A skin tag on the tongue, medically known as an oral fibroma or fibroepithelial polyp, is a small, painless growth that can develop on the surface of the tongue. While these benign lesions are typically harmless, they can cause discomfort when eating, speaking, or performing other oral activities. Understanding the nature of tongue skin tags, their causes, and available treatment options is essential for anyone experiencing this common oral condition.
Oral health concerns often go unnoticed until they cause significant discomfort. A skin tag on the tongue represents one such condition that may initially seem minor but could potentially impact daily activities and quality of life. This comprehensive guide aims to provide valuable insights into tongue skin tags, helping readers make informed decisions about their oral health.

A skin tag on the tongue, also known as an oral fibroma, is a small, soft tissue growth that protrudes from the tongue's surface. These benign lesions typically appear as small, flesh-colored or slightly darker outgrowths that may be attached to the tongue by a thin stalk (pedunculated) or have a broader base (sessile). Tongue skin tags consist primarily of fibrous connective tissue covered by normal oral mucosa.
Unlike skin tags that appear on other parts of the body, tongue skin tags have some distinct characteristics due to their location in the moist environment of the oral cavity. They can vary in size from a few millimeters to several centimeters, though most remain relatively small. Their texture may range from soft and pliable to firm, depending on the amount of fibrous tissue present.
Oral fibromas, including skin tags on the tongue, are among the most common benign soft tissue growths in the oral cavity. They can affect individuals of any age, though they are more frequently observed in adults than in children. Studies suggest that approximately 1-2% of adults may develop oral fibromas at some point in their lives.
Interestingly, there appears to be a slight gender predisposition, with some research indicating that women may be more susceptible to developing tongue skin tags than men. This gender difference might be related to hormonal factors, though conclusive evidence is still lacking.
Skin tags can develop on various parts of the tongue, though certain locations are more common than others:
The location of a tongue skin tag can significantly influence the symptoms experienced and the treatment approach recommended by healthcare providers at specialized facilities like The Minor Surgery Center.
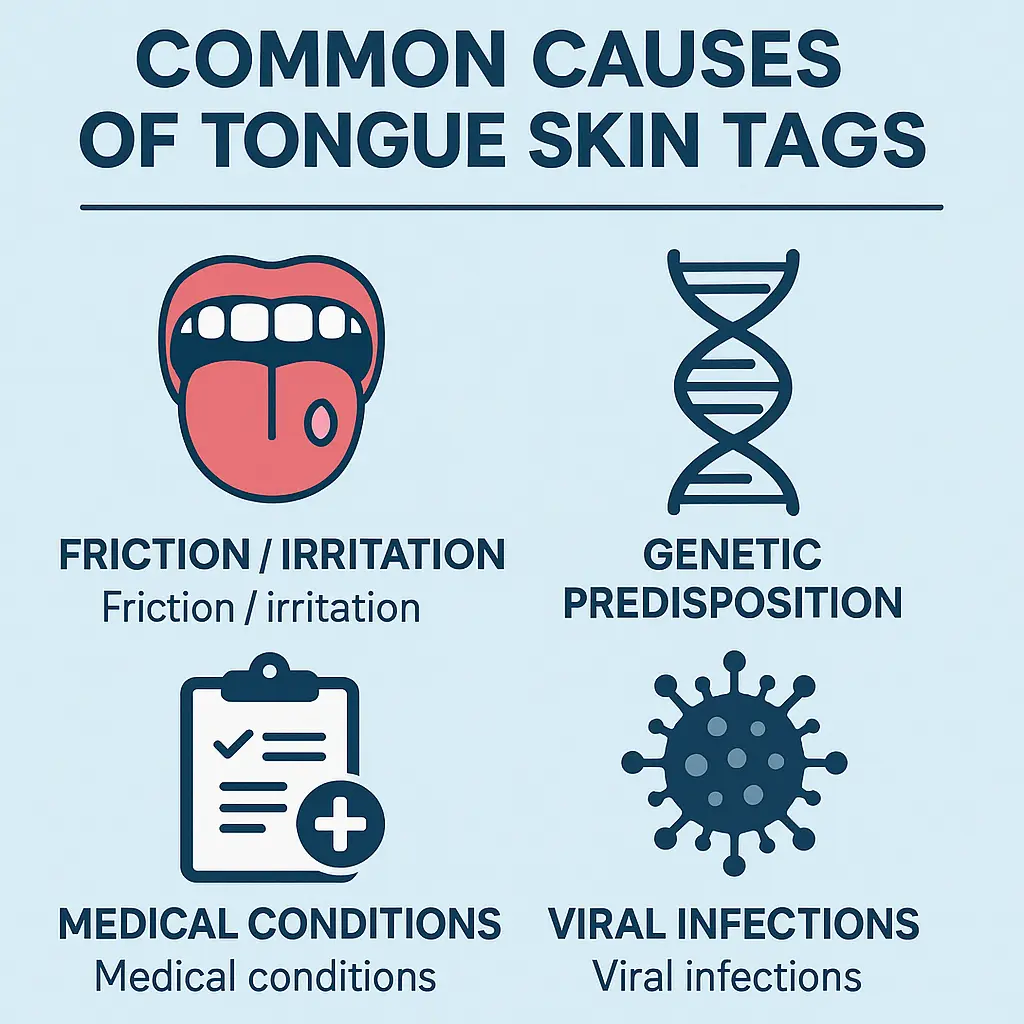
The most common cause of skin tags on the tongue is chronic irritation or trauma. The tongue is constantly moving during speaking, eating, and swallowing, making it susceptible to friction against teeth, dental appliances, or rough food textures. Specific sources of irritation that may lead to tongue skin tag formation include:
