You might think melanoma only appears on sun-exposed skin, but nail apparatus melanoma (NAM) is a hidden threat that often goes unnoticed until it reaches advanced stages. This rare subtype of melanoma develops beneath or around your nails, masquerading as harmless discoloration or injury. The stakes are high: early detection can mean the difference between a simple surgical procedure and extensive treatment involving amputation.
In 2025, advances in diagnostic technology and surgical techniques are transforming how we approach this condition. Whether you're a patient who's noticed suspicious nail changes or simply want to understand this complex condition, this comprehensive guide will walk you through everything you need to know about nail apparatus melanoma—from recognizing early warning signs to understanding cutting-edge treatment options.
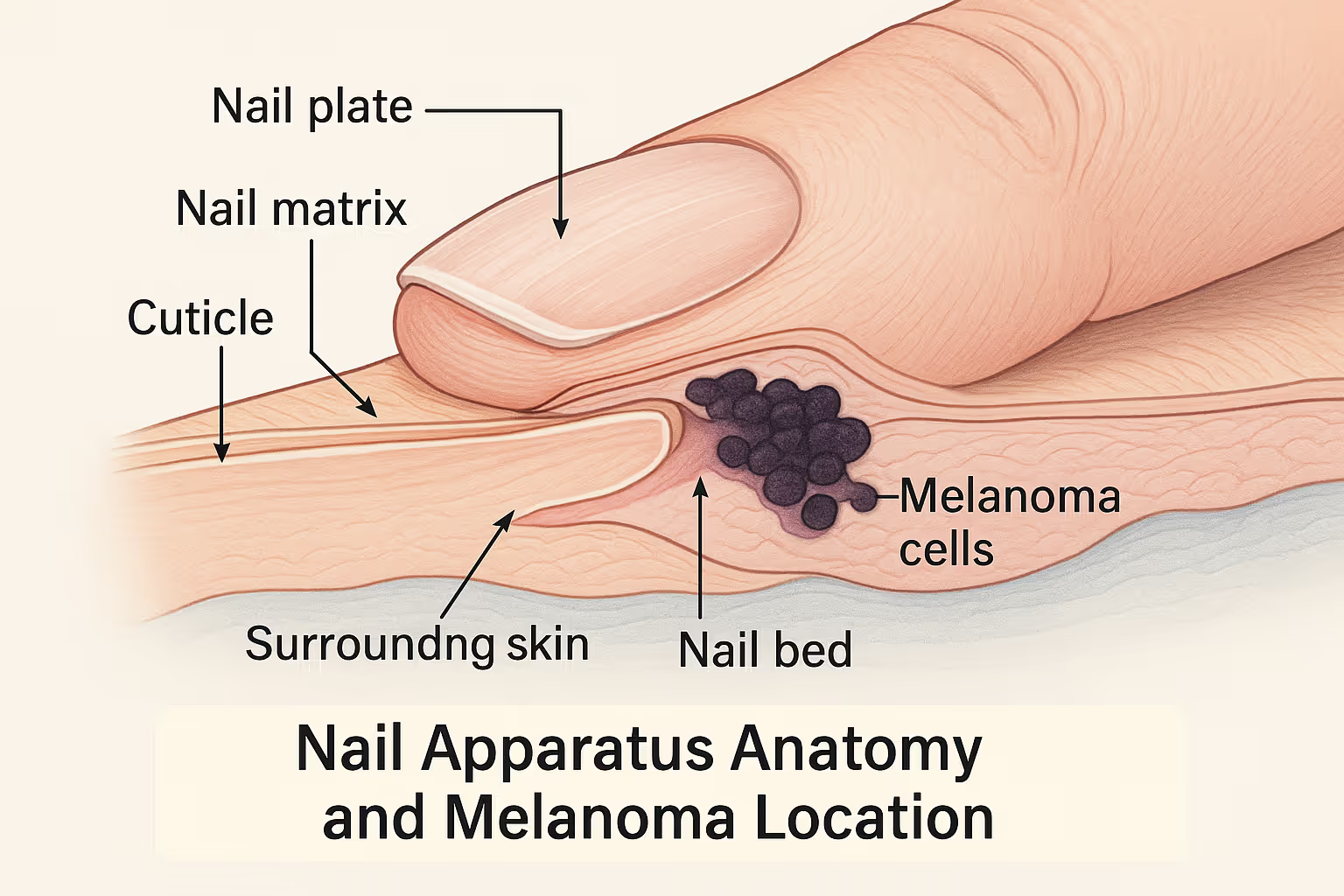
Nail apparatus melanoma develops in the melanocytes—pigment-producing cells—located in the nail matrix, nail bed, or surrounding skin. Unlike melanomas that appear on your arms or back, NAM hides beneath the protective covering of your nail plate, making it incredibly difficult to spot in its early stages.
