Picture this: you're getting ready for the day when you notice a small, dark spot on your shoulder that you've never seen before. Your mind immediately races with questions—is it dangerous? Should you be worried? Understanding skin mole types can help you distinguish between harmless beauty marks and spots that require medical attention. With millions of people developing new moles throughout their lives, knowing what to look for could literally save your life.
• Common moles are typically harmless, symmetrical, and uniform in color, while atypical moles may show irregular features that warrant monitoring

• The ABCDE criteria (Asymmetry, Border, Color, Diameter, Evolving) helps identify potentially concerning mole changes
• Congenital moles present at birth carry different risk factors than acquired moles that develop over time
• Regular skin examinations by dermatologists are crucial for early detection of skin cancer, especially for high-risk individuals
• Most moles are benign, but any changing or new moles after age 30 should be evaluated by a medical professional
Moles, medically known as nevi, are clusters of pigmented cells called melanocytes that appear as spots on the skin. These common skin growths develop when melanocytes grow in clusters instead of spreading evenly throughout the skin. Understanding the different skin mole types begins with recognizing that moles are incredibly common—most adults have between 10 to 40 moles on their body.
The formation of moles involves complex interactions between genetics, sun exposure, and hormonal changes. Melanocytes produce melanin, the pigment responsible for skin color and protection against UV radiation. When these cells cluster together, they create the various mole types we see on our skin.
Several factors contribute to mole formation and the specific skin mole types that develop:
Most moles fall into the benign category, meaning they're harmless and pose no health risks. However, understanding the characteristics of different skin mole types helps distinguish normal variations from potentially concerning changes.
Junctional moles appear at the junction between the epidermis (outer skin layer) and dermis (deeper skin layer). These moles typically present as:
Junctional moles are among the most common skin mole types and rarely become problematic. They often develop during childhood and may fade or disappear with age.
Compound moles contain melanocytes in both the epidermis and dermis, creating a distinctive appearance:
These moles represent a natural progression from junctional moles as melanocytes migrate deeper into the skin. The presence of hair in a compound mole is actually a reassuring sign of benign behavior.
Intradermal moles develop entirely within the dermis and represent the final stage of mole evolution:
These moles often lose their pigmentation over time and may become skin-colored. They're considered the most stable of all skin mole types and rarely undergo malignant transformation.
While most moles are harmless, certain skin mole types require closer monitoring due to their increased risk of developing into melanoma or other skin cancers.
Dysplastic nevi are unusual moles that share some characteristics with melanoma but aren't cancerous. Key features include:
🚨 Important: People with dysplastic nevi have a 4-12 times higher risk of developing melanoma compared to those without these atypical moles.
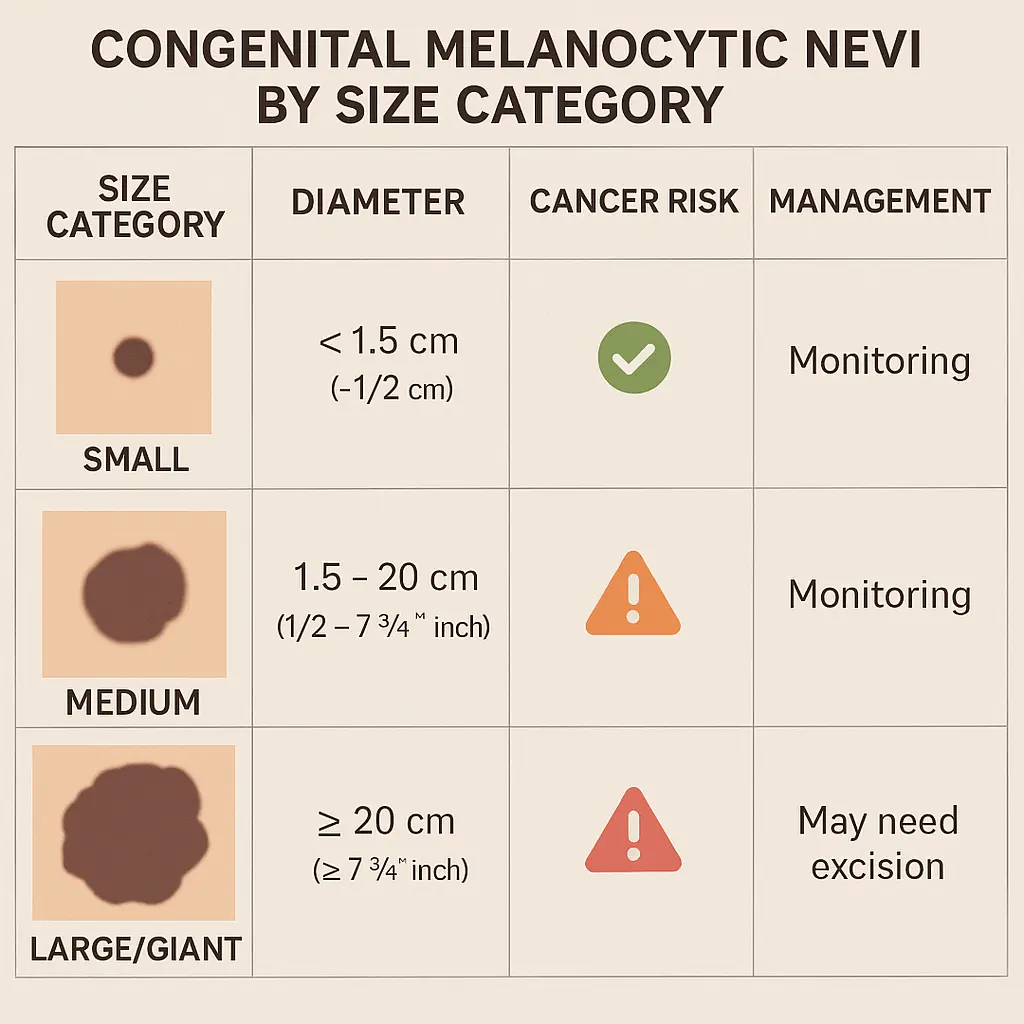
Congenital melanocytic nevi are moles present at birth, affecting approximately 1% of newborns. These skin mole types are classified by size:
Size CategoryDiameterCancer RiskManagementSmall<1.5 cmVery lowRoutine monitoringMedium1.5-19.9 cmLow to moderateRegular dermatology follow-upLarge/Giant≥20 cmModerate to highMultidisciplinary care
Large congenital nevi carry the highest risk of malignant transformation, with studies showing a 5-10% lifetime risk of developing melanoma.
Blue nevi are distinctive skin mole types characterized by their blue or blue-black coloration. They occur when melanocytes are trapped deep in the dermis, creating a blue appearance due to light scattering. Features include:
Most blue nevi are benign, but cellular blue nevi can occasionally undergo malignant transformation and require monitoring.
The ABCDE criteria provide a systematic approach to evaluating skin mole types and identifying potentially dangerous changes. This method helps both healthcare providers and patients recognize warning signs that warrant professional evaluation.