When the tongue tissue experiences repeated trauma, the body's healing response may sometimes result in excessive tissue growth, leading to the formation of a fibroma or skin tag.
Genetic factors may play a role in determining an individual's susceptibility to developing oral fibromas, including skin tags on the tongue. Some people appear to have a genetic predisposition that makes their oral tissues more likely to respond to irritation by forming fibrous growths. This genetic component may explain why certain individuals develop tongue skin tags despite minimal irritation, while others do not develop them even with significant oral trauma.
Family history of oral fibromas or similar soft tissue growths might indicate a higher risk for developing tongue skin tags, though comprehensive research in this area remains limited.
Several medical conditions have been associated with an increased risk of developing skin tags on the tongue:
Oral Papillomatosis: This condition, characterized by multiple papilloma (wart-like) growths in the oral cavity, can sometimes manifest as lesions resembling skin tags on the tongue.
Cowden Syndrome: A rare genetic disorder that causes multiple hamartomas (benign tumors) throughout the body, including the oral cavity.
Oral Fibrosis: Conditions that cause fibrous tissue changes in the mouth may increase the likelihood of fibroma development.
Diabetes: Some studies suggest that individuals with diabetes may have a higher incidence of oral fibromas, possibly due to impaired wound healing and altered tissue responses.
For individuals with these conditions, regular oral examinations by healthcare professionals at specialized clinics are particularly important for early detection and management of oral lesions.
Certain viral infections have been implicated in the development of oral lesions that may resemble skin tags:
Human Papillomavirus (HPV): Some strains of HPV can cause oral papillomas that may initially appear similar to skin tags. These virus-induced growths typically have a more irregular, cauliflower-like appearance upon closer examination.
Herpes Simplex Virus: While herpes primarily causes ulcerative lesions, recurrent infections and the subsequent healing process might occasionally contribute to fibrous tissue formation.
It's important to note that true fibromas (skin tags) are not directly caused by viral infections, but viral-induced lesions may be mistaken for skin tags, highlighting the importance of professional diagnosis.
Identifying a skin tag on the tongue requires understanding its typical physical characteristics:
Unlike some other oral lesions, tongue skin tags typically maintain a consistent appearance over time unless they experience further irritation or trauma.
