Every month, a simple 10-minute routine could save your life. With skin cancer affecting one in five Americans during their lifetime, learning how to perform proper skin self-exams represents one of the most powerful tools for early detection and successful treatment outcomes.
• Monthly skin self-exams should be performed after bathing in a well-lit room using both full-length and handheld mirrors
• Look for the "ABCDE" warning signs: Asymmetry, Border irregularities, Color changes, Diameter larger than a pencil eraser, and Evolving characteristics
• Document your baseline during the first examination to track changes over time using photos or body maps
• Examine every area including scalp, between toes, genital areas, and other commonly overlooked spots
• Seek professional evaluation for any new, changing, or unusual spots that concern you
Skin cancer represents the most common form of cancer in the United States, yet it's also among the most preventable and treatable when detected early [1]. The key lies in recognizing suspicious changes before they progress to advanced stages. Skin self-exams: how to check your own skin effectively can mean the difference between a simple outpatient procedure and extensive treatment requiring multiple interventions.
When melanoma is caught in its earliest stage, the five-year survival rate exceeds 99% [2]. However, this rate drops significantly as the cancer spreads to other parts of the body. This dramatic difference underscores why monthly self-examinations have become a cornerstone recommendation among dermatologists and cancer prevention specialists.
The process doesn't require medical training or expensive equipment. With proper technique and consistency, anyone can learn to monitor their skin effectively and identify changes that warrant professional evaluation at specialized medical facilities.
Proper lighting forms the foundation of an effective skin examination. Natural daylight provides the best illumination, but bright indoor lighting works well when natural light isn't available. Avoid dim lighting or colored bulbs that might mask subtle color changes in moles or lesions.
Temperature control matters more than many people realize. A comfortably warm room prevents shivering and allows for thorough examination without rushing. Cold environments can cause skin changes that might interfere with accurate assessment.
ItemPurposeAlternative OptionsFull-length mirrorFront and back body viewsLarge bathroom mirrorHandheld mirrorHard-to-reach areasCompact or makeup mirrorBright lightingClear visibilityDesk lamp or flashlightHair dryer or combScalp examinationHair clips for partingCamera/smartphoneDocumentationNotebook for written records
Monthly frequency represents the gold standard recommended by most dermatological organizations [3]. This interval allows sufficient time for meaningful changes to develop while maintaining familiarity with your normal skin patterns.
Post-shower timing offers practical advantages. The skin is clean, exposed, and you're already in a private setting with mirrors available. Many people find it easier to incorporate skin checks into existing bathroom routines rather than scheduling separate examination times.
