Imagine discovering a suspicious spot on your skin that turns out to be melanoma – but catching it at the absolute earliest stage possible. This scenario, while initially frightening, actually represents one of the best possible outcomes when dealing with skin cancer. Stage 0 melanoma offers patients an incredibly hopeful prognosis, but understanding what it means and how to handle it can feel overwhelming.
When doctors diagnose stage 0 melanoma, they're identifying cancer cells that haven't yet spread beyond the outermost layer of skin. This early detection represents a crucial window of opportunity where treatment is most effective and outcomes are exceptionally positive. However, many people don't fully understand what this diagnosis means or what steps they should take next.
The journey from discovery to treatment doesn't have to be confusing or scary. With the right information and proper medical care, patients can navigate this diagnosis with confidence and achieve excellent results.
• Stage 0 melanoma (melanoma in situ) is confined to the epidermis and hasn't spread deeper into the skin
• The survival rate for stage 0 melanoma approaches nearly 100% with proper treatment
• Early detection through regular skin checks significantly improves treatment outcomes
• Surgical removal is typically the primary and most effective treatment option
• Prevention strategies and ongoing monitoring remain crucial even after successful treatment
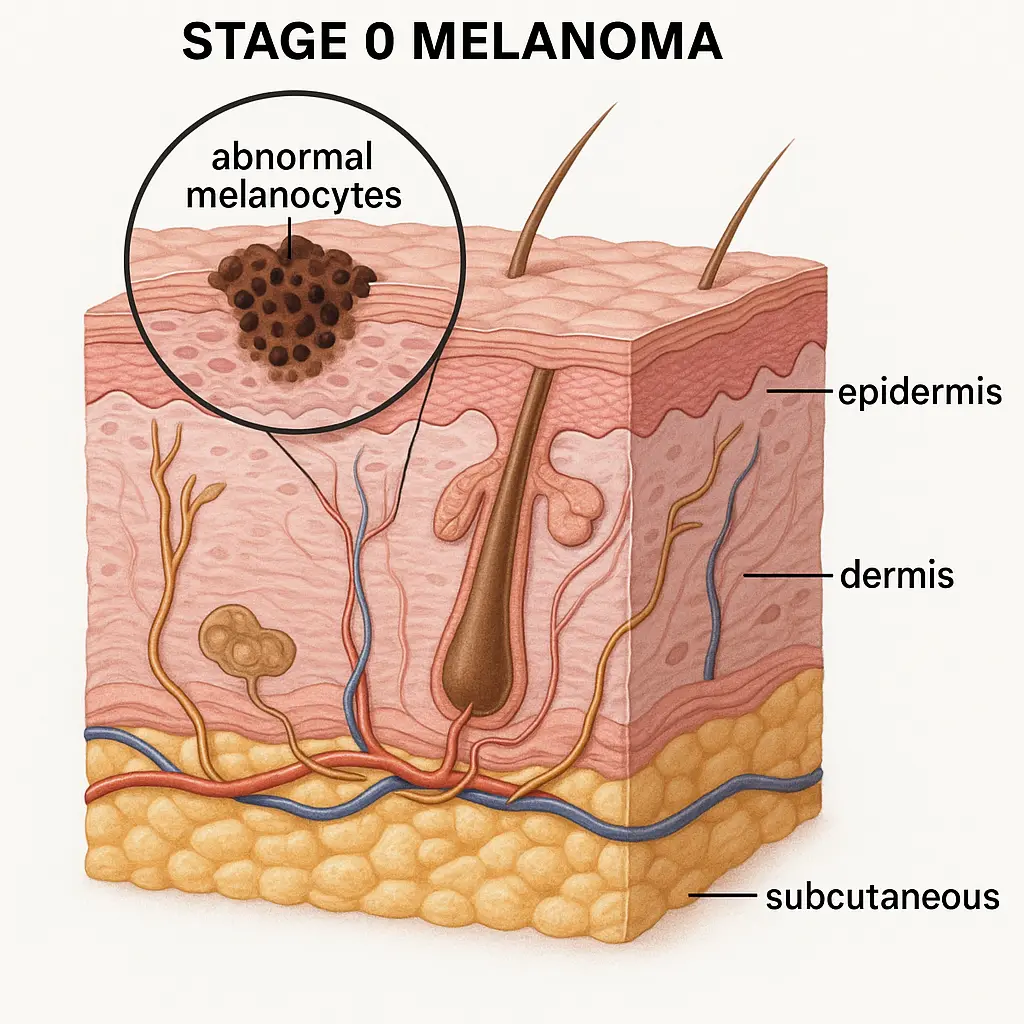
Stage 0 melanoma, also known as melanoma in situ, represents the earliest possible stage of melanoma diagnosis. The term "in situ" literally means "in place," indicating that abnormal melanocytes (pigment-producing cells) remain confined to the epidermis – the outermost layer of skin.