Here's what makes NAM particularly challenging:
The nail apparatus consists of several components: the nail matrix (where nail growth begins), the nail bed (tissue beneath the nail plate), the nail plate itself, and the surrounding folds of skin. Melanoma can arise in any of these structures, though it most commonly originates in the nail matrix.
While anyone can develop nail apparatus melanoma, certain factors increase your risk:
Demographics and Risk Factors:
Risk FactorDetailsAgeMost common in people aged 50-70 yearsEthnicityHigher proportional incidence in Asian, African, and Hispanic populationsLocationThumb and big toe account for 75-90% of casesPrevious traumaHistory of nail injury may increase risk, though connection remains controversialGenetic factorsFamily history of melanoma increases overall riskRadiation exposurePrevious radiation treatment to hands or feet
It's crucial to understand that nail apparatus melanoma doesn't follow the same sun-exposure pattern as cutaneous melanoma. You won't prevent it by applying sunscreen to your nails. Instead, vigilance and early recognition of suspicious changes are your best defense.
Early detection dramatically improves outcomes for nail apparatus melanoma. That's why understanding the warning signs is so important—for you, your loved ones, and even your healthcare providers.
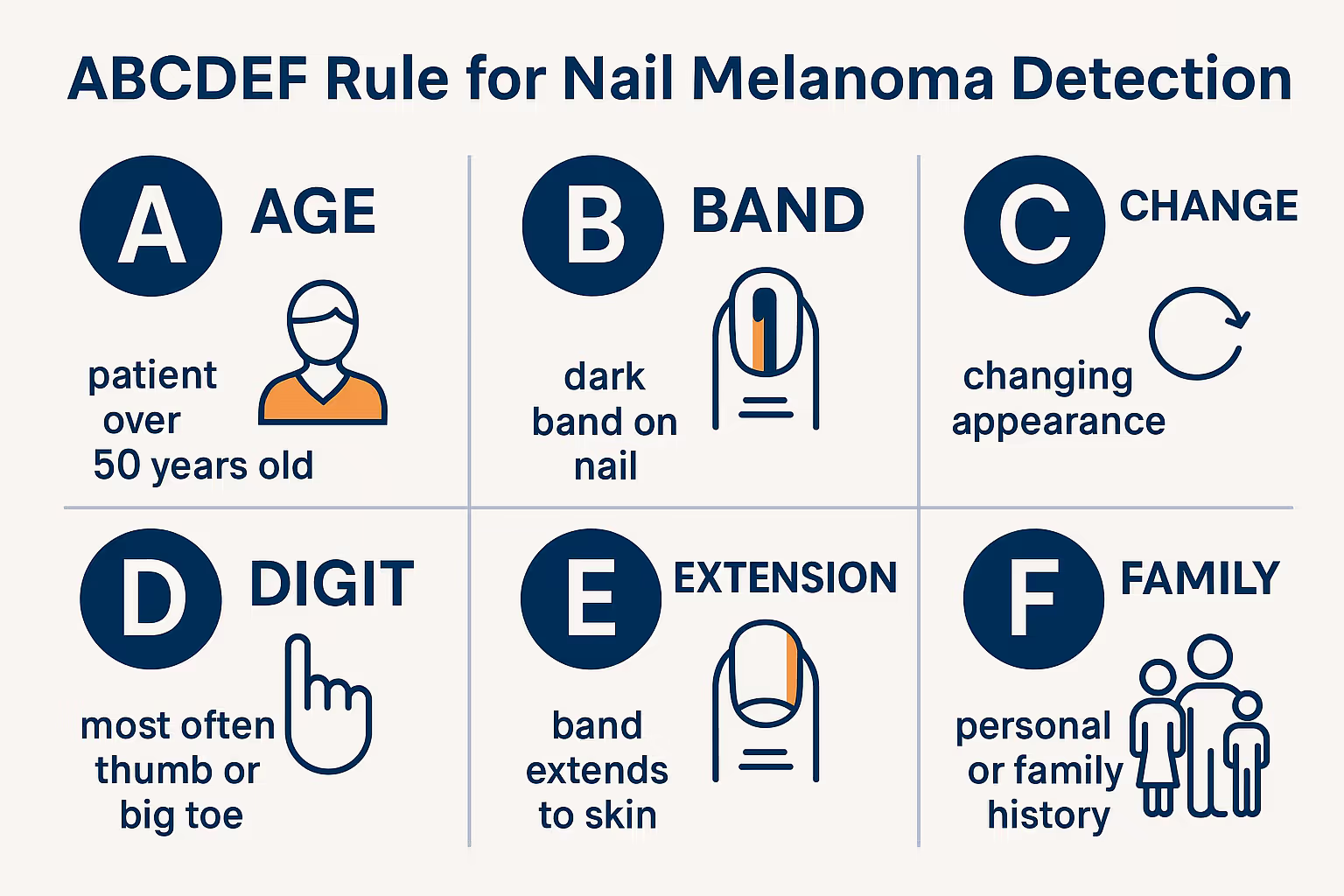
Medical professionals use the ABCDEF criteria to evaluate suspicious nail pigmentation:
A - Age and Ancestry
B - Band (Brown-Black)
C - Change
D - Digit
E - Extension
F - Family or Personal History
