When you notice tiny red or purple spots appearing on your skin that don't blanch when pressed, you might be looking at petechiae. These small, pinpoint-sized spots can appear suddenly and often cause concern, especially when you're unsure what they are or what they might indicate about your health.
Petechiae pictures serve as valuable diagnostic tools, helping both patients and healthcare professionals identify these distinctive skin manifestations. Understanding what petechiae look like, where they commonly appear, and when they signal a need for medical attention can help you make informed decisions about your health care.
• Petechiae are tiny, flat red or purple spots that measure 1-3mm in diameter and don't fade when pressure is applied • Common locations include legs, arms, face, and inside the mouth, though they can appear anywhere on the body
• Causes range from minor injuries to serious medical conditions including blood disorders, infections, and autoimmune diseases
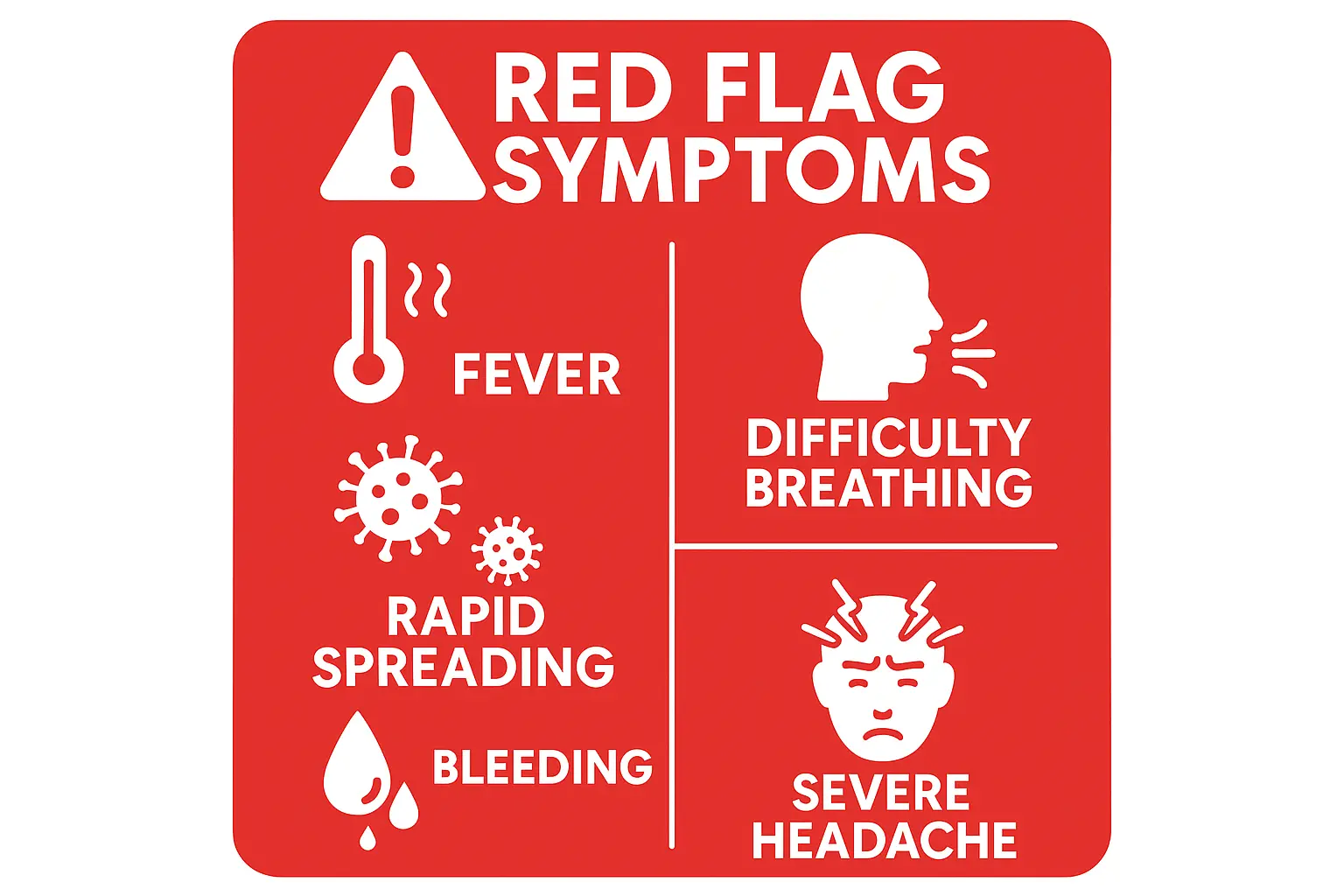
• Immediate medical attention is needed when petechiae appear with fever, difficulty breathing, or other concerning symptoms
• Professional evaluation at specialized clinics like The Minor Surgery Center can provide accurate diagnosis and appropriate treatment recommendations
Petechiae are small, flat spots that appear on the skin when tiny blood vessels called capillaries break or leak. Unlike larger bruises, these spots are typically 1-3 millimeters in diameter—about the size of a pinpoint. The name comes from the Italian word "petecchia," meaning flea bite, which gives you an idea of their small size.