For individuals with higher risk factors, some specialists recommend more frequent monitoring. Those with specific skin conditions may benefit from customized examination schedules developed with their healthcare providers.

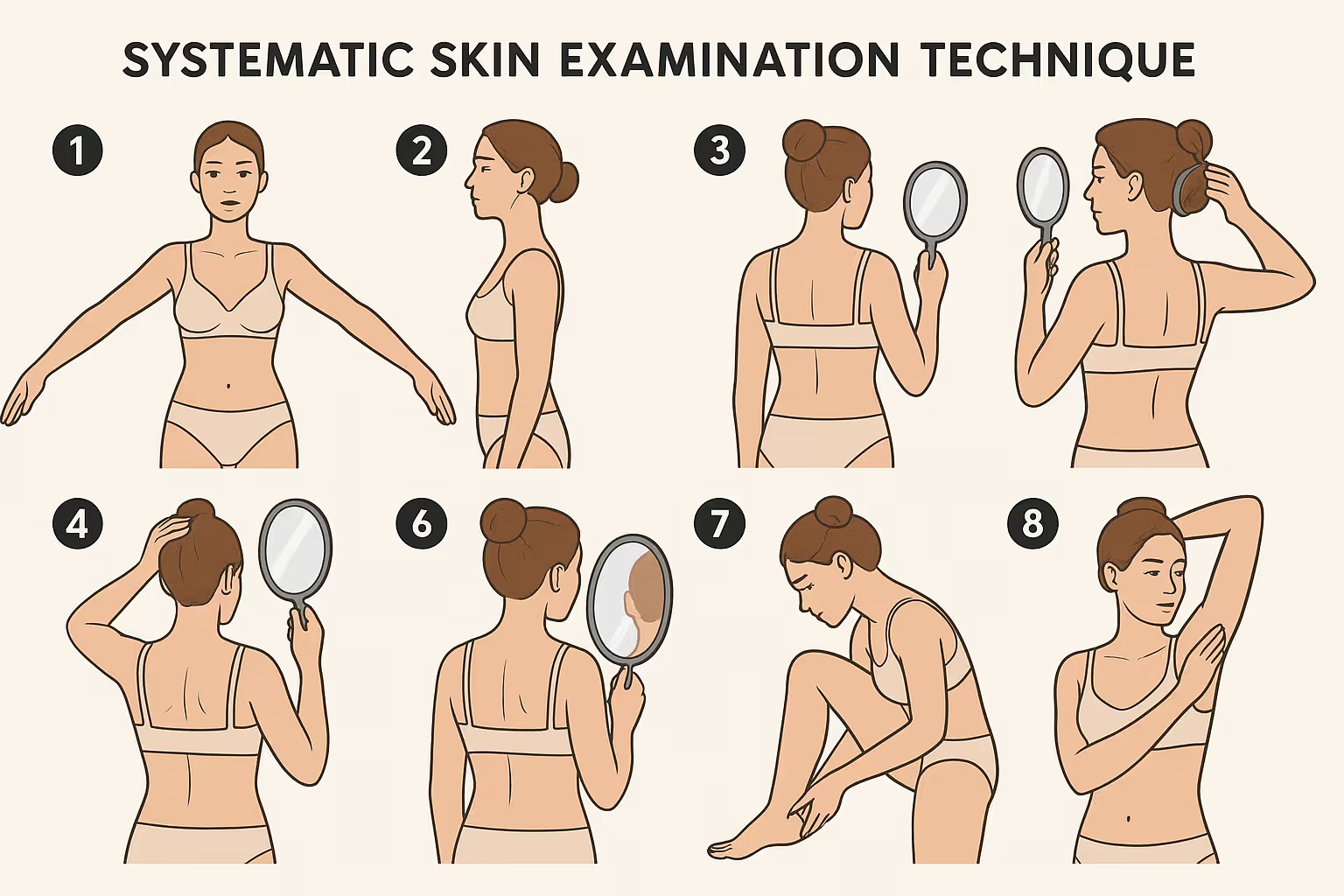
Begin your skin self-exam by standing directly in front of a full-length mirror in bright lighting. Start with your face and scalp, examining your forehead, temples, around your eyes, nose, cheeks, lips, and chin. Don't forget to check your ears, both front and back surfaces.
Neck examination requires careful attention to all angles. Turn your head left and right to visualize the sides of your neck, then tilt your head back to examine the front throat area. Use the handheld mirror to check the back of your neck thoroughly.
Move systematically to your chest and abdomen. Women should lift their breasts to examine the skin underneath, an area often overlooked but susceptible to skin cancer development. Check your underarm areas completely, as lymph node regions can sometimes develop suspicious lesions.
Arm examination should cover every surface methodically. Start with your shoulders and work down to your fingertips. Examine the fronts and backs of your upper arms, elbows, forearms, and wrists. Pay special attention to areas that receive frequent sun exposure.
Hand and finger assessment requires detailed attention. Check your palms, the backs of your hands, between your fingers, and under your fingernails. Melanoma can develop in unexpected locations, including areas with minimal sun exposure.
Leg inspection begins with sitting down for easier access. Examine the fronts of your thighs, knees, shins, and tops of your feet. Check between your toes and under your toenails, areas where melanoma occasionally develops.
Using your handheld mirror, examine the backs of your legs one at a time. Check your calves, the backs of your thighs, and your buttocks. These areas require careful mirror positioning for complete visualization.
Back examination presents the greatest challenge for self-assessment. Position yourself with your back to the full-length mirror while using the handheld mirror to systematically view your entire back surface. This technique requires practice but becomes easier with repetition.
For areas that remain difficult to see, consider asking a trusted family member or partner to assist. Many couples incorporate mutual skin checks into their monthly routines, providing an extra layer of protection for both partners.
Scalp examination often gets neglected despite being a common location for skin cancer, particularly in individuals with thinning hair or bald spots. Use a hair dryer on a cool setting or a comb to part your hair in sections, systematically checking your entire scalp.
Work from front to back, creating multiple parts to visualize all scalp areas. Pay particular attention to the crown of your head and areas where you might have experienced sunburn in the past.