"Hutchinson's sign—pigmentation spreading beyond the nail onto the surrounding skin—should always prompt immediate medical evaluation. It's not something to watch and wait on." — Expert consensus from dermatologic oncology
Pay attention to these additional warning signs:
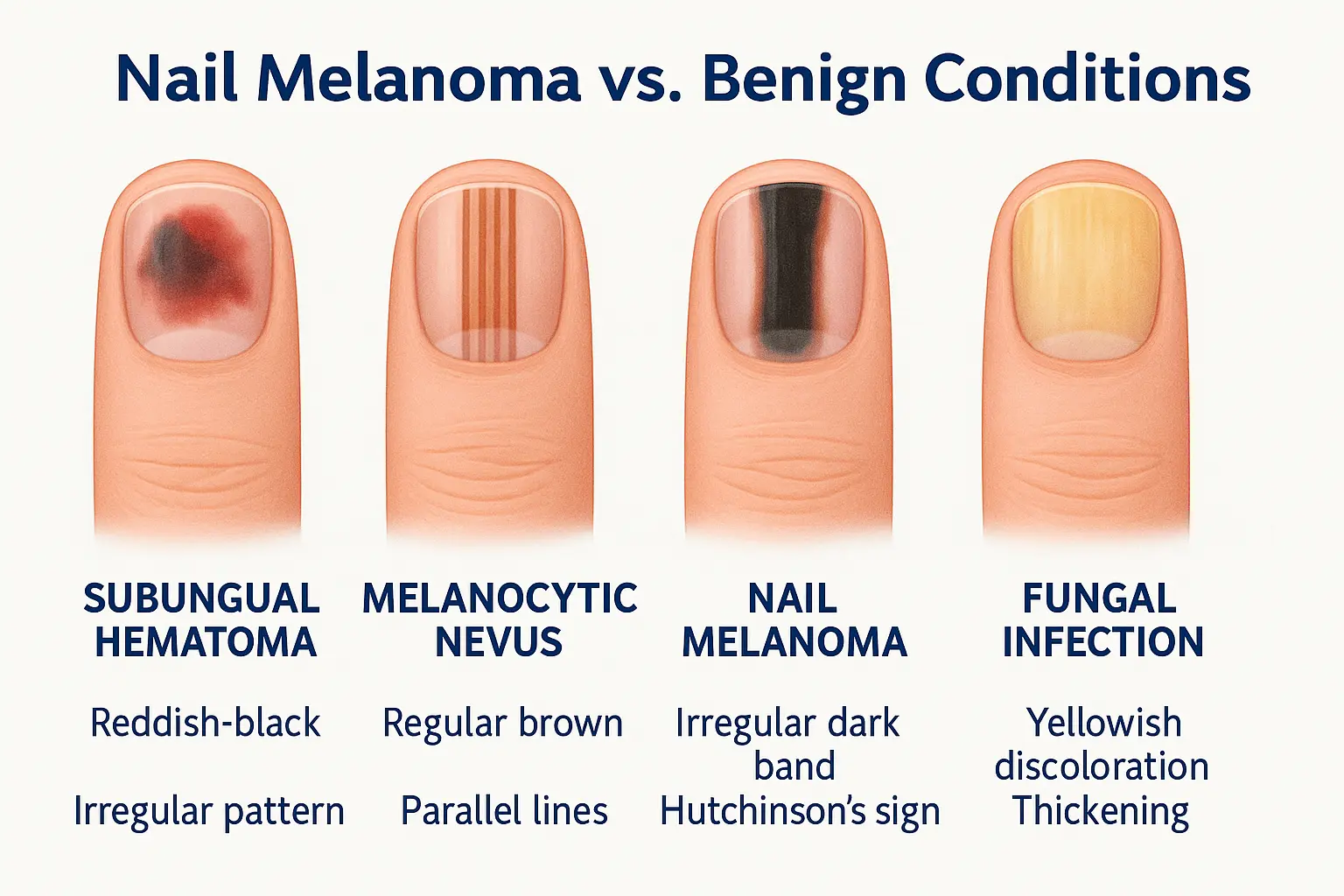
Not every dark streak on your nail is melanoma. In fact, most aren't. Benign conditions like subungual hematoma (blood under the nail), fungal infections, and melanocytic nevi are far more common. However, when in doubt, get it checked out. The Minor Surgery Center specializes in evaluating and treating concerning skin lesions, including those affecting the nail apparatus.
One of the greatest challenges in managing nail apparatus melanoma is distinguishing it from benign conditions that look remarkably similar. Understanding these lookalikes helps explain why diagnosis can be so challenging.