Key characteristics of petechiae include:
The most distinguishing feature of petechiae is that they don't blanch—meaning they don't turn white or fade when you apply pressure. This happens because the blood has leaked out of the vessels and into the surrounding tissue, so pressing on the area doesn't affect the color.
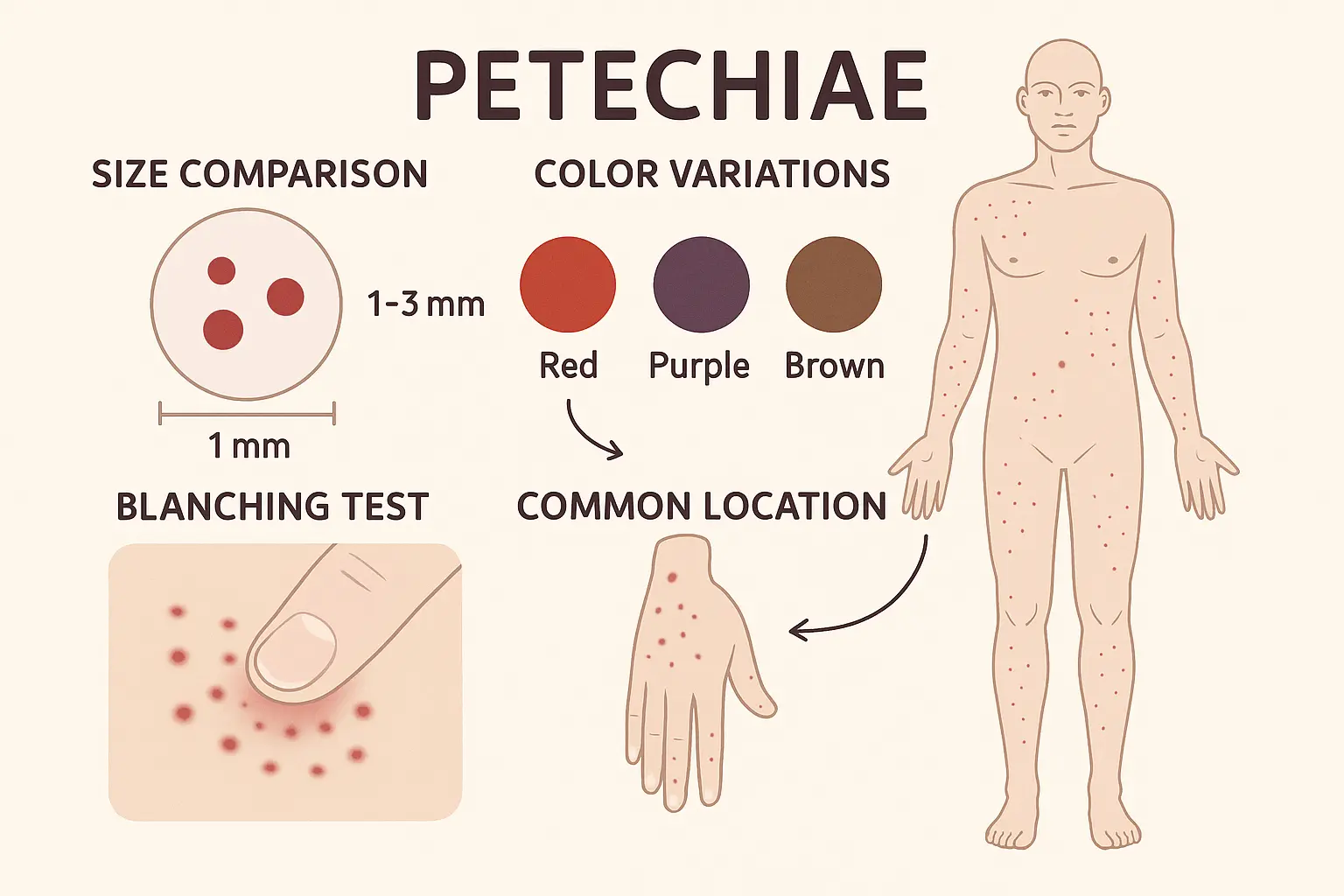
When examining petechiae pictures, you'll notice several distinctive visual features that set them apart from other skin conditions. Understanding these characteristics helps ensure accurate identification.