Unlike more advanced stages of melanoma, stage 0 melanoma hasn't penetrated the basement membrane that separates the epidermis from the deeper dermis layer. This containment is what makes stage 0 melanoma so treatable and why the prognosis remains excellent.
At the cellular level, stage 0 melanoma involves melanocytes that have undergone genetic changes causing them to grow abnormally. However, these cells haven't yet developed the ability to invade surrounding tissues or spread to other parts of the body. They remain clustered within the epidermis, making them accessible for complete removal.
The melanocytes in stage 0 melanoma may appear larger than normal, have irregular shapes, or show increased pigmentation. These changes are visible under microscopic examination, which is why a biopsy is essential for proper diagnosis.
Understanding the staging system helps patients grasp why stage 0 melanoma carries such a positive outlook. The melanoma staging system ranges from 0 to IV, with each stage representing increasing levels of cancer spread and complexity.
Stage 0: Cancer cells remain in the epidermis only Stage I: Melanoma has grown into the dermis but remains localized Stage II: Thicker melanoma with possible ulceration, still localized Stage III: Cancer has spread to nearby lymph nodes or skin Stage IV: Cancer has spread to distant organs or lymph nodes
The key difference lies in invasion and spread. While stage 0 melanoma stays put in the epidermis, higher stages involve progressively deeper invasion and wider spread throughout the body.
Stage 0 melanoma often appears as changes in existing moles or new growths on the skin. The famous ABCDE criteria provide an excellent framework for identifying suspicious changes:
🔍 A - Asymmetry: One half doesn't match the other half 🔍 B - Border: Edges are irregular, ragged, or blurred 🔍 C - Color: Multiple colors or uneven color distribution 🔍 D - Diameter: Larger than 6mm (about the size of a pencil eraser) 🔍 E - Evolving: Changes in size, shape, color, or texture
Beyond the ABCDE criteria, other symptoms may include:
It's important to note that stage 0 melanoma may not cause any physical symptoms like pain or itching. Many cases are discovered during routine skin examinations, highlighting the importance of regular check-ups.
Diagnosing stage 0 melanoma involves several steps, each designed to confirm the presence of cancer cells and determine their exact location and extent.
The diagnostic journey typically begins with a visual examination by a dermatologist or healthcare provider. They'll assess suspicious areas using specialized tools like dermatoscopes, which provide magnified views of skin structures.
When a suspicious lesion is identified, a biopsy becomes necessary. Several biopsy types may be used:
Excisional Biopsy: Removes the entire suspicious area Incisional Biopsy: Removes a portion of the suspicious area Punch Biopsy: Uses a circular tool to remove a small cylinder of tissue Shave Biopsy: Removes the surface layers of skin
For suspected melanoma, excisional biopsy is often preferred when possible, as it provides the most complete tissue sample for analysis.
Once tissue is obtained, pathologists examine it under microscopes to identify cancer cells and determine their characteristics. They'll look for:
This analysis confirms whether the diagnosis is stage 0 melanoma and provides information crucial for treatment planning.
The primary treatment for stage 0 melanoma focuses on complete surgical removal of the abnormal tissue. Since the cancer cells haven't spread beyond the epidermis, surgical intervention typically provides a cure.
Wide local excision represents the gold standard treatment for stage 0 melanoma. This procedure involves:
The surgeon will send the removed tissue for pathological examination to confirm that all cancer cells have been eliminated. Clear margins indicate successful removal.
In certain cases, particularly when the melanoma is located in cosmetically sensitive areas like the face, Mohs surgery may be recommended. This specialized technique:
After surgical removal of stage 0 melanoma, proper wound care becomes essential. Patients typically need to:
Most surgical sites heal completely within 2-4 weeks, depending on the location and size of the excision.
