When a small, translucent bump appears near the fingernail, many people worry about what it could mean. Myxoid cysts are among the most common benign growths affecting the fingers and toes, yet they remain poorly understood by most patients. These pearl-like lumps can cause concern, especially when they affect nail appearance or cause discomfort. Understanding myxoid cyst pictures & explanation helps patients recognize these harmless growths, make informed decisions about treatment, and know when to seek medical attention.
This comprehensive guide explores everything about myxoid cysts, from their distinctive appearance to diagnostic methods and treatment options. Whether you've just noticed a suspicious bump or have been living with a diagnosed cyst, this article provides the visual and clinical information needed to understand this common condition.
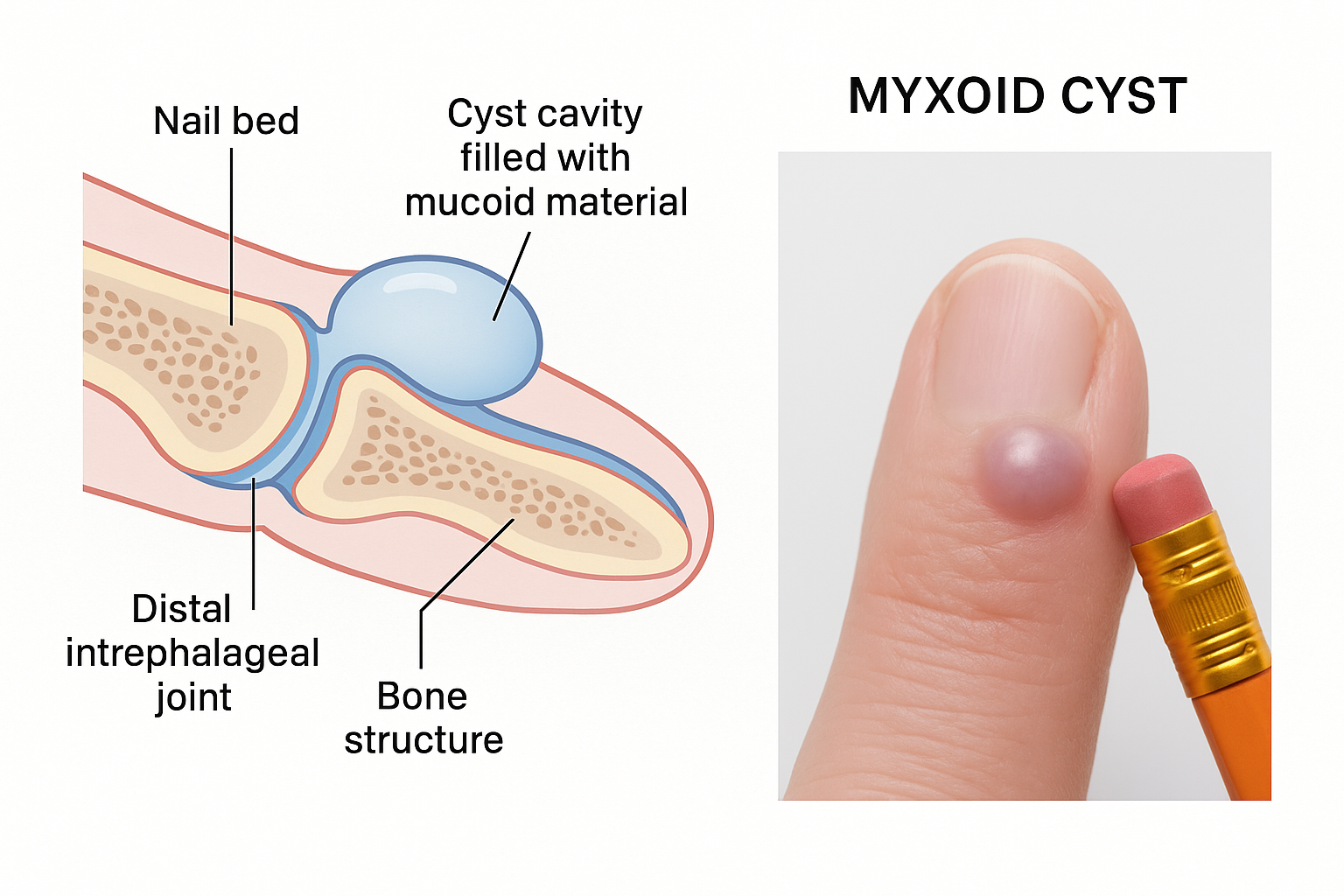
Myxoid cysts, also known as digital mucous cysts or mucous pseudocysts, represent small, noncancerous lumps that develop on the fingers or toes. These benign growths typically measure between 5 millimeters to 1 centimeter in diameter—roughly the size of a pencil eraser—and appear as smooth, round or oval bumps with either a firm or fluid-filled texture.