Petechiae maintain a remarkably consistent size range. In medical photography, they appear as:
Petechiae pictures reveal that these spots can appear differently depending on your skin tone:
On lighter skin:
On darker skin:
On olive or medium skin tones:
Petechiae pictures often show characteristic distribution patterns that can provide clues about their cause:
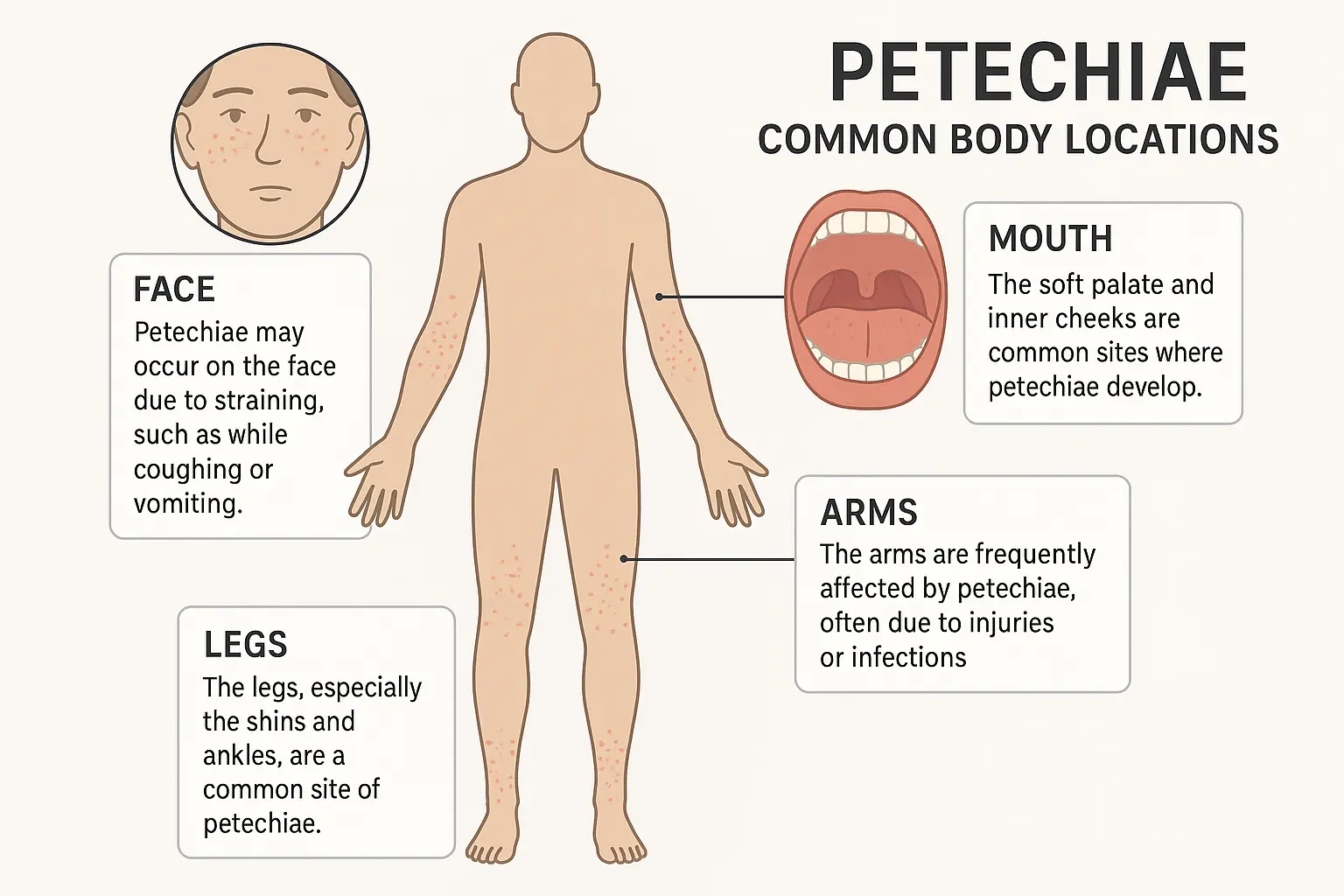
Understanding where petechiae typically develop helps you know where to look and what petechiae pictures to reference for comparison.
The legs and feet are among the most common locations for petechiae to appear:
Why legs are frequently affected:
Typical patterns on legs:
Petechiae on the upper body often indicate different underlying causes:
Arms and hands:
Face and neck:
Petechiae inside the mouth or on mucous membranes can be particularly significant:
These locations often indicate systemic conditions that affect blood clotting or platelet function.

Understanding what causes petechiae helps explain why they appear and when they might signal serious health concerns. The causes range from benign, temporary conditions to serious medical emergencies.
Many cases of petechiae result from physical pressure or trauma:
Sudden pressure increases:
External pressure:
Several health conditions can cause petechiae to develop:
Blood-related disorders:
Infections:
Autoimmune conditions:
Other medical causes:
Some medications can increase the risk of petechiae formation:
Petechiae can affect people of all ages, but the appearance, causes, and significance often vary by age group.
