Understanding what nodular melanoma looks like through pictures and real examples could be the difference between early detection and a life-threatening situation. Unlike other types of melanoma that spread outward across the skin's surface, nodular melanoma grows downward into deeper layers of skin, making early recognition absolutely critical.
• Nodular melanoma appears as raised, dome-shaped bumps that are often black, blue, or red, and can develop quickly over weeks or months
• The traditional ABCDE rule doesn't always apply to nodular melanoma, making it harder to identify using standard melanoma detection methods
• Any new, changing, or unusual raised lesion should be examined by a medical professional immediately, especially if it bleeds, itches, or grows rapidly
• Early detection is crucial because nodular melanoma can penetrate deeper into the skin faster than other melanoma types
• Professional evaluation at specialized centers like The Minor Surgery Center can provide expert assessment and treatment options
Nodular melanoma represents about 10-15% of all melanomas, but it's responsible for a disproportionate number of melanoma-related deaths. This type of skin cancer doesn't follow the typical rules that most people learn about spotting melanoma.
While superficial spreading melanoma—the most common type—grows outward across the skin's surface before penetrating deeper, nodular melanoma takes a different approach. It grows vertically from the start, diving deep into the skin layers like a dangerous iceberg.
Rapid Growth 🚨
Nodular melanoma can develop and change within weeks to months, not years like other melanomas.
Raised Appearance
These lesions are typically elevated above the skin surface, appearing as bumps, nodules, or dome-shaped growths.
Uniform Color
Unlike other melanomas that often show multiple colors, nodular melanomas frequently appear as a single color—usually black, blue, red, or even pink.
Smooth Surface
The surface is often smooth and may be shiny or glossy in appearance.

When examining nodular melanoma pictures, several distinct visual patterns emerge that set this cancer apart from other skin lesions.
The most recognizable form appears as a dark black or blue-black raised bump. These lesions often look like:
In pictures, these classic presentations show a clear contrast against normal skin, with well-defined borders and a distinctly raised profile.
Perhaps more concerning because they're often overlooked, amelanotic (non-pigmented) nodular melanomas appear as:
These are particularly dangerous because they don't fit the typical "dark mole" image most people associate with melanoma.
Some nodular melanomas display:
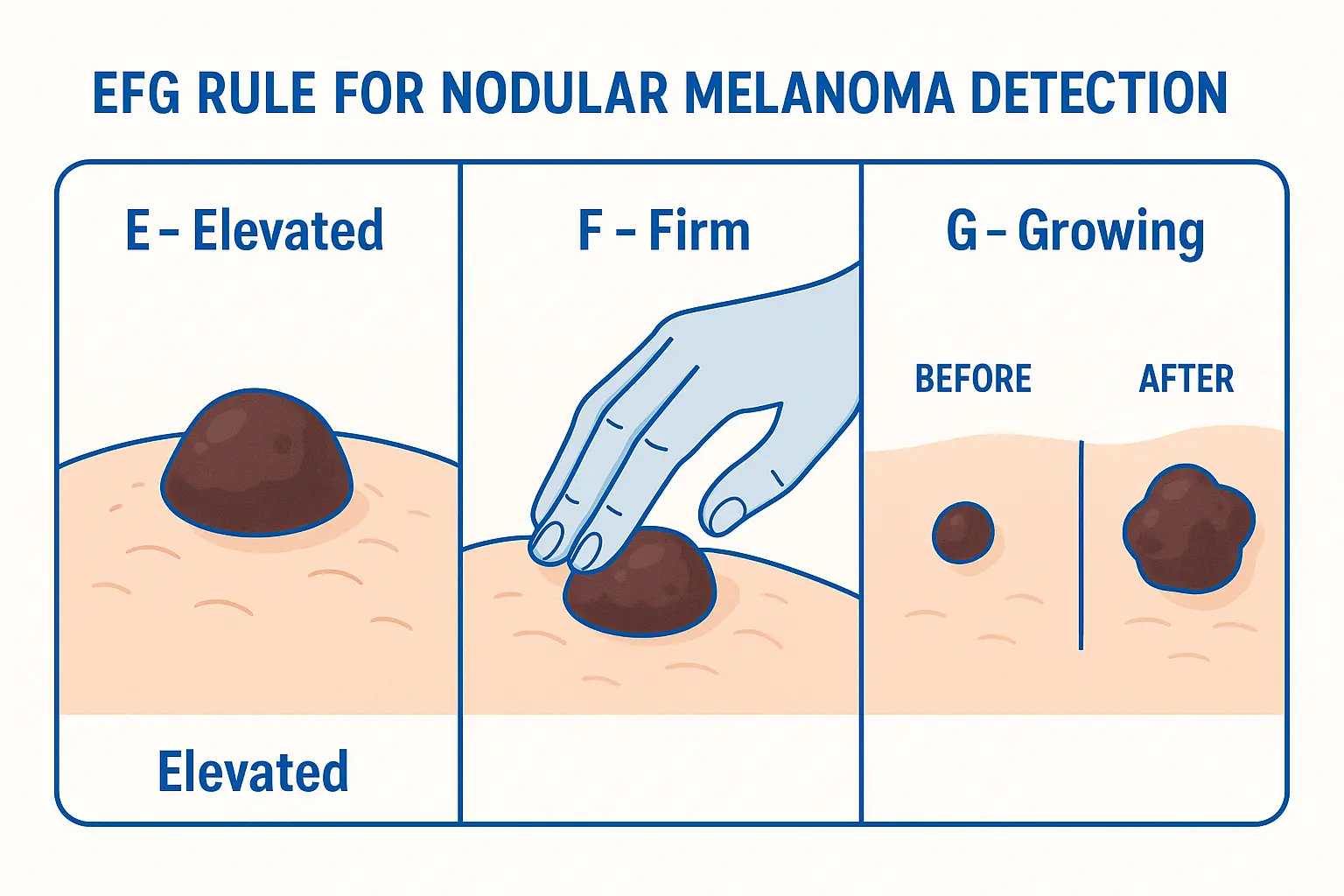