The term "myxoid" refers to the mucus-like substance contained within these cysts. Unlike true cysts that have an epithelial lining, myxoid cysts are technically pseudocysts because they lack this cellular layer. Instead, they contain a thick, gelatinous material composed of hyaluronic acid and other mucopolysaccharides.
Myxoid cysts show a strong preference for specific locations on the hands and feet:
Most Common Sites:
The cysts almost exclusively develop near the distal interphalangeal (DIP) joint—the joint closest to the fingertip or toe tip. They typically appear on the dorsal (top) surface of the digit, positioned between the last joint and the base of the nail.
Understanding the visual appearance of myxoid cysts helps with identification and differentiation from other conditions:
FeatureDescriptionSize5-10 millimeters (0.2-0.4 inches)ShapeRound, oval, or dome-shapedColorSkin-colored, translucent, pinkish, or bluishTextureSmooth surface, firm or fluctuantTransparencyOften slightly see-through (translucent)ConsistencyMay feel soft and compressible or firm
The translucent quality of myxoid cysts gives them a distinctive pearl-like or bubble-like appearance that sets them apart from other finger bumps. When light shines through them, the fluid content may be visible, creating a characteristic glow.
Recognizing myxoid cysts through visual examination is the first step in diagnosis. Understanding what these cysts look like in various presentations helps patients identify them early and seek appropriate care.
The typical myxoid cyst appears as a smooth, dome-shaped bump positioned just behind the nail fold on the top of the finger. The cyst sits directly over or adjacent to the DIP joint, creating a visible protrusion that may measure anywhere from the size of a small pea to that of a large pencil eraser.
Key Visual Features:
The color of a myxoid cyst can provide clues about its contents and characteristics:
Clear to Yellowish: The most common presentation, indicating typical synovial fluid content with minimal blood or inflammation.
Pinkish or Reddish: May suggest increased vascularity around the cyst or minor bleeding within the cyst cavity. This doesn't necessarily indicate a problem but may occur after trauma.
Bluish Tinge: Often results from the translucent cyst overlying blood vessels or containing slightly bloody fluid. This pearl-like blue appearance is characteristic of myxoid cysts.
Skin-Colored: Some cysts have thicker overlying skin that obscures the translucent quality, making them appear similar to the surrounding skin tone.
Myxoid cysts typically develop slowly over several months, gradually increasing in size. Patients often report first noticing a small bump that progressively enlarges. The growth pattern includes:
Some individuals experience size fluctuations where the cyst appears larger or smaller at different times. This variation occurs because the amount of fluid within the cyst can change, particularly if there's a connection to the underlying joint space.
One of the most distinctive features of myxoid cysts is their effect on nail growth. When a cyst develops close to the nail matrix—the area where nail cells are produced—it can compress this delicate structure and cause characteristic nail deformities.
Common Nail Changes:
✅ Longitudinal grooves running from the base to the tip of the nail
✅ Ridges or depressions creating an uneven nail surface
✅ Nail splitting or separation along the groove lines
✅ Thinning of the nail plate in the affected area
✅ Nail discoloration in severe cases
✅ Complete nail loss in rare, untreated cases with significant pressure
The nail groove typically appears directly in line with the cyst position. If the cyst sits on the right side of the finger, the groove appears on the right side of the nail. This correlation helps confirm the diagnosis and demonstrates the mechanical pressure effect of the cyst on nail formation.