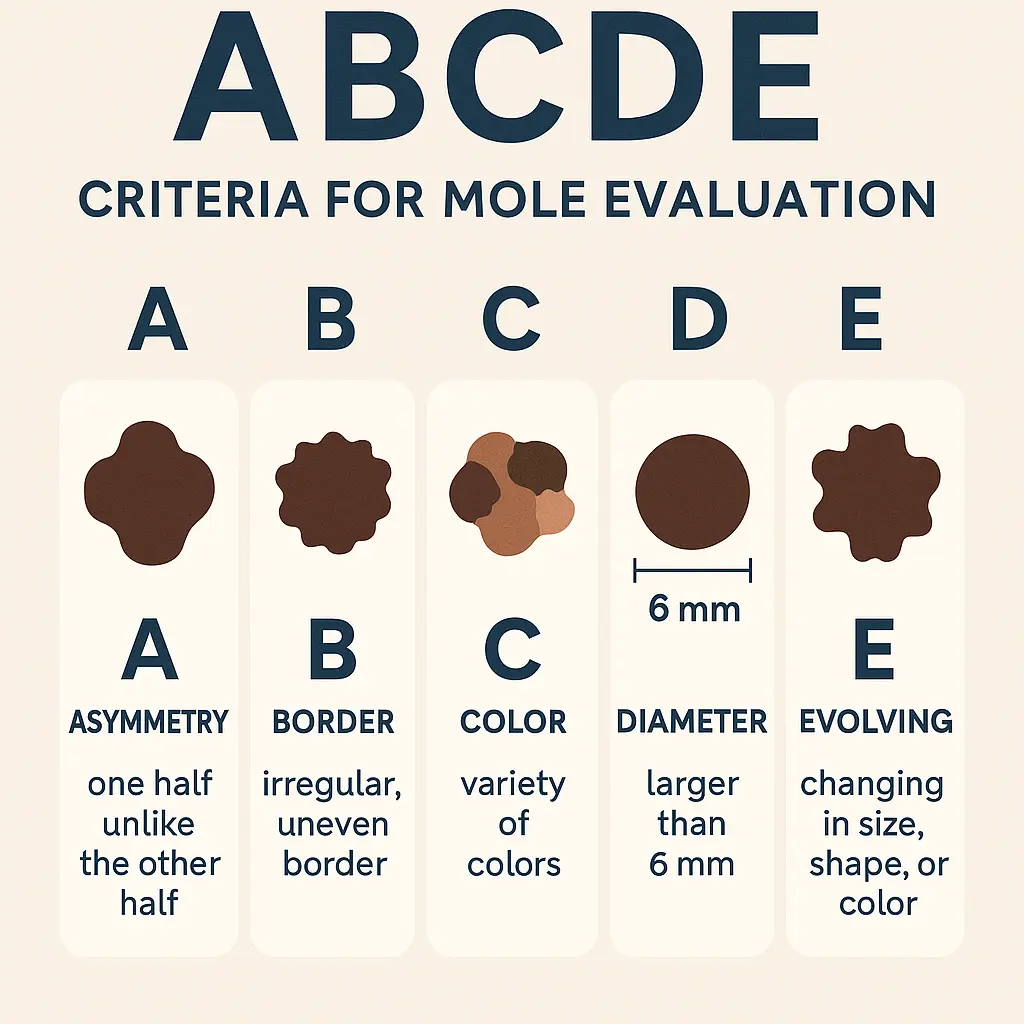
Asymmetrical moles have one half that doesn't match the other half. Benign moles are typically symmetrical, meaning if you draw a line through the middle, both sides should look similar.
Border characteristics provide important clues about mole behavior:
Color consistency is a key indicator of mole stability:
Size considerations help identify problematic skin mole types:
Changes over time represent the most important warning sign:
Understanding how various factors influence skin mole types helps create personalized monitoring strategies. Different populations and circumstances require tailored approaches to mole evaluation and management.
Pediatric mole development follows predictable patterns that differ from adult skin mole types:
Key considerations for young patients:
Hormonal fluctuations significantly impact skin mole types during pregnancy:
Pregnant women should maintain regular skin monitoring while understanding that most changes are benign and hormone-related.
Chronic sun exposure influences both mole development and the appearance of other skin mole types:
Knowing when to consult healthcare professionals about skin mole types can be lifesaving. While most moles are harmless, certain situations warrant immediate medical attention.
Immediate medical evaluation is necessary for moles showing:
Regular professional examinations should follow these guidelines:
Risk CategoryExamination FrequencySpecial ConsiderationsLow RiskAnnualRoutine skin checksModerate RiskEvery 6 monthsPersonal/family historyHigh RiskEvery 3-4 monthsMultiple risk factorsVery High RiskAs directedPrevious melanoma
Maximize your dermatology visit by:
Professional evaluation at specialized clinics ensures comprehensive assessment using advanced diagnostic tools and expertise.
When skin mole types require intervention, several treatment options are available depending on the mole's characteristics, location, and underlying concerns.