1. Subungual Hematoma (Blood Under the Nail)
2. Melanocytic Nevus (Mole)
3. Onychomycosis (Fungal Infection)
4. Subungual Bowen's Disease
5. Onychopapilloma
6. Drug-Induced Melanonychia
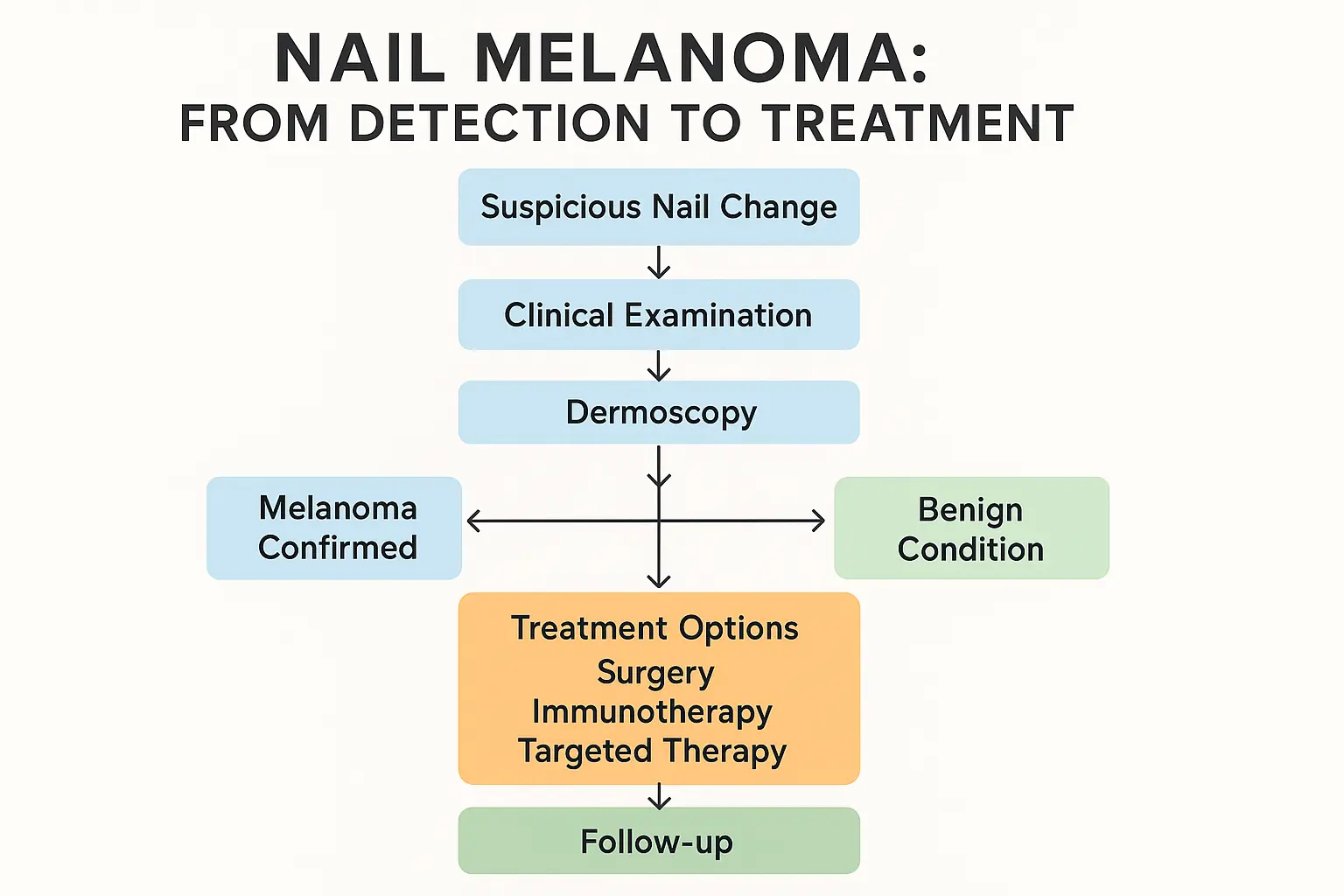
Dermoscopy—examination using a specialized magnifying device—has revolutionized the evaluation of nail pigmentation. This non-invasive technique allows your doctor to see patterns invisible to the naked eye.
Key dermoscopic features suggesting melanoma:
Benign conditions typically show more regular patterns with evenly spaced, parallel lines and consistent coloration. However, dermoscopy alone cannot definitively rule out melanoma—when suspicion is high, biopsy remains essential.
For concerning skin changes anywhere on your body, including nails, our experienced team can provide expert evaluation and guidance on next steps.
Diagnosing nail apparatus melanoma requires a systematic approach combining clinical examination, imaging, and histopathological confirmation. Here's how the diagnostic journey typically unfolds.