Important Note: Nail changes caused by myxoid cysts are usually reversible if the cyst is successfully treated before permanent damage occurs to the nail matrix.
The fluid contained within myxoid cysts has distinctive characteristics that help differentiate them from other types of cysts and growths. Understanding this content provides insight into the cyst's origin and behavior.
Myxoid cysts are filled with a thick, gelatinous substance that has a consistency similar to clear jelly or egg white. This material is composed primarily of:
The fluid typically appears clear to slightly yellowish, though it may have a pinkish tinge if minor bleeding has occurred within the cyst. When a cyst ruptures or is punctured, this viscous material may leak out, often described by patients as a thick, sticky, clear fluid.
In many cases, myxoid cysts have a direct connection to the underlying DIP joint. This connection explains why the cyst contains synovial fluid—the lubricating fluid normally found within joints. Through a small stalk or channel, joint fluid can flow into the cyst cavity, which explains several important characteristics:
Not all myxoid cysts maintain an active connection to the joint, but the fluid composition suggests most originated from joint-related tissue even if the connection has closed.
Understanding what causes myxoid cysts helps patients recognize their risk factors and potentially prevent future occurrences. While the exact mechanism remains debated, several theories and risk factors have been identified.
Theory 1: Joint Degeneration The most widely accepted explanation links myxoid cysts to osteoarthritis and joint degeneration. As the cartilage in the DIP joint breaks down with age or wear, several changes occur:
This theory explains why myxoid cysts occur predominantly in older adults with arthritic changes in their finger joints.
Theory 2: Mucin Deposition An alternative theory suggests that abnormal deposits of mucopolysaccharides accumulate in the skin and connective tissue near joints. This mucin material attracts water and forms a gelatinous collection, creating the cyst. This mechanism may explain cysts that don't have an obvious connection to the joint space.
Theory 3: Trauma and Repetitive Stress Some researchers believe that repeated minor trauma to the finger joints contributes to cyst formation. Activities involving repetitive finger flexion or pressure on the fingertips may damage connective tissue and create conditions favorable for cyst development.
Several factors significantly increase the likelihood of developing myxoid cysts:
Age and Gender:
Joint Health:
Occupational and Activity Factors:
Other Contributing Factors:
Understanding these risk factors helps explain why certain individuals develop myxoid cysts while others don't, even with similar joint conditions. Much like managing other health conditions requires careful planning—similar to how financial planning requires understanding various factors—recognizing risk factors enables better prevention and management strategies.
While myxoid cysts are often asymptomatic, they can produce various symptoms depending on their size, location, and relationship to surrounding structures.
Visual Changes:
Physical Sensations:
Functional Impact:
Most myxoid cysts cause minimal symptoms and don't interfere with daily activities. However, certain situations warrant medical attention:
Concerning Symptoms:
For most people, myxoid cysts represent more of a cosmetic concern than a functional problem. However, certain activities may be affected:
Potentially Affected Activities:
The psychological impact shouldn't be underestimated. Many patients report self-consciousness about the appearance of their hands, particularly if the cyst is large or causes visible nail deformity. This concern is valid and represents a legitimate reason to consider treatment options.
Accurate diagnosis of myxoid cysts typically involves a combination of clinical examination, patient history, and sometimes imaging studies or other diagnostic procedures.
The diagnostic process usually begins with a thorough physical examination of the affected digit. Healthcare providers look for several characteristic features:
Inspection:
Palpation:
Transillumination: A simple but effective diagnostic technique involves shining a light through the cyst. Because myxoid cysts contain clear or translucent fluid, light passes through them, creating a characteristic glow. This transillumination test helps differentiate myxoid cysts from solid tumors or other growths.