Traditional melanoma detection relies on the ABCDE rule (Asymmetry, Border, Color, Diameter, Evolution), but this method often fails with nodular melanoma. Instead, dermatologists recommend the EFG rule specifically for nodular melanoma:
The lesion is raised above the skin surface. Any new bump or nodule that wasn't there before deserves attention.
When you touch it (gently), the lesion feels firm or hard compared to surrounding skin.
The lesion is growing progressively over weeks or months. This rapid change is a red flag.
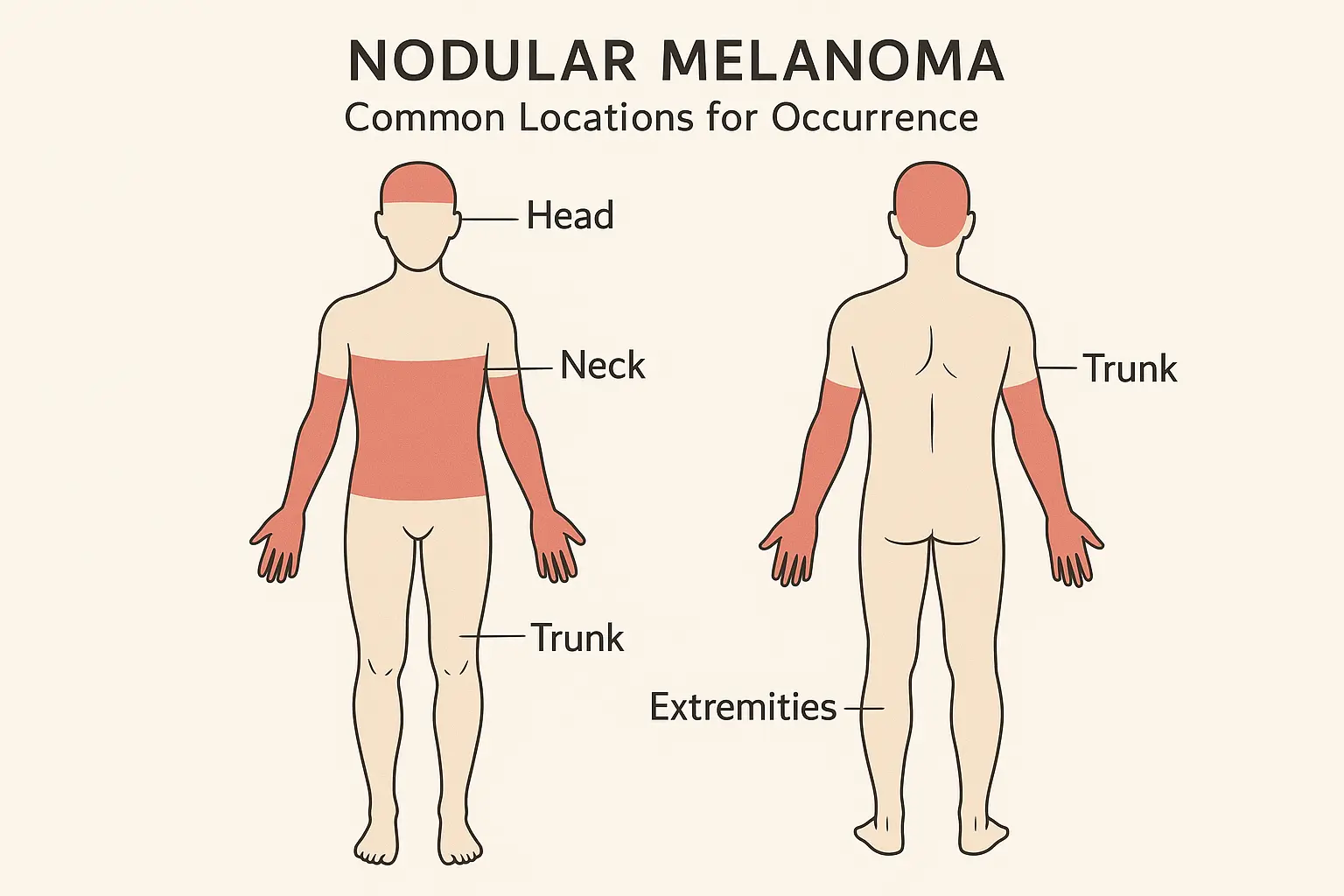
Nodular melanoma pictures reveal that these cancers can appear anywhere on the body, but certain locations are more common:
Head and Neck Region
Trunk
Extremities
Men tend to develop nodular melanoma more frequently on:
Women more commonly see nodular melanoma on:
When studying nodular melanoma pictures across different demographics, certain patterns emerge:
Older Adults (50+)
Younger Adults
Sun Damage History Pictures from patients with significant sun exposure often show nodular melanomas surrounded by other sun damage signs like age spots and wrinkles.
Fair Skin Light-skinned individuals may show more contrast between the melanoma and surrounding skin in pictures.
Previous Melanoma Subsequent nodular melanomas may appear different from the original cancer.