Your doctor will begin with a thorough history and physical examination:
History Questions:
Physical Examination:
Modern diagnostic approaches incorporate several imaging techniques:
Dermoscopy
Reflectance Confocal Microscopy (RCM)
Optical Coherence Tomography (OCT)
When clinical and dermoscopic findings raise suspicion for melanoma, biopsy is essential. However, nail biopsies are technically challenging and should be performed by experienced practitioners.
Biopsy Techniques:
TechniqueWhen UsedAdvantagesDisadvantagesNail matrix biopsySuspected matrix melanomaDirect sampling of origin siteRisk of permanent nail dystrophyNail bed biopsyPigmentation visible after plate removalGood tissue sampleRequires nail plate removalExcisional biopsyHigh suspicion, small lesionComplete removal, definitive diagnosisMore invasive, potential functional impactPunch biopsyLower suspicion, diagnostic uncertaintyLess invasive, preserves functionMay miss diagnosis if sampling error
The biopsy should include adequate depth to assess invasion and should be performed in a way that preserves nail function when possible. At The Minor Surgery Center, procedures are performed with precision and attention to both diagnostic accuracy and cosmetic outcomes.
Once tissue is obtained, a dermatopathologist examines it under the microscope to determine:
Immunohistochemistry (special staining techniques) may be used to confirm the diagnosis, particularly in challenging cases. Markers like S100, SOX10, Melan-A, and HMB-45 help identify melanocytic cells.
If melanoma is confirmed, staging determines the extent of disease and guides treatment:
Local Assessment:
Imaging for Advanced Disease:
Staging follows the American Joint Committee on Cancer (AJCC) TNM system, which considers tumor thickness, nodal involvement, and metastases.
Treatment for nail apparatus melanoma has evolved significantly over the past decade. The approach depends on the stage at diagnosis, tumor characteristics, and patient factors. Let's break down the current treatment options.
Surgery remains the primary treatment for localized nail apparatus melanoma. The goal is complete tumor removal with adequate margins while preserving as much function as possible.
Margin Recommendations:
Breslow ThicknessRecommended MarginIn situ (confined to epidermis)5-10 mm≤1.0 mm1 cm1.01-2.0 mm1-2 cm>2.0 mm2 cm
For nail apparatus melanoma, achieving these margins often requires:
Digit-Preserving Surgery:
Amputation:
"The decision between digit preservation and amputation requires careful consideration of tumor extent, functional outcomes, and patient preferences. When possible, we aim to preserve function without compromising oncologic outcomes." — Surgical oncology perspective
Mohs Micrographic Surgery:
An emerging approach for select cases of nail apparatus melanoma:
For melanomas >1mm thick or with high-risk features (ulceration, high mitotic rate), sentinel lymph node biopsy is recommended:
The Procedure:
Controversy and Evolution:
Recent studies (MSLT-II trial) showed that completion lymph node dissection (removing all regional nodes) after positive SLNB doesn't improve survival compared to observation with ultrasound surveillance. This has shifted practice toward more conservative lymph node management.
For patients with high-risk melanoma (stage IIB-IV), adjuvant therapy after surgery reduces the risk of recurrence and improves survival.
Pembrolizumab (Keytruda)
Nivolumab (Opdivo)
How They Work: These medications release the "brakes" on your immune system, allowing it to recognize and attack melanoma cells more effectively.
Common Side Effects:
Most side effects are manageable, but immune-related adverse events require prompt recognition and treatment.
For melanomas with BRAF V600 mutations (found in about 50% of cutaneous melanomas):
Combination Therapy:
These combinations target specific genetic mutations driving melanoma growth.
Important Notes:
For stage IV melanoma (distant metastases), treatment has been revolutionized by immunotherapy and targeted therapy:
First-Line Options:
Response Rates in 2025: Modern therapies achieve objective response rates of 40-60%, with some patients experiencing durable complete responses lasting years.
Radiation Therapy:
For comprehensive evaluation and treatment of skin concerns, including suspicious lesions that require expert care, explore our services designed to provide accessible, expert surgical care.