Medical reasons for mole removal include:
Cosmetic considerations may also warrant removal:
Excisional biopsy represents the gold standard for suspicious skin mole types:
Shave excision may be appropriate for clearly benign moles:
Post-procedure care ensures optimal healing:
Professional surgical centers provide comprehensive care from initial evaluation through complete recovery.
While genetic factors influence skin mole types, several strategies can reduce the risk of developing problematic moles and skin cancer.
Comprehensive sun protection forms the foundation of prevention:
Behavioral changes that reduce mole-related risks:
Individuals with increased risk require enhanced prevention:
Modern technology has revolutionized how healthcare providers evaluate and monitor skin mole types, improving early detection and diagnostic accuracy.
Dermoscopy (dermatoscopy) provides magnified visualization of mole structures:
Digital dermoscopy mapping offers advanced tracking:
AI-powered diagnostic tools are enhancing skin mole types evaluation:
Reflectance confocal microscopy provides cellular-level imaging:
These advanced technologies are increasingly available at specialized treatment centers, improving patient outcomes through enhanced diagnostic capabilities.
Individuals with numerous skin mole types face unique challenges in monitoring and managing their skin health. Understanding how to effectively track multiple moles while maintaining quality of life is essential.
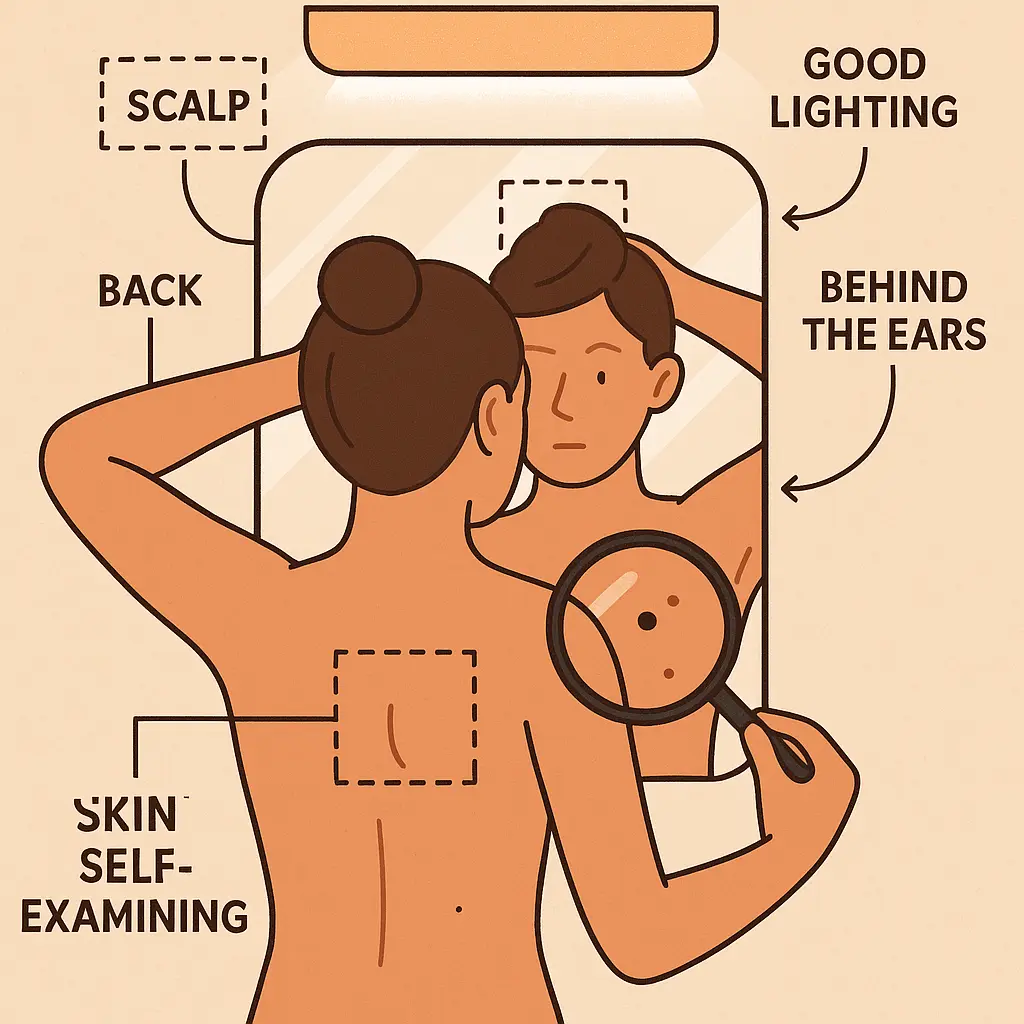
Systematic self-examination becomes crucial for people with many moles:
Emotional aspects of living with multiple moles include:
Professional support helps manage psychological aspects:
Separating fact from fiction about skin mole types helps people make informed decisions about their skin health. Many persistent myths can lead to unnecessary anxiety or dangerous neglect.