While many skin tags on the tongue remain asymptomatic, they can cause various symptoms depending on their size, location, and individual factors:
Physical Sensations:
Functional Impacts:
Psychological Effects:
It's worth noting that pain is not typically associated with tongue skin tags unless they become irritated, inflamed, or traumatized. Persistent pain should prompt immediate medical evaluation to rule out other conditions.
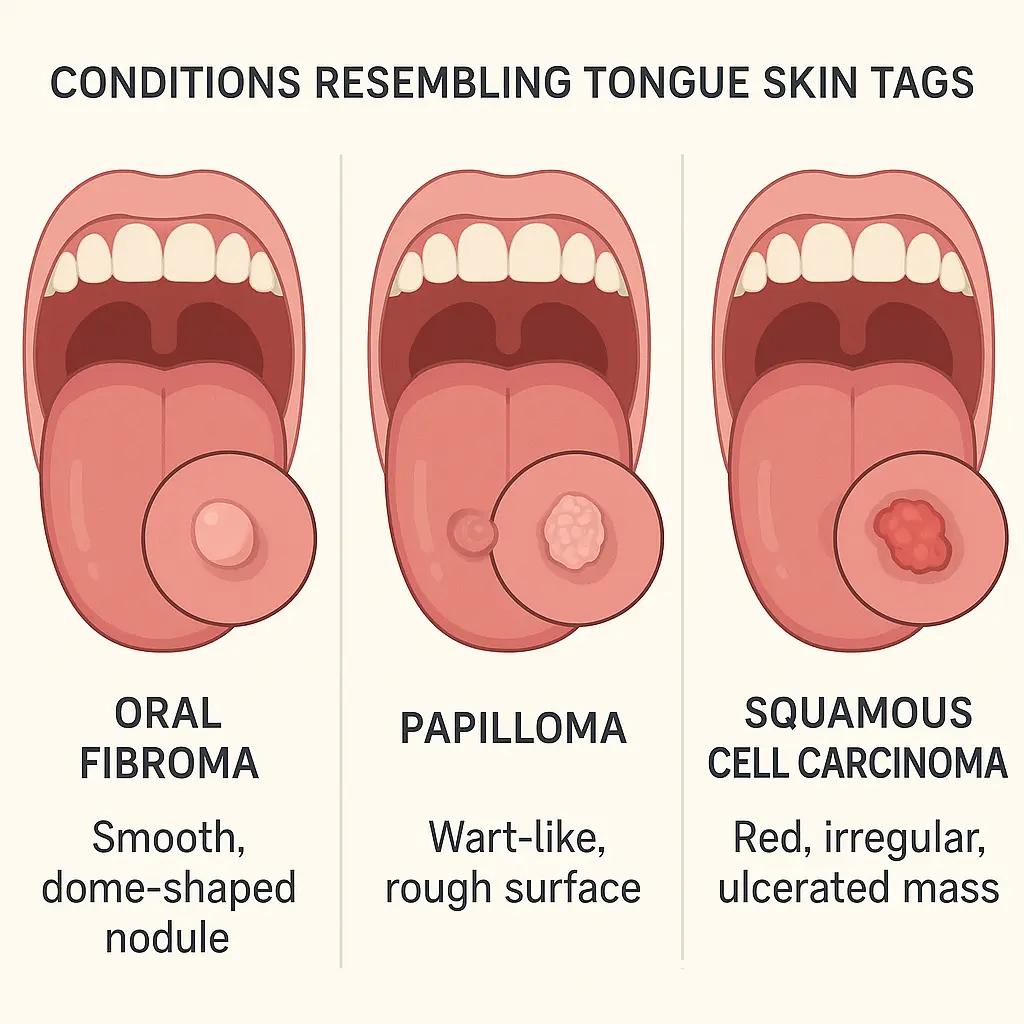
Several oral conditions can resemble skin tags on the tongue, making professional diagnosis essential. Key differential diagnoses include:
ConditionDistinguishing FeaturesLevel of ConcernOral Fibroma (Skin Tag)Smooth, same color as surrounding tissue, painlessLow (benign)MucoceleFluid-filled, bluish, may rupture and reformLow (benign)PapillomaCauliflower-like surface, possible HPV associationLow-ModerateSquamous Cell CarcinomaIrregular borders, hardened texture, may ulcerate, often painfulHigh (malignant)LeukoplakiaWhite patch that cannot be scraped off, potential precancerousModerate-HighGeographic TongueChanging pattern of smooth red patches with white bordersLow (benign)
Self-diagnosis is strongly discouraged due to the potential for misidentification. Healthcare professionals at The Minor Surgery Center have the expertise and tools necessary to accurately diagnose oral lesions and recommend appropriate treatment.