The prognosis for stage 0 melanoma is exceptionally positive. When properly treated, the survival rate approaches nearly 100%. This excellent outcome reflects the fact that cancer cells haven't had the opportunity to spread to other parts of the body.
Several factors influence the outlook for stage 0 melanoma patients:
Complete surgical removal: Achieving clear margins during surgery is crucial Location: Some body areas may have slightly different recurrence risks Patient compliance: Following up with regular skin checks affects long-term outcomes Sun protection: Preventing future skin damage reduces the risk of new melanomas
Patients successfully treated for stage 0 melanoma can expect:
The key to maintaining this positive outlook lies in ongoing vigilance and proper skin care practices.
Even after successful treatment of stage 0 melanoma, prevention strategies remain crucial for avoiding future skin cancers. Understanding and implementing protective measures can significantly reduce the risk of developing additional melanomas.
🌞 Daily Sunscreen Use: Apply broad-spectrum SPF 30+ sunscreen every day, even on cloudy days
🌞 Protective Clothing: Wear long-sleeved shirts, wide-brimmed hats, and UV-blocking sunglasses
🌞 Seek Shade: Avoid direct sun exposure during peak hours (10 AM to 4 PM)
🌞 Avoid Tanning Beds: Eliminate artificial UV exposure completely
Beyond sun protection, other lifestyle changes can help reduce melanoma risk:
Being aware of environmental factors that increase UV exposure helps with prevention:
After treatment for stage 0 melanoma, establishing a comprehensive follow-up care plan becomes essential. Regular monitoring helps detect any recurrence early and identifies new skin changes that might require attention.
Schedule Regular Check-ups: Most patients need dermatological examinations every 3-6 months initially Full-Body Skin Mapping: Some providers use photography to track changes over time Lymph Node Checks: Although unlikely with stage 0, providers may examine nearby lymph nodes Documentation: Keeping records of all moles and skin changes helps track patterns
Patients play a crucial role in ongoing monitoring through monthly self-examinations:
🔍 Use Good Lighting: Examine skin in bright, natural light when possible 🔍 Use Mirrors: Check hard-to-see areas with handheld and full-length mirrors 🔍 Be Systematic: Develop a routine that covers every area of the body 🔍 Document Changes: Take photos of suspicious areas for comparison 🔍 Know Your Skin: Become familiar with your normal mole patterns
Patients should contact their healthcare team if they notice:
Early communication with healthcare providers ensures prompt evaluation of concerning changes.
Receiving a stage 0 melanoma diagnosis can trigger various emotional responses, even though the prognosis is excellent. Understanding how to cope with the diagnosis and move forward positively is an important part of the healing process.
Common emotional reactions to a stage 0 melanoma diagnosis include:
Initial Shock: Even with a good prognosis, cancer diagnosis can be overwhelming Anxiety: Worry about recurrence or developing other skin cancers Relief: Learning that the cancer was caught very early Motivation: Increased commitment to prevention and health maintenance
Several approaches can help patients manage the emotional aspects of their diagnosis:
Education: Learning about stage 0 melanoma reduces fear and anxiety Support Systems: Connecting with family, friends, or support groups Professional Counseling: Speaking with counselors experienced in cancer care Mindfulness Practices: Meditation, yoga, or other stress-reduction techniques
Patients can develop resilience by:
Stage 0 melanoma can affect people of all ages, but certain considerations apply to different age groups that influence treatment approaches and follow-up care.
Young people diagnosed with stage 0 melanoma face unique challenges:
Genetic Factors: Early onset may indicate inherited risk factors Lifestyle Education: Learning sun protection habits early is crucial Long-Term Monitoring: Decades of follow-up care will be needed Family Planning: Understanding hereditary risks for future children
Adults in their 30s-50s often deal with:
Work Considerations: Managing treatment around career responsibilities Family Responsibilities: Balancing personal care with family needs Insurance Planning: Ensuring adequate coverage for ongoing monitoring Prevention Education: Teaching family members about sun safety
Seniors with stage 0 melanoma may face:
Multiple Health Conditions: Coordinating care with other medical issues Medication Interactions: Considering how treatments affect other medications Mobility Concerns: Adapting self-examination techniques as needed Support Systems: Ensuring adequate help with ongoing care
Understanding the genetic components of stage 0 melanoma helps patients make informed decisions about their care and family planning. While most melanomas occur sporadically, genetic factors can influence risk and treatment approaches.