A - Asymmetry: Healthy moles typically display symmetrical shapes. If you draw an imaginary line through the middle of a mole, both halves should look similar. Asymmetrical moles warrant professional evaluation.
B - Border Irregularity: Normal moles have smooth, even borders. Suspicious lesions often display uneven, scalloped, or notched edges that appear irregular or poorly defined.
C - Color Variation: Most benign moles maintain consistent coloring throughout. Multiple colors within a single mole, particularly black, brown, red, white, or blue variations, require medical assessment.
D - Diameter: While not absolute, moles larger than 6 millimeters (about the size of a pencil eraser) deserve attention, especially if they're new or changing.
E - Evolving: Any mole that changes in size, shape, color, elevation, or develops new symptoms like bleeding, itching, or crusting should be evaluated promptly.
The "Ugly Duckling" Sign 🦆 represents an important concept in skin cancer detection. This refers to moles that look distinctly different from your other moles. Even if a lesion doesn't meet ABCDE criteria, significant differences from your normal mole pattern warrant investigation.
New growths after age 30 require attention, particularly if they appear different from your existing moles. While new moles can be benign, they should be evaluated by professionals familiar with skin cancer diagnosis and treatment.
Non-healing sores that persist for several weeks, continue to bleed, or repeatedly scab and reopen may indicate skin cancer. These lesions often appear in sun-exposed areas like the face, ears, neck, or hands.
During your first comprehensive skin self-exam, spend extra time documenting your normal skin patterns. This baseline becomes invaluable for identifying changes during future examinations.
Photography provides the most accurate documentation method. Use your smartphone to photograph any moles or spots that concern you, ensuring good lighting and clear focus. Date-stamp these images and store them in a dedicated folder for easy comparison.
Body mapping offers an alternative or complementary approach. Several smartphone apps and printable charts allow you to mark mole locations and characteristics. This method works particularly well for tracking multiple spots across your body.
Monthly comparisons between current observations and your baseline documentation help identify subtle changes that might otherwise go unnoticed. Look for differences in size, color, texture, or shape.
Professional consultation becomes necessary when you notice any changes that concern you. Don't wait for annual check-ups if something appears different. Many specialized clinics offer prompt evaluation for concerning skin changes.
Family history of melanoma or other skin cancers significantly increases individual risk. People with affected first-degree relatives should be particularly vigilant about monthly self-examinations and annual professional screenings.
Previous skin cancer diagnosis creates elevated risk for developing additional skin cancers. These individuals often benefit from more frequent professional monitoring and should be especially thorough with self-examinations.
Immunosuppression from medications or medical conditions increases skin cancer risk. Organ transplant recipients, individuals with autoimmune diseases, and those taking immunosuppressive medications should prioritize regular skin monitoring.
Fair-skinned individuals with light hair and eyes face higher melanoma risk, but skin cancer can affect people of all skin tones and ethnicities. Darker-skinned individuals should pay particular attention to areas with less pigmentation, such as palms, soles, and nail beds.
Extensive sun exposure history, including severe sunburns, tanning bed use, or occupational outdoor work, increases risk regardless of current age. These individuals should be especially thorough during self-examinations.
New or changing lesions that concern you should prompt professional evaluation without delay. Trust your instincts—if something doesn't look right, seek medical opinion from qualified healthcare professionals.
Persistent symptoms like itching, bleeding, or pain in a mole or skin spot require medical assessment. These symptoms often indicate changes that warrant professional evaluation.
Rapid changes in any skin lesion, particularly growth, color changes, or development of irregular borders, should be evaluated promptly rather than waiting for the next scheduled appointment.
Annual dermatological examinations complement monthly self-exams for comprehensive skin cancer prevention. Professional screenings can identify suspicious lesions that might be missed during self-examination.
Specialized evaluation may be recommended for individuals with numerous moles, atypical mole patterns, or strong family histories. Some people benefit from professional photography and mapping services for enhanced monitoring.
Before seeking professional care, consider reviewing frequently asked questions about skin examinations and treatment options to better prepare for your consultation.
Smartphone apps designed for mole tracking offer sophisticated features for monitoring skin changes. Many include measurement tools, comparison features, and reminder systems for monthly examinations.
Digital photography techniques can improve documentation quality. Use consistent lighting, camera distance, and angles for accurate comparison over time. Some people find it helpful to include a ruler or coin for size reference.