While most skin tags on the tongue are benign, certain signs and symptoms warrant prompt medical attention:
These warning signs might indicate a more serious condition that requires immediate evaluation by a healthcare professional.
Professional diagnosis of tongue lesions is crucial for several reasons:
The diagnostic process typically involves a thorough oral examination, medical history review, and possibly additional testing such as biopsy for definitive tissue analysis.
For evaluation and treatment of a skin tag on the tongue, several types of healthcare providers may be consulted:
Dentist: Often the first healthcare professional to identify oral lesions during routine dental examinations.
Oral Medicine Specialist: Dentists with advanced training in the diagnosis and management of oral conditions.
Oral and Maxillofacial Surgeon: Specialists who can surgically remove oral lesions when necessary.
Otolaryngologist (ENT): Physicians specializing in conditions of the ear, nose, and throat, including the oral cavity.
Dermatologist: While primarily focused on skin conditions, some dermatologists also treat oral lesions.
Specialized facilities like The Minor Surgery Center offer comprehensive evaluation and treatment options for oral lesions including tongue skin tags. When selecting a provider, consider factors such as:
Many patients find it helpful to review the credentials and experience of the medical team before scheduling a consultation.
The diagnostic journey for a skin tag on the tongue typically begins with a comprehensive clinical examination. During this assessment, the healthcare provider will:
The clinical examination provides valuable initial information but may need to be supplemented with additional diagnostic procedures for definitive diagnosis.
For definitive diagnosis of a tongue lesion, a biopsy may be recommended. This involves removing a small tissue sample for microscopic examination by a pathologist. Several biopsy techniques may be employed:
Excisional biopsy: The entire lesion is removed and examined. This serves both diagnostic and therapeutic purposes for small lesions.
Incisional biopsy: Only a portion of a larger lesion is removed for analysis.
Punch biopsy: A specialized circular tool removes a cylindrical tissue sample.
The tissue sample undergoes histopathological analysis, which can definitively identify the nature of the lesion. For true skin tags (fibromas), typical findings include:
This analysis is crucial for distinguishing benign fibromas from potentially serious conditions like squamous cell carcinoma or other oral malignancies.
In certain cases, particularly when there are concerning features or when planning complex treatments, advanced imaging or additional tests may be recommended:
Oral or Maxillofacial CT Scan: Provides detailed cross-sectional images that can show the extent of larger lesions and their relationship to surrounding structures.
MRI: Offers excellent soft tissue contrast, helpful for evaluating lesions with deep extension or when nerve involvement is suspected.
Toluidine Blue Staining: A simple chairside test where a dye preferentially stains abnormal tissues, helping identify areas of concern.
Brush Cytology: A less invasive alternative to traditional biopsy where cells are collected from the surface of the lesion for preliminary analysis.
The healthcare providers at specialized treatment centers can determine which diagnostic approaches are most appropriate based on the specific characteristics of each case.
Not all skin tags on the tongue require immediate treatment, particularly if they are small, asymptomatic, and have been professionally confirmed as benign. Conservative management options include:
Watchful Waiting: Regular monitoring of the lesion for any changes in size, appearance, or symptoms. This approach is suitable for small, stable lesions that don't interfere with function.
Irritation Reduction: Identifying and addressing factors that may be irritating the tongue and contributing to the skin tag's growth or discomfort:
Oral Rinses: Antiseptic mouth rinses may help reduce inflammation around the lesion and prevent secondary infection, though they won't eliminate the skin tag itself.