While physical examination often provides sufficient information for diagnosis, imaging studies may be ordered in certain situations:
X-rays:
Ultrasound:
MRI (Magnetic Resonance Imaging):
Healthcare providers must distinguish myxoid cysts from other conditions that can cause similar finger bumps:
Conditions to Rule Out:
ConditionKey Distinguishing FeaturesHeberden's NodesHard, bony enlargements on both sides of joint; not fluid-filledGiant Cell TumorUsually located on the palm side; firm, not translucentGanglion CystCan occur anywhere on hand; typically larger and on wristEpidermoid CystContains white, cheesy material; not near jointVerruca (Wart)Rough surface; caused by viral infectionSquamous Cell CarcinomaIrregular, may ulcerate; more concerning appearance
In some cases, healthcare providers may perform needle aspiration—using a small needle to withdraw fluid from the cyst. This procedure serves both diagnostic and therapeutic purposes:
Diagnostic Benefits:
Therapeutic Benefits:
However, aspiration alone rarely provides permanent resolution, with recurrence rates of 50-70% within months.
Surgical biopsy is rarely necessary for typical myxoid cysts but may be performed if:
Pathological examination of myxoid cyst tissue reveals characteristic features including mucoid material, lack of epithelial lining, and degenerative connective tissue changes.
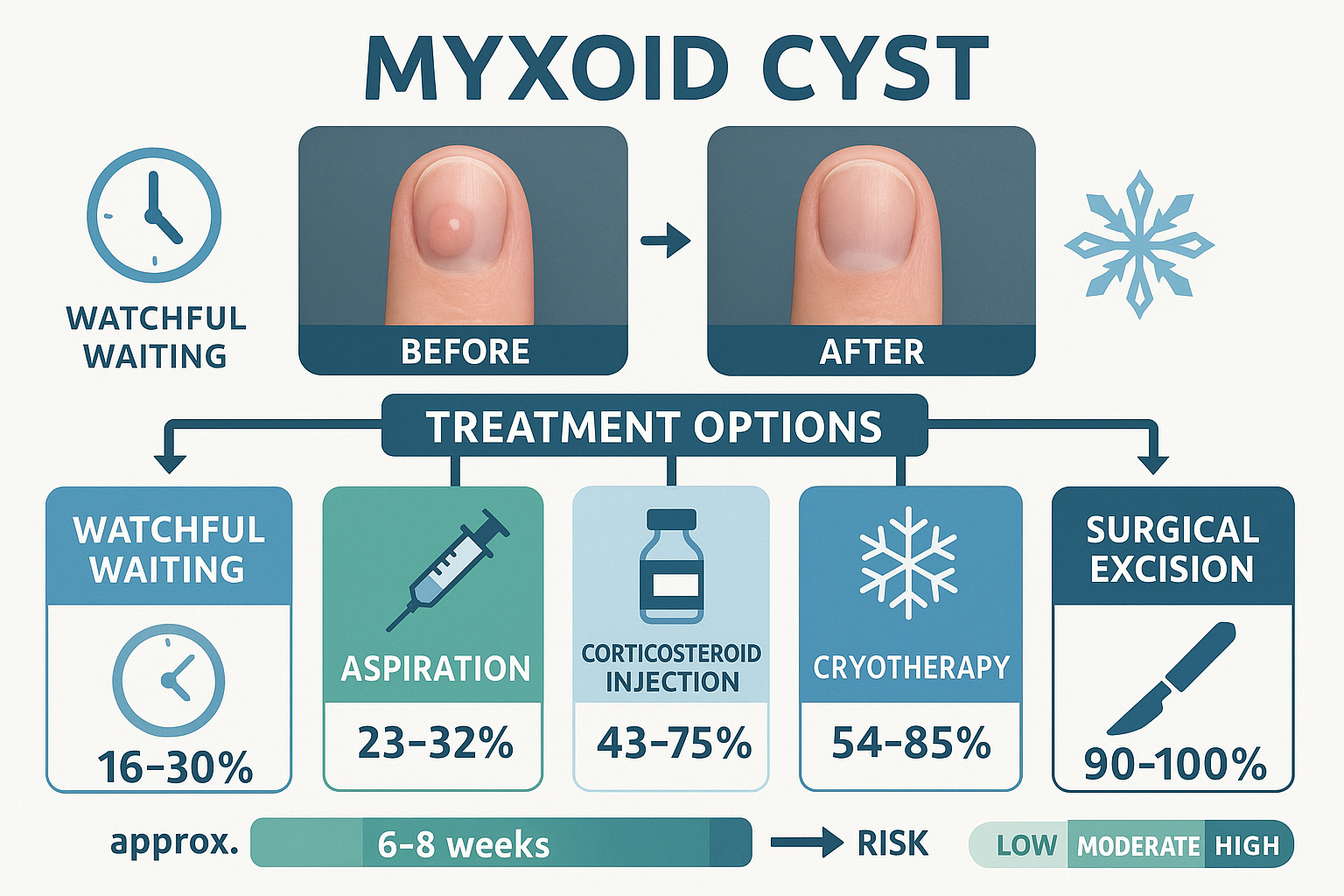
Treatment decisions for myxoid cysts depend on several factors including symptom severity, cosmetic concerns, functional impairment, and patient preferences. Options range from simple observation to surgical excision.