Approximately 10% of melanomas occur as part of hereditary cancer syndromes:
CDKN2A Mutations: Most common hereditary melanoma gene CDK4 Mutations: Less common but significant risk factor BAP1 Mutations: Associated with uveal melanoma and other cancers MITF Mutations: Recently identified melanoma susceptibility gene
Genetic testing may be recommended for patients with:
When genetic factors are identified, family members may benefit from:
Enhanced Screening: More frequent skin examinations Genetic Counseling: Understanding inheritance patterns and risks Preventive Measures: Aggressive sun protection strategies Testing Options: Considering genetic testing for themselves
Modern medicine continues to develop new approaches for diagnosing and monitoring stage 0 melanoma. These advanced techniques improve accuracy and help detect changes earlier than traditional methods.
Digital dermoscopy enhances the ability to detect melanoma by:
Magnification: Providing detailed views of skin structures Digital Storage: Creating permanent records for comparison Computer Analysis: Using algorithms to identify suspicious patterns Telemedicine: Allowing remote consultation with specialists
This non-invasive imaging technique offers:
Real-Time Imaging: Viewing skin structures without biopsy Cellular Detail: Examining individual cell characteristics Margin Assessment: Helping determine surgical boundaries Research Applications: Contributing to melanoma research
AI technology is increasingly used for:
Pattern Recognition: Identifying subtle changes in moles Risk Assessment: Calculating probability of malignancy Screening Efficiency: Improving dermatologist accuracy Early Detection: Finding melanomas that might be missed
These technologies complement but don't replace traditional examination and biopsy techniques. They serve as additional tools to improve diagnostic accuracy and patient outcomes.
While treatment remains the primary focus for stage 0 melanoma, nutrition and lifestyle factors may play supportive roles in recovery and prevention of future skin cancers.
Certain nutrients may offer protective benefits:
🥕 Beta-Carotene: Found in orange and yellow vegetables
🥕 Vitamin D: Essential for immune function (with careful sun exposure)
🥕 Omega-3 Fatty Acids: May have anti-inflammatory properties
🥕 Antioxidants: Vitamin C, E, and selenium support cellular health
🥕 Polyphenols: Found in green tea, dark chocolate, and berries
A melanoma-conscious diet might include:
Beyond nutrition, other lifestyle elements that may influence skin health include:
Regular Exercise: Supports immune function and overall health Stress Management: Chronic stress may affect immune response Adequate Sleep: Essential for cellular repair and immune function Hydration: Maintains skin health and overall cellular function Avoiding Smoking: Smoking may increase skin cancer risk
Understanding the financial aspects of stage 0 melanoma treatment helps patients plan appropriately and access necessary care without undue financial stress.

Typical costs associated with stage 0 melanoma care include:
Initial Consultation: Dermatologist examination and evaluation Biopsy Procedures: Tissue sampling and pathological analysis Surgical Treatment: Excision procedure and facility fees Pathology Review: Microscopic examination of removed tissue Follow-up Care: Ongoing monitoring and examinations
Most health insurance plans cover medically necessary melanoma care:
Diagnostic Procedures: Biopsies and necessary imaging Surgical Treatment: Excision procedures for confirmed melanoma Follow-up Monitoring: Regular dermatological examinations Genetic Testing: When medically indicated
Patients can manage costs by:
The field of stage 0 melanoma research continues to evolve, with new developments promising to improve detection, treatment, and prevention strategies.
Biomarker Development: Identifying blood or tissue markers that predict recurrence risk Immunotherapy Applications: Exploring immune system enhancement for prevention Genetic Research: Understanding hereditary factors more completely Prevention Studies: Testing new approaches to reduce melanoma development Technology Integration: Improving AI and imaging technologies
Several promising technologies are under development:
Liquid Biopsies: Blood tests that might detect circulating tumor cells Advanced Imaging: New techniques for non-invasive melanoma detection Personalized Medicine: Tailoring treatment based on genetic profiles Prevention Vaccines: Experimental vaccines to prevent melanoma development
Patients with stage 0 melanoma might consider participating in:
These studies contribute to advancing melanoma care while potentially providing access to cutting-edge treatments.
Successfully managing stage 0 melanoma often involves coordinating care among multiple healthcare professionals. Building an effective team ensures comprehensive care and optimal outcomes.