Prognosis for nail apparatus melanoma depends heavily on the stage at diagnosis. Let's look at the survival data and factors that influence outcomes.
Five-Year Survival Rates (Approximate):
StageDescription5-Year SurvivalStage 0In situ (confined to epidermis)~99%Stage IThin melanoma, no spread90-95%Stage IIThicker melanoma, no spread65-90%Stage IIIRegional lymph node involvement40-70%Stage IVDistant metastases15-30%
Important Context: These numbers represent historical data and don't fully reflect the impact of modern immunotherapy and targeted therapy, which have significantly improved outcomes for advanced disease since 2015.
Several factors influence prognosis:
Tumor Characteristics:
Patient Factors:
Treatment-Related Factors:
Unfortunately, nail apparatus melanoma is often diagnosed at more advanced stages compared to cutaneous melanoma:
This underscores the critical importance of awareness, early recognition, and prompt evaluation of suspicious nail changes.
After treatment, regular follow-up is essential:
Surveillance Schedule:
What Follow-Up Includes:
Recurrence Patterns:
If you have questions about follow-up care or need guidance on concerning changes, our team is here to help provide clarity and expert evaluation.
The field of melanoma treatment is rapidly evolving. Here are the most promising developments that may change how we manage nail apparatus melanoma in the coming years.
Artificial Intelligence and Machine Learning
Molecular Diagnostics
Enhanced Imaging
Oncolytic Virus Therapy
Cellular Therapies
Next-Generation Immunotherapy
Targeted Therapy Advances
The future of melanoma treatment is increasingly personalized:
Genomic Profiling:
Predictive Biomarkers:
Response Monitoring:
Minimally Invasive Techniques:
Intraoperative Imaging:
Screening Programs:
Public Awareness:
Risk Stratification:
Numerous clinical trials are currently investigating:
Participating in clinical trials may provide access to cutting-edge treatments while advancing scientific knowledge. Ask your oncologist about appropriate trials for your situation.
A diagnosis of nail apparatus melanoma brings not only medical challenges but also emotional, functional, and practical considerations. Here's guidance for navigating life during and after treatment.
Receiving a melanoma diagnosis is overwhelming. Here are strategies that help:
Emotional Support:
Practical Steps:
Trusted Resources:
Different treatments come with different challenges:
Surgical Recovery:
Immunotherapy Side Effects:
Targeted Therapy Side Effects:
Amputation or extensive surgery may require adjustments:
Occupational Therapy:
Prosthetics:
Psychological Adjustment:
After treatment, you play a crucial role in monitoring for recurrence:
Self-Examination:
What to Report Immediately:
Sun Protection: While nail melanoma isn't caused by sun exposure, protecting your skin from UV damage reduces risk of other skin cancers:
While no specific diet prevents melanoma recurrence, healthy lifestyle choices support overall health:
Nutrition:
Physical Activity:
Stress Management:
For any concerning skin changes or questions about minor surgical procedures, reach out to our team for compassionate, expert guidance.
Yes, when caught early. In situ melanoma (confined to the top layer) has a cure rate near 99%. Even invasive melanomas have excellent cure rates when diagnosed at stage I or II. The key is early detection and appropriate treatment.
Sometimes nail plate removal (avulsion) is necessary to visualize the underlying nail bed and matrix. This allows better examination and, if needed, biopsy. The nail will regrow, though it may take 4-6 months.
Not necessarily. Many nail melanomas can be treated with digit-preserving surgery, especially when caught early. Amputation is reserved for cases where adequate margins cannot be achieved otherwise or when the tumor extensively involves bone or other structures.
The biology is similar, but the location creates unique challenges. Nail melanoma is hidden beneath the nail plate, making early detection difficult. It's also more common in people with darker skin tones, where it represents a higher proportion of all melanomas.
There's no strong evidence that nail polish or gel manicures cause melanoma. However, nail polish can hide suspicious changes, and UV lamps used for gel nails expose skin to UV radiation (though the cancer risk appears very low). If you have a suspicious nail change, remove polish for medical evaluation.