For patients choosing conservative management, regular follow-up examinations are essential to monitor for any concerning changes that might necessitate more definitive treatment.
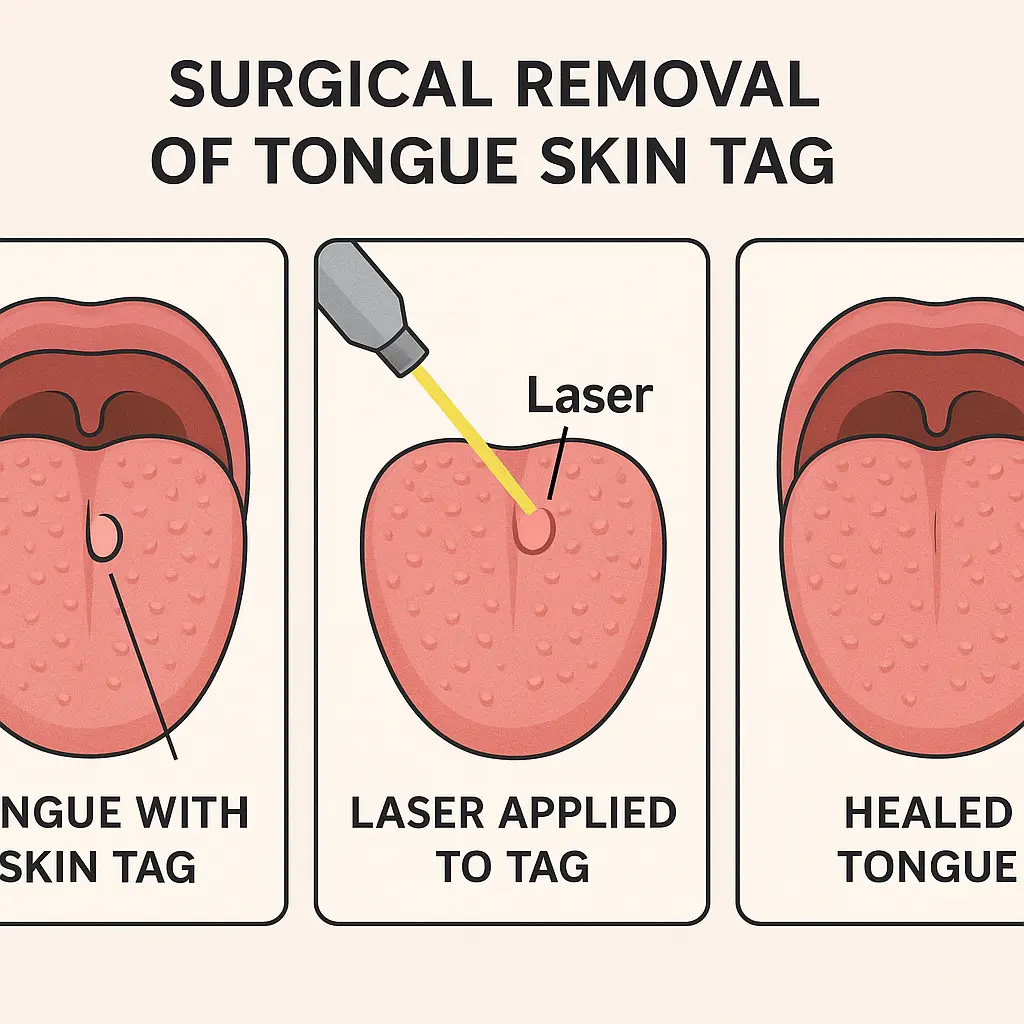
Surgical removal is the most definitive treatment for skin tags on the tongue and offers the advantage of providing tissue for pathological examination. Common surgical approaches include:
Conventional Excision: The most traditional approach involves removing the lesion with a scalpel under local anesthesia. The wound may be closed with sutures that typically dissolve within 7-10 days.
Electrosurgical Excision: Uses electrical current to simultaneously cut tissue and coagulate blood vessels, reducing bleeding. This technique is particularly useful for vascular lesions.