Certain visual characteristics in nodular melanoma pictures indicate the need for urgent medical evaluation:
Rapid Changes
Bleeding or Oozing
Pain or Sensation Changes
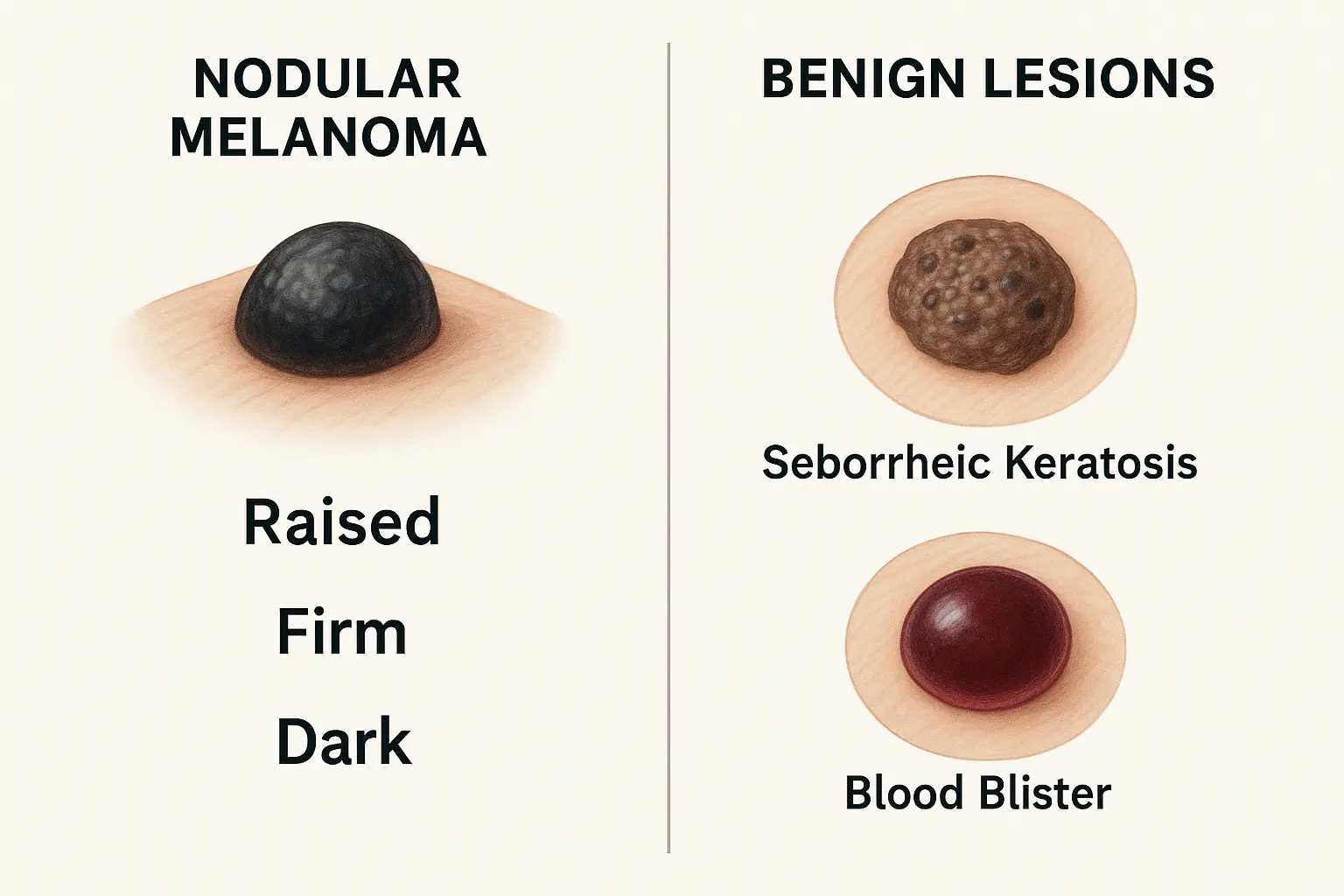
Understanding the difference between nodular melanoma and harmless skin growths is crucial for proper identification.