For asymptomatic or minimally bothersome cysts, observation without active treatment represents a reasonable approach. This conservative strategy is appropriate because:
Best Candidates for Observation:
During watchful waiting, patients should monitor for changes such as rapid growth, increasing pain, signs of infection, or progressive nail damage that might prompt treatment.
Several minimally invasive options exist for patients who want treatment but prefer to avoid surgery:
1. Aspiration (Needle Drainage)
This procedure involves using a sterile needle to withdraw fluid from the cyst:
2. Aspiration with Corticosteroid Injection
Combining drainage with corticosteroid medication may improve outcomes:
3. Cryotherapy (Freezing)
Liquid nitrogen application freezes and destroys cyst tissue:
4. Sclerotherapy
Injection of sclerosing agents aims to destroy the cyst lining:
Surgical excision offers the highest cure rate and is considered the definitive treatment for myxoid cysts. The procedure involves complete removal of the cyst along with addressing underlying joint pathology.
Surgical Procedure Details:
Preparation:
Excision Process:
Success Rates:
Recovery:
All treatment modalities carry potential risks that should be discussed with healthcare providers:
General Risks:
Surgery-Specific Risks:
Understanding these risks helps patients make informed decisions about treatment. Just as individuals carefully weigh options when making major decisions—similar to how people evaluate mortgage options—treatment decisions should be based on thorough understanding of benefits and risks.
Understanding what to expect after treatment helps patients prepare for recovery and recognize normal healing versus complications.
After Aspiration:
After Surgical Excision:
When myxoid cysts have caused nail deformities, patients often wonder about nail appearance after treatment:
Timeline for Nail Improvement:
Factors Affecting Nail Recovery:
Patient Perspective: "After my cyst was removed, I was worried about my nail. My doctor explained it would take about nine months for the nail to completely grow out. Sure enough, the groove gradually moved toward the tip as new, normal nail grew from the base. Now you can't even tell there was ever a problem."
The long-term prognosis after myxoid cyst treatment depends on the treatment method and individual factors:
Excellent Outcomes:
Factors Affecting Recurrence:
Managing Recurrence: If a cyst recurs after treatment, options include:
For patients choosing observation or waiting between treatments, several strategies can help manage myxoid cysts and minimize symptoms.
Preventing Rupture:
Why Avoid Rupture: Spontaneous or traumatic cyst rupture can lead to:
When a cyst is causing nail changes, certain measures may help:
Adjusting certain activities can reduce symptoms and prevent cyst enlargement:
Helpful Modifications:
Contact a healthcare provider if any of these situations occur:
While complete prevention of myxoid cysts may not be possible, certain strategies might reduce risk or delay their development.
Since myxoid cysts are closely linked to osteoarthritis, maintaining joint health represents the most important preventive strategy:
Joint Protection Strategies:
For individuals in occupations requiring repetitive hand use:
Since osteoarthritis is the primary risk factor for myxoid cysts, managing arthritis effectively may help:
Much like how proactive financial planning can prevent future problems, early attention to joint health may reduce the risk of developing myxoid cysts.
Understanding how myxoid cysts differ from other finger conditions helps with accurate self-assessment and knowing when to seek medical evaluation.
Heberden's nodes are bony enlargements that occur at the DIP joint, similar in location to myxoid cysts:
Key Differences:
Both conditions are associated with osteoarthritis and may even occur together in the same patient.