In pediatric patients, petechiae pictures often show:
Common childhood causes:
Concerning signs in children:
When to seek immediate care: Children with petechiae should be evaluated promptly, especially if accompanied by other symptoms, as they may indicate serious conditions like leukemia or other blood disorders.
Adult petechiae pictures typically show:
Common adult causes:
Gender differences:
In older adults, petechiae may appear more frequently due to:
While many cases of petechiae are benign, certain presentations require immediate medical attention. Learning to recognize these warning signs can be life-saving.
Seek emergency medical care when petechiae appear with:
Systemic symptoms:
Bleeding symptoms:
Rapid progression:
Several serious medical conditions can present with petechiae:
Meningococcal disease:
Thrombotic thrombocytopenic purpura (TTP):
Acute leukemia:
When petechiae appear, professional medical evaluation is often necessary to determine the underlying cause and appropriate treatment. Understanding what to expect during this process can help you prepare and ensure you receive the best care.
A thorough evaluation typically includes:
Medical history review:
Physical examination:
Vital signs and general assessment:
Depending on the initial assessment, your healthcare provider may order:
Blood tests:
Specialized tests:
Imaging studies:
For comprehensive evaluation and treatment, consider visiting specialized medical facilities. The Minor Surgery Center provides expert assessment of skin conditions and can help determine when petechiae require further investigation or treatment.
Benefits of specialized evaluation:
Treatment for petechiae depends entirely on the underlying cause. Understanding various treatment approaches helps set appropriate expectations for recovery.
Blood disorder treatments:
Infection management:
Medication adjustments:
While addressing the underlying cause, supportive measures can help:
Skin protection:
Activity modifications:
Monitoring and follow-up:
For cases with benign causes, home care focuses on:
General measures:
When to seek additional care:
While not all cases of petechiae can be prevented, understanding risk factors and implementing preventive strategies can reduce your likelihood of developing these skin manifestations.
Physical activity considerations:
Clothing and accessories:
General health maintenance:
Medication management:
Regular health monitoring:
Infection prevention:
Be especially vigilant about petechiae development during:
Times of illness:
Medication changes:
Life transitions:
Some individuals experience recurring episodes of petechiae due to chronic conditions or ongoing risk factors. Learning to manage this condition effectively can improve quality of life and reduce anxiety.
Keeping detailed records:
Communication with healthcare providers:
Dealing with anxiety:
Building confidence:
Social and professional life:
Long-term planning:
For ongoing support and expert care, consider establishing a relationship with specialized healthcare providers. Our team at The Minor Surgery Center understands the concerns that come with unexplained skin changes and can provide the expert evaluation and peace of mind you deserve.
The key distinguishing feature is the blanching test—petechiae won't disappear when you press on them, while many other red spots will temporarily fade with pressure. Petechiae are also consistently small (1-3mm), flat, and have well-defined borders.
Not necessarily. Many cases result from minor causes like coughing, physical exertion, or tight clothing. However, petechiae can also indicate serious conditions, so medical evaluation is important, especially when accompanied by other symptoms.
The duration depends on the cause. Petechiae from minor trauma or pressure may fade within a few days to weeks. Those caused by medical conditions may persist until the underlying issue is treated.
While not all cases are preventable, you can reduce risk by avoiding tight clothing, managing chronic conditions properly, taking medications as prescribed, and seeking prompt treatment for infections.
Document petechiae when they first appear, especially if they're spreading or accompanied by other symptoms. Take clear, well-lit photos that show the size, color, and distribution of the spots.
If you have concerns about skin changes or need professional evaluation, contact us to schedule an appointment. Our experienced team can provide the expert assessment and peace of mind you need.
Understanding petechiae pictures and their significance empowers you to make informed decisions about your health. While these tiny red spots can appear alarming, knowing how to identify them, when they require immediate attention, and what causes them helps you respond appropriately.
Remember that petechiae can range from benign, temporary manifestations to signs of serious medical conditions. The key is recognizing when professional evaluation is needed and seeking care promptly when concerning symptoms develop.
Your next steps should include:
• Monitoring any existing petechiae for changes in size, number, or associated symptoms • Seeking medical evaluation if petechiae appear with fever, bleeding, or other concerning signs • Documenting new occurrences with photos and detailed notes about timing and potential triggers • Maintaining open communication with healthcare providers about any skin changes or health concerns
For expert evaluation of skin conditions and professional medical guidance, visit our clinic where our experienced team provides comprehensive care in a comfortable, patient-focused environment. We're here to help you understand your symptoms and receive the appropriate care you need.
Don't let uncertainty about skin changes cause unnecessary worry. With proper knowledge and professional support, you can confidently manage your health and seek appropriate care when needed. Your skin health matters, and expert care is always available when you need it.