Dermatologist: Primary specialist for skin cancer diagnosis and treatment Dermatopathologist: Specialist in microscopic examination of skin tissue Surgeon: May be needed for complex excision procedures Primary Care Physician: Coordinates overall health care Genetic Counselor: Provides guidance on hereditary risk factors
When selecting providers, consider:
Experience with Melanoma: Look for providers who regularly treat skin cancers Board Certification: Ensure appropriate specialty training and certification Communication Style: Choose providers who explain things clearly Location and Accessibility: Consider convenience for regular follow-up care Insurance Acceptance: Verify coverage before beginning treatment
Effective care coordination involves:
Being an informed patient involves asking the right questions about your stage 0 melanoma diagnosis and treatment. Preparing questions in advance helps ensure you get the information you need.
Don't hesitate to ask for clarification if you don't understand something. Consider bringing a family member or friend to appointments to help remember important information.
Dealing with stage 0 melanoma becomes easier when patients have access to reliable resources and support systems. Multiple organizations and tools are available to help patients navigate their diagnosis and treatment.
American Cancer Society: Comprehensive information about melanoma and treatment options Skin Cancer Foundation: Specialized resources for skin cancer education and prevention National Cancer Institute: Government-sponsored research and educational materials Melanoma Research Foundation: Patient-focused resources and support programs
Skin Cancer Apps: Mobile applications for tracking moles and skin changes Sun Safety Resources: UV index monitoring and protection guidance Medical Journals: Access to current research for interested patients Support Forums: Online communities for sharing experiences and advice
Many communities offer local resources such as:
Social Workers: Help navigate healthcare systems and access resources Patient Navigators: Guide patients through treatment processes Counselors: Provide emotional support and coping strategies Financial Counselors: Assist with insurance and payment issues
Developing a personalized action plan helps patients take control of their stage 0 melanoma care and maintain long-term skin health. This plan should be comprehensive yet practical for daily implementation.
Schedule Treatment: Arrange surgical consultation and procedure Gather Information: Collect all medical records and test results Notify Family: Inform close family members about diagnosis and hereditary considerations Insurance Review: Understand coverage and any pre-authorization requirements
Regular Monitoring: Maintain schedule of professional skin examinations Prevention Focus: Continue strict sun protection and avoidance strategies Family Education: Ensure family members understand their risk and prevention needs Health Maintenance: Maintain overall health through diet, exercise, and lifestyle choices Stay Informed: Keep up with new developments in melanoma research and prevention
Know when to seek immediate medical attention:
Have contact information readily available for your healthcare team and know how to access urgent care when needed.
Stage 0 melanoma represents a highly treatable form of skin cancer with an excellent prognosis when properly managed. The key to success lies in early detection, appropriate treatment, and ongoing prevention strategies. While receiving any cancer diagnosis can be frightening, patients diagnosed with stage 0 melanoma can feel confident about their outlook when working with qualified healthcare providers.
The journey from diagnosis to recovery involves several important steps: understanding the diagnosis, pursuing appropriate treatment, implementing prevention strategies, and maintaining regular follow-up care. Each of these elements plays a crucial role in achieving the best possible outcomes.
Prevention remains paramount even after successful treatment. Sun protection, regular skin examinations, and healthy lifestyle choices significantly reduce the risk of developing future skin cancers. The habits developed during treatment and recovery often lead to improved overall health and well-being.
The medical community continues to advance understanding and treatment of melanoma through ongoing research and technological developments. Patients benefit from these advances through improved diagnostic techniques, more precise treatments, and better prevention strategies.
For those facing a stage 0 melanoma diagnosis, remember that this represents the earliest possible detection of melanoma – a situation that offers the best possible outcomes. With proper care and attention, patients can expect to return to normal, healthy lives while maintaining vigilance about their skin health.
Take an active role in your care by staying informed, asking questions, and working closely with your healthcare team. The combination of medical expertise and patient engagement creates the foundation for successful treatment and long-term health.
If you're concerned about skin changes or need specialized care for melanoma, consider consulting with experienced professionals who understand the complexities of skin cancer treatment. Contact specialized providers who can offer comprehensive evaluation and treatment options tailored to your specific needs.
Remember, early detection and proper treatment of stage 0 melanoma lead to excellent outcomes. Stay vigilant about skin health, maintain regular check-ups, and don't hesitate to seek professional evaluation for any concerning skin changes. Your proactive approach to skin health is the best investment in your long-term well-being.