Ganglion cysts are the most common hand masses but differ from myxoid cysts:
Distinguishing Features:
These benign tumors can occur on fingers but have distinct characteristics:
How They Differ:
Viral warts can appear on fingers and might be confused with cysts:
Distinctive Features:
FeatureMyxoid CystHeberden's NodeGanglion CystGiant Cell TumorConsistencySoft/firm, fluidHard, bonySoft/firm, fluidFirm, solidLocationNear nail, top of fingerDIP joint, both sidesWrist, variousPalm side of fingerTranslucentYesNoYesNoAge Group40+ years40+ years20-40 years30-50 yearsArthritis LinkStrongStrongWeakNone
No, myxoid cysts are completely benign and do not transform into cancer. They are non-cancerous growths with no malignant potential. However, any unusual finger growth should be evaluated by a healthcare provider to ensure accurate diagnosis.
Approximately 10-30% of myxoid cysts resolve spontaneously without treatment. However, most persist or recur even after spontaneous resolution. The unpredictable nature of these cysts makes it difficult to predict which ones will disappear.
Absolutely not. Self-draining a myxoid cyst carries significant risks:
Always seek professional medical care for cyst drainage.
Recovery timeline varies:
Individual healing rates vary based on surgical extent, patient health, and adherence to post-operative instructions.
In most cases, yes, the nail will return to normal after successful cyst removal, but this takes time. The nail must completely grow out from the matrix to the tip, which takes 6-12 months. If the nail matrix was permanently damaged, some residual deformity may persist.
Yes, though much less common than on fingers, myxoid cysts can develop on toes, particularly the big toe. The same principles of diagnosis and treatment apply to toe cysts.
There is no clear genetic pattern, but some families may have a predisposition to osteoarthritis, which increases myxoid cyst risk. The cysts themselves are not directly inherited.
While no method guarantees prevention of recurrence:
Even with optimal treatment, a small percentage of cysts may recur.
Understanding the relationship between osteoarthritis and myxoid cysts provides insight into prevention and management strategies.
Osteoarthritis represents the single strongest risk factor for myxoid cyst development. Research shows that:
Several arthritis-related changes contribute to cyst development:
1. Joint Capsule Weakening
2. Osteophyte Formation
3. Increased Synovial Fluid Production
The arthritis connection has important treatment implications:
Understanding this connection emphasizes why comprehensive treatment addressing both the cyst and underlying joint pathology produces superior results. Similar to how understanding mortgage fundamentals leads to better financial decisions, understanding the cyst-arthritis relationship leads to better treatment outcomes.
Medical research continues to explore new approaches to myxoid cyst management, offering hope for improved treatments in the future.
Biological Therapies:
Minimally Invasive Techniques:
Preventive Strategies:
Surgical approaches continue to evolve:
Recent Improvements:
Increasing focus on patient perspectives includes:
This research helps align treatment recommendations with patient priorities and values.
Healthcare professionals across specialties offer valuable insights into optimal myxoid cyst management.
Dermatologists frequently diagnose and perform initial treatments for myxoid cysts:
"The key is accurate diagnosis. Many patients worry these bumps might be something serious. Once we confirm it's a benign myxoid cyst, we can discuss the full range of options from observation to referral for surgery. Not every cyst needs treatment—it depends on the patient's symptoms and concerns."
Hand surgeons typically perform definitive surgical treatment:
"When I operate on myxoid cysts, I'm not just removing the cyst—I'm addressing the underlying joint problem. Removing bone spurs and properly closing the joint capsule significantly reduces recurrence rates. The surgery is delicate because we must protect the nail matrix to prevent permanent nail deformity."
Rheumatologists focus on the arthritis connection:
"Myxoid cysts are really a manifestation of underlying osteoarthritis. While we can't reverse arthritis, managing joint inflammation and slowing disease progression may help. Patients with myxoid cysts should have their overall joint health evaluated."
Primary care providers often make initial diagnoses:
"I see myxoid cysts regularly in my practice. My role is to recognize them, reassure patients they're benign, and help them decide whether referral to a specialist is needed. Many patients do well with simple observation and reassurance."
The visible nail deformities caused by myxoid cysts can have significant psychological impact that deserves attention and support.