FeatureNodular MelanomaSeborrheic KeratosisSurfaceSmooth, often shinyRough, "stuck-on" appearanceGrowth RateRapid (weeks/months)Very slow (years)ColorUniform dark or redBrown, often mottledFeelFirm, hardSoft, waxy
Blood Blisters:
Nodular Melanoma:
Normal Mole Evolution:
Nodular Melanoma Development:
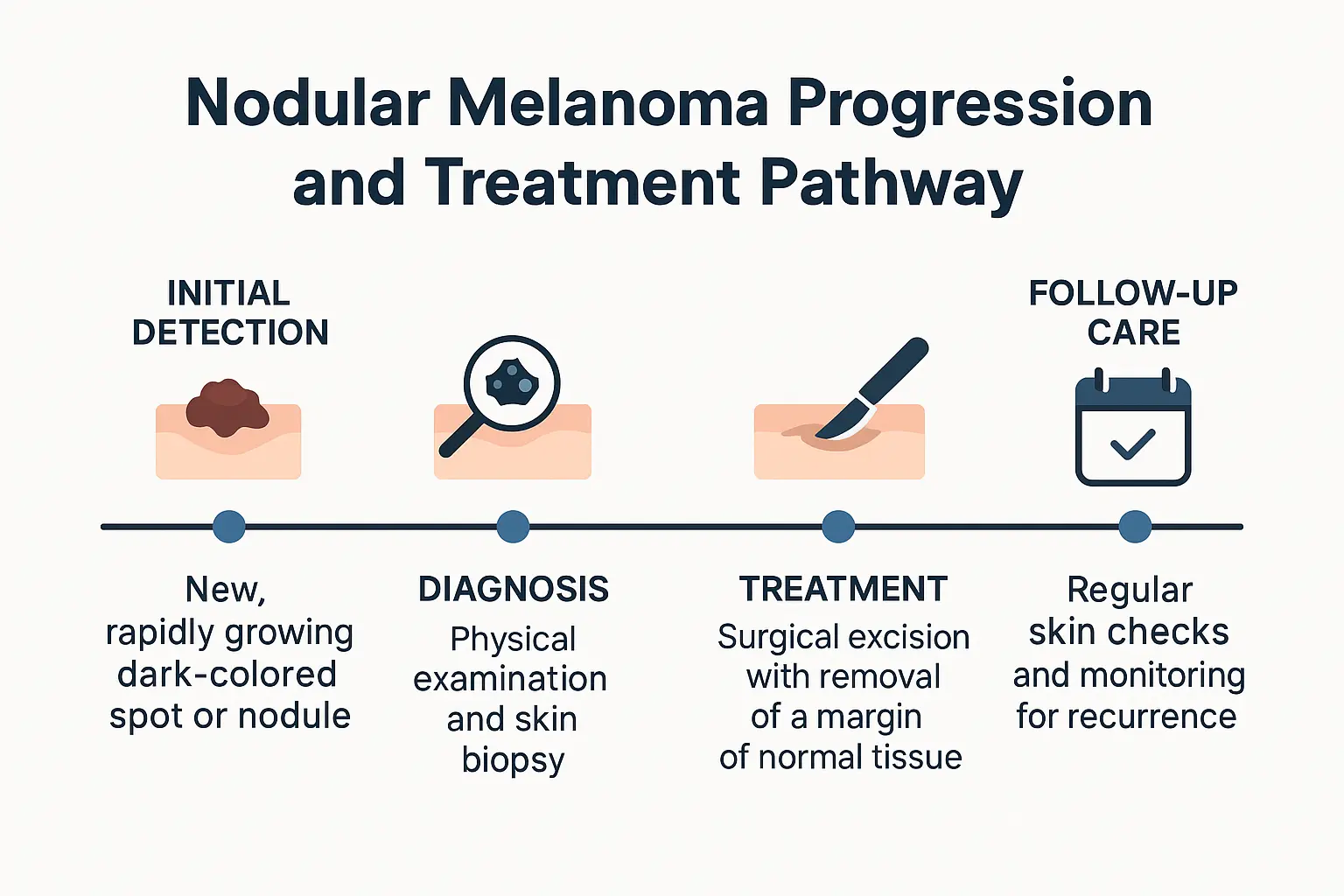
While nodular melanoma pictures can help with initial recognition, nothing replaces professional medical evaluation. The subtle differences between cancerous and benign lesions require trained expertise.
Visual Examination Your doctor will examine the lesion under proper lighting and may use magnification tools.
Dermoscopy A special magnifying device called a dermatoscope allows detailed examination of skin structures not visible to the naked eye.
Photography Documentation Medical photography helps track changes over time and aids in diagnosis.
Biopsy Consideration If there's any suspicion of melanoma, a biopsy will be recommended for definitive diagnosis.