Laser Excision: Employs focused laser energy to precisely remove the lesion with minimal damage to surrounding tissues. Benefits include reduced bleeding, swelling, and post-operative discomfort.
Cryosurgery: Involves freezing the lesion with liquid nitrogen or other cryogenic substances, causing cellular destruction and eventual sloughing of the tissue. This technique may be less precise but is sometimes preferred for smaller lesions.
The surgical approach is typically determined based on factors such as:
Most surgical procedures for tongue skin tags are performed on an outpatient basis at facilities like The Minor Surgery Center, with patients returning home the same day.
Proper recovery and follow-up care are essential for optimal healing after tongue skin tag removal:
Immediate Post-Procedure Care (First 24-48 hours):
Short-term Recovery (3-7 days):
Long-term Follow-up:
Most patients experience complete healing within 2-3 weeks, with minimal long-term effects. The tongue's rich blood supply typically facilitates rapid healing compared to other body sites. However, patients should promptly report any unusual symptoms during recovery to their healthcare provider.
For detailed information about specific procedures and recovery expectations, patients can consult the FAQs section of specialized treatment centers.
Maintaining excellent oral hygiene is fundamental to preventing many oral conditions, including some of the factors that may contribute to tongue skin tags:
Effective Brushing Techniques:
Interdental Cleaning:
Antimicrobial Rinses:
Proper oral hygiene reduces inflammation and irritation in the oral cavity, potentially decreasing the risk of reactive tissue growth like fibromas or skin tags.
Certain lifestyle factors can influence oral health and potentially affect the development or recurrence of tongue skin tags:
Dietary Considerations:
Harmful Habits to Avoid:
Stress Management:
These lifestyle modifications contribute to overall oral health and may help reduce risk factors associated with tongue irritation and subsequent skin tag development.
Regular professional dental examinations play a crucial role in preventing and detecting oral conditions early:
Recommended Frequency:
Benefits of Regular Examinations:
Professional Assessment:
Maintaining a relationship with dental professionals ensures that any developing oral conditions, including tongue skin tags, can be addressed promptly and appropriately. Many dental practices work collaboratively with specialized treatment facilities like The Minor Surgery Center to provide comprehensive care for patients with oral lesions.
For individuals who have chosen not to remove a skin tag on the tongue or who are awaiting treatment, several strategies can help manage associated discomfort:
Dietary Adjustments:
Topical Remedies (with healthcare provider approval):
Physical Protection:
Patients should document any changes in symptoms or in the appearance of the skin tag and report these to their healthcare provider during follow-up appointments.
The presence of a skin tag on the tongue can have psychological and social implications that extend beyond physical discomfort:
Self-consciousness and Body Image:
Communication Challenges:
Coping Strategies:
Healthcare providers should address both the physical and psychological aspects of living with a tongue skin tag, offering reassurance and comprehensive care that acknowledges these dimensions of the patient experience.
Learning from others who have experienced similar conditions can provide valuable perspective and reassurance. While individual experiences vary, common themes emerge from patient testimonials:
"I was initially very worried when I discovered the small growth on my tongue. After proper diagnosis and a simple outpatient procedure, I realized I had been unnecessarily anxious. The recovery was quick, and I'm grateful for the professional care I received." - Patient at The Minor Surgery Center
"Living with a small skin tag on my tongue for several years taught me it wasn't worth the worry. My dentist monitors it during my regular check-ups, and it causes no problems. Understanding that it's benign gave me peace of mind." - Long-term management patient
"The procedure to remove my tongue skin tag was much simpler than I expected. I had some soreness for a few days, but within a week, I couldn't even tell anything had been there. I wish I hadn't postponed treatment out of fear." - Surgical removal patient
These experiences highlight the importance of professional diagnosis, the generally favorable outcomes of treatment, and the significant relief that comes with addressing both the physical condition and associated concerns.
Patients considering treatment options may find additional testimonials and information through the blog section of specialized treatment centers, where real patient experiences are often shared.
