OA, research on hand OA is limited. Potential benefits include:
However, they're less well-studied for hand joints, may not be covered by insurance, and are generally more expensive than steroid injections.
PRP involves injecting concentrated platelets from your own blood into the affected joint. The theory is that growth factors in platelets may promote healing. Current evidence for hand OA is:
Some studies suggest PRP might provide longer-lasting relief than steroids with potentially fewer side effects, but more research is needed.
This procedure uses heat to interrupt pain signals from nerves around the affected joint. It's:
When conservative treatments including injections no longer provide adequate relief, surgery might be appropriate:
For CMC arthritis:
For finger joint arthritis:
Surgery is typically reserved for severe cases where quality of life is significantly impacted despite comprehensive non-surgical management. You can learn more about surgical and procedural options available for various hand conditions.
Theory is one thing; real life is another. Here are practical considerations when deciding about steroid injections.
Steroid injections are generally well-covered by insurance for medically appropriate indications. Typical costs:
Compare this to:
One of the biggest advantages of steroid injections is efficiency:
This makes them practical for busy people who need relief without extensive time off work or major lifestyle disruption.
Some people are comfortable with:
Others prefer to:
Neither approach is wrong—it's about what aligns with your values, goals, and comfort level.
Consider what you're hoping to achieve:
Injections might be ideal if you want to:
Other approaches might be better if you're seeking:
Having a productive conversation with your doctor helps ensure steroid injections are right for you. Consider asking:
Don't hesitate to ask for clarification if you don't understand something. A good healthcare provider welcomes questions and wants you to feel informed and comfortable with your treatment decisions.
If you'd like to discuss your hand concerns with experienced professionals who prioritize clear communication and patient comfort, consider reaching out to our team at The Minor Surgery Center.

Steroid injections are just one tool in managing hand osteoarthritis. The most successful approach involves accepting the chronic nature of the condition while actively managing it.
Effective hand OA management often involves:
The field of arthritis treatment continues to evolve. Stay current by:
While you can't control whether you develop arthritis or how quickly it progresses, you can control:
Living with hand OA means appreciating improvements, even if they're temporary or partial:
These victories matter, whether they come from steroid injections, hand therapy, adaptive equipment, or a combination of approaches.
How painful is the injection itself?
Most people describe it as a brief pinch followed by pressure. The discomfort typically lasts only a few seconds. Many doctors use a very thin needle and may include local anesthetic with the steroid, which provides immediate numbing. Some patients report that the anticipation is worse than the actual injection.
Can I use my hand normally after the injection?
You should rest your hand for the first 24-48 hours, avoiding strenuous activities, heavy gripping, and repetitive motions. After that, gradually resume normal activities as comfort allows. Most people return to regular use within a few days.
Will I need to take time off work?
Most people don't need time off work for the injection itself. However, if your job involves heavy hand use, you might want to schedule the injection before a weekend or lighter work period to allow for initial rest.
How quickly will I feel relief?
If your doctor included local anesthetic, you might feel immediate numbing that lasts a few hours. The steroid itself typically takes 3-7 days to reach full effect, though some people notice improvement sooner.
What if the injection doesn't help?
If you experience no improvement after 2-3 weeks, the injection likely didn't work for you. This information is still valuable—it helps your doctor refine your diagnosis and consider alternative treatments. Don't give up; there are many other options to explore.
Can steroid injections cure my arthritis?
No. Steroid injections provide symptom relief but don't cure arthritis, reverse cartilage damage, or stop disease progression. They're a management tool, not a cure.
Are steroid injections addictive?
No. Corticosteroids used for joint injections are not addictive. However, some people become psychologically dependent on the relief they provide and want injections more frequently than is medically appropriate. This is why doctors limit injection frequency.
Can I get injections in multiple joints at the same time?
This depends on your overall health and the total steroid dose. Some doctors prefer to inject one or two joints per visit to minimize systemic steroid exposure. Discuss your specific situation with your provider.
For more answers to common questions about procedures and treatments, visit our FAQs page.
If you're struggling with hand osteoarthritis and wondering whether steroid injections might help, you don't have to figure it out alone.
At The Minor Surgery Center, we understand that dealing with hand pain affects every aspect of your life. While our primary focus is on minor surgical procedures for conditions like moles, cysts, and lipomas, we believe in connecting patients with appropriate care for all their concerns.
If you have questions about hand conditions or need guidance on finding the right specialist, we're happy to point you in the right direction. You can contact us or learn more about our approach to patient care.
Steroid injections for hand osteoarthritis can be a valuable tool when used appropriately. They're most suitable when conservative treatments haven't provided adequate relief, when you're experiencing an acute flare-up, when you need temporary symptom control for a specific purpose, or when you're working to delay more invasive interventions.
The key to successful outcomes is realistic expectations. Steroid injections won't cure your arthritis or provide permanent relief, but they can offer a significant window of reduced pain and improved function—typically 6-12 weeks—that allows you to engage more fully in life and other therapeutic activities.
They work best as part of a comprehensive approach that includes hand therapy, joint protection, appropriate exercise, lifestyle modifications, and ongoing medical management. The decision to pursue injections should be made collaboratively with your healthcare provider, considering your specific joint involvement, overall health, treatment goals, and personal preferences.
Remember that managing hand OA is a journey, not a destination. There will be good days and challenging days. The goal isn't perfection—it's finding the combination of strategies that allows you to maintain the function and quality of life that matters most to you.
Whether steroid injections become part of your treatment plan or not, staying informed, proactive, and engaged in your care gives you the best chance of living well despite arthritis. You deserve to feel confident in your hands and the activities they allow you to do. With the right approach and support, that's entirely possible.