At The Minor Surgery Center, our experienced team specializes in the evaluation and treatment of suspicious skin lesions. We understand that discovering a concerning bump or mole can be anxiety-provoking, which is why we prioritize quick, thorough assessments in a comfortable environment.
When nodular melanoma is confirmed through biopsy, prompt treatment is essential. The specific approach depends on several factors including the thickness of the melanoma, its location, and whether it has spread.
Wide Local Excision This is the primary treatment for nodular melanoma, involving:
Sentinel Lymph Node Biopsy For thicker melanomas, doctors may recommend:
Immunotherapy For advanced nodular melanoma:
Targeted Therapy For melanomas with specific genetic mutations:
Our team at The Minor Surgery Center works closely with oncology specialists to ensure comprehensive care when advanced treatments are needed.
While studying nodular melanoma pictures is valuable for recognition, prevention remains the best strategy against this aggressive cancer.
Daily Sunscreen Use ☀️
Protective Clothing
Seek Shade
Monthly Skin Checks Perform thorough self-examinations monthly:
Partner Assistance Have a partner or family member help examine hard-to-see areas like your back and scalp.
Annual Dermatology Visits
Know Your Risk Level Higher-risk individuals may need more frequent screenings:
For individuals diagnosed with nodular melanoma, ongoing care extends beyond initial treatment.
First Two Years
Years 3-5
Lifelong Monitoring
Dealing with Anxiety A melanoma diagnosis can create lasting anxiety about cancer recurrence:
Family Considerations Melanoma can have genetic components:
Advances in technology are improving our ability to detect and analyze suspicious lesions.
Machine Learning Applications
Smartphone Apps While not replacements for professional evaluation:
Confocal Microscopy
Optical Coherence Tomography
When facing a potential melanoma diagnosis, choosing the right healthcare provider makes a significant difference in outcomes and experience.
Expertise in Skin Cancer Specialized centers offer:
Comprehensive Services
At The Minor Surgery Center, we've designed our practice specifically to address the needs of patients with skin concerns. Our approach combines medical expertise with compassionate care, ensuring that you receive both excellent treatment and emotional support throughout your journey.
Rapid Access
Clear Communication
Coordinated Treatment
For questions about our services or to schedule a consultation, visit our contact page or explore our frequently asked questions.
The field of melanoma research continues to evolve, offering hope for better detection and treatment options.
Genetic Testing
Biomarker Research
Improved Immunotherapies
Precision Medicine
Knowledge about nodular melanoma pictures and characteristics is most valuable when combined with a concrete action plan.
Risk Assessment
Lifestyle Modifications
Healthcare Relationships
Understanding nodular melanoma through pictures and clinical descriptions empowers you to recognize potentially dangerous skin changes early. Unlike other forms of melanoma, nodular melanoma's rapid growth and deep penetration make early detection absolutely critical for successful treatment.
The key points to remember are that nodular melanoma often appears as a raised, firm bump that grows quickly over weeks to months. It may be black, blue, red, or even pink, and doesn't always follow traditional melanoma warning signs. The EFG rule—Elevated, Firm, and Growing—provides a more effective detection framework for this aggressive cancer type.
Your next steps should include:
• Schedule a professional skin examination if you have any concerning lesions • Begin regular self-examinations to monitor for new or changing spots • Implement daily sun protection to reduce your risk of developing melanoma • Stay informed about advances in detection and treatment
Remember, when it comes to skin cancer, early action saves lives. Any new, changing, or unusual skin growth deserves professional evaluation. Don't wait or hope it will go away—your health and peace of mind are worth the investment in proper medical care.
If you're concerned about a skin lesion or want to establish care with melanoma specialists, The Minor Surgery Center provides expert evaluation and treatment in a comfortable, patient-focused environment. Our team understands that skin cancer concerns can be frightening, and we're here to provide both excellent medical care and the support you need during this important health decision.
For more information about our services and to take the first step toward protecting your skin health, explore our comprehensive resources or contact us directly to schedule your consultation.