Myth: "Hairy moles are always cancerous" Truth: Hair growth from moles actually indicates healthy, functioning follicles and is generally a reassuring sign of benign behavior.
Myth: "Cutting or irritating a mole causes cancer" Truth: Physical trauma doesn't cause mole transformation to cancer, though it may reveal pre-existing concerning features.
Myth: "All dark moles are dangerous" Truth: Color alone doesn't determine malignancy; many benign skin mole types are naturally dark.
Myth: "Moles that don't hurt are safe" Truth: Most melanomas are painless in early stages; absence of symptoms doesn't guarantee safety.
Myth: "Only sun-exposed areas develop dangerous moles" Truth: Melanoma can occur anywhere on the body, including areas never exposed to sun.
Evidence-based understanding of skin mole types reveals:
Healthcare providers should address common worries by:
Different groups require tailored approaches to skin mole types monitoring and management based on unique risk factors and characteristics.
Age-related changes affect mole evaluation in older adults:
Reduced immune function significantly impacts skin mole types risk:
High UV exposure groups need specialized strategies:
Light-skinned populations face elevated risks:
Understanding these population-specific needs helps healthcare providers develop appropriate monitoring and treatment strategies.
The field of skin mole types research continues evolving, with promising developments in prevention, diagnosis, and treatment approaching clinical application.
Molecular understanding of mole development reveals:
Immune system modulation offers new treatment possibilities:
Digital health solutions expand access to specialized care:
Molecular diagnostics enhance skin mole types evaluation:
These advancing technologies promise to improve outcomes while reducing the burden of monitoring multiple skin mole types.
Creating an individualized approach to monitoring skin mole types helps ensure early detection while maintaining quality of life. Your personal plan should reflect your specific risk factors and circumstances.
Individual risk evaluation considers:
Personalized surveillance based on risk level:
Low Risk Individuals:
Moderate Risk Individuals:
High Risk Individuals:
Effective tracking includes:
Clear protocols for concerning changes:
Understanding skin mole types empowers individuals to take control of their skin health through informed monitoring and timely medical intervention. While the majority of moles remain harmless throughout life, recognizing the characteristics that distinguish benign from potentially dangerous lesions can literally save lives.
The key to effective mole management lies in balancing vigilant monitoring with realistic risk assessment. Most people can maintain excellent skin health through regular self-examinations, appropriate sun protection, and professional evaluations tailored to their individual risk factors. The ABCDE criteria provide a practical framework for identifying concerning changes, while understanding normal variations in skin mole types helps prevent unnecessary anxiety.
Modern advances in diagnostic technology, from dermoscopy to artificial intelligence, continue improving our ability to detect dangerous changes early when treatment is most effective. However, these tools complement rather than replace the fundamental importance of regular monitoring and professional evaluation.
Take action today by:
Remember that knowledge about skin mole types serves as your first line of defense against skin cancer. By staying informed, maintaining regular monitoring habits, and seeking professional guidance when needed, you can enjoy peace of mind while protecting your long-term health.
For comprehensive evaluation and treatment of concerning moles, consider consulting with specialists who can provide expert assessment and personalized monitoring strategies. Your proactive approach to understanding and monitoring skin mole types today contributes to a lifetime of healthy skin tomorrow.