Start with a dermatologist for evaluation. If melanoma is suspected or confirmed, you'll likely be referred to a surgical oncologist or Mohs surgeon for definitive treatment. A multidisciplinary approach often provides the best outcomes.
Nail lesions can be challenging to diagnose pathologically. If the diagnosis is uncertain, options include:
Yes, melanoma can recur. That's why regular follow-up is essential. Recurrence risk depends on the original stage—higher stage disease has greater recurrence risk. Modern adjuvant therapies significantly reduce recurrence rates.
While most cases aren't inherited, having a family history of melanoma increases your risk. Genetic syndromes like familial atypical multiple mole melanoma (FAMMM) syndrome increase melanoma risk, though they more commonly affect skin than nails.
Extremely rarely. Nail melanoma is predominantly a disease of adults, with peak incidence in the 50-70 age range. Pigmented bands in children are almost always benign, but any concerning changes should still be evaluated.
If you have additional questions or concerns about nail changes or other skin lesions, our FAQ section provides helpful information, and our team is always available for consultation.
Knowledge is power, but only when combined with action. If you've read this far, you're already taking an important step in protecting your health. Here's what to do next.
Don't wait and watch indefinitely. While not every dark streak is melanoma, concerning features warrant prompt evaluation:
Red flags requiring urgent evaluation:
Take a deep breath. A melanoma diagnosis is serious, but you're not alone, and treatment options are better than ever.
Immediate steps:
Questions to ask your doctors:
Even if you don't currently have concerning nail changes, awareness helps:
Monthly self-examination:
Annual professional skin examinations:
Spread awareness:
The Minor Surgery Center specializes in the evaluation and treatment of skin lesions, providing expert care in a comfortable, accessible setting. Whether you need evaluation of a concerning nail change, removal of a suspicious lesion, or guidance on next steps, our experienced team is here to help.
What sets us apart:
Ready to take the next step? Contact us to schedule a consultation. Your skin health deserves expert attention, and we're here to provide it.
Nail apparatus melanoma may be rare, but its impact on those affected is profound. The hidden nature of this disease, the diagnostic challenges it presents, and the potential for serious outcomes make it a formidable adversary. Yet, the landscape of melanoma care in 2025 offers genuine hope.
Early detection remains your most powerful weapon. The difference between a curable in situ melanoma and advanced disease often comes down to awareness and timely action. By understanding the warning signs—particularly the ABCDEF criteria and Hutchinson's sign—you can catch this disease when it's most treatable.
Modern treatment options are transforming outcomes. Surgical techniques continue to improve, balancing oncologic control with functional preservation. Immunotherapy and targeted therapy have revolutionized the treatment of advanced disease, turning what was once a rapidly fatal diagnosis into a manageable chronic condition for many patients. Ongoing research promises even better treatments in the years ahead.
You're not alone in this journey. Whether you're monitoring a suspicious nail change, recovering from surgery, or managing advanced disease, a community of healthcare providers, researchers, survivors, and supporters stands ready to help. The Minor Surgery Center is proud to be part of that community, offering expert care delivered with compassion and clarity.
The story of Sarah, which opened this article, has a hopeful ending. Caught at stage IB, her melanoma was successfully treated with digit-preserving surgery. Three years later, she remains cancer-free, vigilant about self-examination, and passionate about sharing her story to help others recognize the warning signs she initially missed.
Your story can have a hopeful ending too. Stay vigilant, seek prompt evaluation of concerning changes, and remember that knowledge combined with action saves lives.
Your next step is clear: If you have any concerning nail changes, don't wait. Schedule an evaluation today. If you're already in treatment, stay committed to your care plan and follow-up schedule. If you're cancer-free, maintain awareness and regular self-examinations.
Your skin tells a story. Make sure you're listening.
For more information about skin conditions, minor surgical procedures, and expert care, visit our blog for helpful resources and updates.