Many patients have questions and concerns about skin tags on the tongue, often fueled by misconceptions. Addressing these can provide valuable clarity:
Are tongue skin tags cancerous? No, true skin tags (fibromas) are benign growths. However, it's essential to have any oral lesion professionally evaluated to confirm its benign nature, as some more serious conditions can initially resemble skin tags.
Can tongue skin tags go away on their own? Unlike some other oral lesions, established fibromas typically don't resolve spontaneously. However, if the lesion is very small and the source of irritation is removed, it might occasionally regress. Most persistent lesions require professional treatment for removal.
Are tongue skin tags contagious? No, oral fibromas are not contagious and cannot be transmitted through kissing or sharing utensils. They are not caused by bacterial or viral infections (though some viral lesions may resemble skin tags).
Will removing a tongue skin tag leave a scar? Modern surgical techniques minimize scarring, and the tongue's excellent blood supply promotes rapid healing. Most patients experience little to no visible scarring after proper treatment and healing.
Do tongue skin tags always grow back after removal? When properly removed and if the underlying cause (such as chronic irritation) is addressed, most tongue skin tags do not recur. However, some individuals may be prone to developing new lesions in the same or different locations over time.
Financial aspects often influence treatment decisions for oral conditions:
Treatment Costs:
These figures are approximate and vary significantly based on geographic location, provider expertise, facility type, and complexity of the procedure.
Insurance Coverage: Most health insurance plans and some dental insurance policies cover the removal of oral lesions when medically necessary. Coverage typically depends on:
Patients are advised to:
Many treatment facilities, including The Minor Surgery Center, offer insurance verification services and financial counseling to help patients navigate these considerations.
Understanding the long-term prognosis helps patients make informed decisions about treatment:
Success Rates: The success rate for complete removal of tongue skin tags is very high, typically exceeding 95% with appropriate surgical techniques. Modern procedures generally result in excellent functional and aesthetic outcomes.
Recurrence Statistics:
Factors Influencing Recurrence:
Monitoring Recommendations: Even after successful treatment, regular oral examinations are recommended to:
The most favorable long-term outcomes are achieved through a combination of appropriate initial treatment, addressing underlying causes, and consistent follow-up care. Patients with questions about their specific prognosis can find additional information in the conditions section of specialized treatment centers.
Throughout this comprehensive guide, several critical aspects of tongue skin tags have been explored:
Nature and Characteristics: Skin tags on the tongue (oral fibromas) are benign soft tissue growths that typically develop in response to chronic irritation or trauma. They appear as small, flesh-colored protrusions that may be attached by a stalk or have a broader base.
Diagnosis and Evaluation: Professional diagnosis is essential to distinguish tongue skin tags from other oral conditions, including potentially serious ones. The diagnostic process may include clinical examination, biopsy, and occasionally advanced imaging.
Treatment Approaches: Options range from conservative management (for asymptomatic lesions) to various surgical removal techniques. The appropriate approach depends on the lesion's size, location, symptoms, and patient preferences.
Prevention and Management: Maintaining excellent oral hygiene, avoiding irritating factors, and attending regular dental check-ups can help prevent tongue skin tags and manage existing ones. Addressing underlying causes is crucial for preventing recurrence.
Long-term Considerations: With proper treatment, most tongue skin tags can be successfully managed with minimal risk of recurrence. Regular follow-up examinations remain important for monitoring oral health.
Individuals should seek professional evaluation for a suspected skin tag on the tongue in the following circumstances:
Early evaluation provides the best opportunity for accurate diagnosis, appropriate treatment planning, and peace of mind.
A skin tag on the tongue represents a common oral condition that, while typically benign, deserves proper attention and management. The key recommendations for individuals dealing with this condition include:
With appropriate care and attention, most patients can expect excellent outcomes and minimal long-term impact from tongue skin tags. For those seeking specialized care for oral lesions, contact a specialized treatment center to schedule a consultation with experienced professionals who can provide personalized guidance and treatment.
By understanding the nature of tongue skin tags and taking a proactive approach to their management, individuals can maintain optimal oral health and function while minimizing unnecessary anxiety about this common condition.