Dermatoscopes designed for consumer use provide magnified views of skin lesions, though they require training for effective interpretation. These tools can supplement but shouldn't replace professional evaluation.
UV photography reveals sun damage not visible to the naked eye, helping identify areas requiring extra attention during self-examinations.

Breast self-exams for women provide an ideal opportunity to simultaneously perform skin checks. Both examinations require similar privacy, lighting, and mirror arrangements.
General health monitoring routines can incorporate skin checks efficiently. Many people find success linking skin examinations to other monthly health activities like weight monitoring or medication reviews.
Documentation sharing with your healthcare provider enhances professional evaluations. Bring photos or notes about concerning changes to medical appointments.
Risk assessment discussions with your doctor can help determine appropriate screening frequency and techniques based on your individual risk factors and medical history.
For those considering professional evaluation or treatment, understanding potential costs can help with planning and decision-making.
Time constraints represent the most common barrier to regular skin self-exams. However, thorough examinations typically require only 10-15 minutes monthly when incorporated into existing routines.
Privacy concerns can be addressed by scheduling examinations during times when you won't be interrupted. Many people find early morning or evening hours work best for comprehensive self-examination.
Physical limitations that make certain body areas difficult to examine can often be overcome with assistance from trusted family members or partners. Don't let physical challenges prevent you from monitoring accessible areas.
Calendar reminders help establish consistent monthly examination schedules. Many people choose the same date each month, such as the first or their birthday date, for easy remembering.
Routine integration works better than scheduling separate examination times. Linking skin checks to existing monthly activities increases compliance and sustainability.
While skin self-exams: how to check your own skin effectively forms a crucial component of cancer prevention, professional medical care remains irreplaceable for comprehensive skin health management. Self-examination serves as an early warning system, but trained dermatologists possess specialized knowledge and equipment for accurate diagnosis and treatment planning.
Professional screenings can identify suspicious lesions in areas difficult to self-examine and detect subtle changes that might escape notice during self-assessment. Many skin cancers develop in locations that are challenging to see without assistance, making regular professional evaluation essential for complete protection.
The combination of monthly self-examinations and annual professional screenings provides the most comprehensive approach to skin cancer prevention and early detection. This dual strategy maximizes the chances of identifying concerning changes when treatment options are most effective and outcomes are most favorable.
For additional resources and information about skin health and cancer prevention, explore comprehensive educational materials that can enhance your understanding of proper skin care and monitoring techniques.

Skin self-exams: how to check your own skin effectively represents one of the most important preventive health practices you can adopt. With skin cancer affecting millions of Americans annually, the ability to detect suspicious changes early can literally save lives while minimizing treatment complexity and improving outcomes.
The monthly examination routine outlined in this guide requires minimal time investment but offers substantial health protection benefits. By systematically checking every area of your body, documenting baseline patterns, and monitoring for changes using the ABCDE criteria, you create a powerful early detection system for skin cancer and other concerning skin conditions.
Take action today by scheduling your first comprehensive skin self-examination. Gather the necessary tools, set aside adequate time, and begin establishing this life-saving monthly habit. Remember that self-examination complements but doesn't replace professional medical care—maintain regular dermatological check-ups and seek prompt evaluation for any concerning changes you discover.
Your skin health deserves the same attention you give to other aspects of preventive healthcare. Start your monthly skin self-examination routine now and take control of your skin cancer prevention strategy. For professional evaluation of any concerning findings, consider consulting with experienced healthcare providers who specialize in skin health and minor surgical procedures when treatment becomes necessary.
[1] American Cancer Society. (2025). Skin Cancer Prevention and Early Detection.
[2] Skin Cancer Foundation. (2025). How to Do a Skin Self-Exam.
[3] American Academy of Dermatology. (2025). How to perform a skin self-exam.
[4] National Cancer Institute. (2025). Skin Cancer Screening.
[5] Mayo Clinic. (2025). Melanoma: Symptoms and Causes.
[6] Cleveland Clinic. (2025). Skin Cancer Self-Examination.
[7] Harvard Health Publishing. (2025). The importance of skin self-exams.
[8] Johns Hopkins Medicine. (2025). Skin Cancer Detection and Prevention.
[9] Dermatology Times. (2025). Best practices for skin self-examination.