Nail changes from myxoid cysts can be distressing:
Common Concerns:
Research shows that visible hand conditions can affect:
These psychological effects are valid and important considerations when discussing treatment options.
While awaiting treatment or nail recovery:
Practical Approaches:
Psychological Support:
Understanding that nail appearance will improve after successful treatment provides hope and motivation for patients bothered by cosmetic aspects.
Understanding the financial aspects of myxoid cyst treatment helps patients plan appropriately.
Costs vary significantly based on treatment type and geographic location:
Typical Cost Ranges (Without Insurance):
TreatmentEstimated Cost (USD)Office consultation$100-300Aspiration$200-500Aspiration with injection$300-700Surgical excision$1,500-5,000Imaging (X-ray)$100-300Imaging (MRI)$500-1,500
These are approximate ranges; actual costs depend on provider, facility, and geographic region.
Most health insurance plans cover medically necessary myxoid cyst treatment:
Generally Covered:
May Not Be Covered:
Important Steps:
Similar to how understanding mortgage costs and options helps with financial planning, understanding treatment costs enables better healthcare decision-making.
For patients without insurance or with high out-of-pocket costs:
Certain populations may have unique considerations regarding myxoid cysts.
While myxoid cysts predominantly affect older adults, they occasionally occur in younger people:
Unique Considerations:
Older adults with multiple health conditions require special consideration:
Treatment Modifications:
Individuals whose livelihoods depend on hand function need careful planning:
Special Considerations:
Diabetes affects healing and infection risk:
Important Factors:
Myxoid cysts represent common, benign growths that can cause concern due to their appearance and potential impact on nail health. Understanding myxoid cyst pictures & explanation empowers patients to recognize these lesions, understand their relationship to underlying joint conditions, and make informed decisions about management.
About the Condition:
Treatment Approach:
Prognosis:
If you have or suspect a myxoid cyst:
Choosing the appropriate healthcare provider depends on your situation:
Don't hesitate to seek second opinions or specialist consultation if you have concerns about your diagnosis or treatment plan.
While myxoid cysts can be bothersome, they represent a manageable condition with multiple treatment options. The benign nature of these growths should provide reassurance, while the availability of effective treatments offers hope for those experiencing symptoms or cosmetic concerns.
By understanding the visual characteristics, causes, and treatment options for myxoid cysts, patients can actively participate in their healthcare decisions and achieve optimal outcomes. Whether choosing observation or pursuing treatment, informed patients working collaboratively with knowledgeable healthcare providers achieve the best results.
Remember that each person's situation is unique, and treatment recommendations should be individualized based on symptoms, lifestyle, priorities, and overall health status. With proper care and realistic expectations, most people with myxoid cysts can expect excellent long-term outcomes.
[1] Rizzo M, Baldridge CR. Mucous cyst of the finger. J Hand Surg Am. 2009;34(4):722-724.
[2] Epstein E. A simple technique for managing digital mucous cysts. Arch Dermatol. 1979;115(11):1315-1316.
[3] Karrer S, Hohenleutner U, Szeimies RM, Landthaler M. Treatment of digital mucous cysts with a carbon dioxide laser. Acta Derm Venereol. 1999;79(3):224-225.
[4] Fritz GR, Stern PJ, Dickey M. Complications following mucous cyst excision. J Hand Surg Br. 1997;22(2):222-225.
[5] Thornburg LE. Ganglions of the hand and wrist. J Am Acad Orthop Surg. 1999;7(4):231-238.
[6] de Berker D, Goettmann S, Baran R. Subungual myxoid cysts: clinical manifestations and response to therapy. J Am Acad Dermatol. 2002;46(2):394-398.
[7] Goldman JA, Goldman L, Jaffe MS, Richfield DF. Digital mucinous pseudocysts. Arthritis Rheum. 1977;20(4):997-1002.
[8] Connolly M, de Berker DA. Management of primary nail disorders. Am J Clin Dermatol. 2001;2(6):373-381.
[9] Lawrence C. Skin excision and closure. In: Robinson JK, Hanke CW, Sengelmann RD, Siegel DM, eds. Surgery of the Skin: Procedural Dermatology. 2nd ed. Philadelphia: Elsevier Mosby; 2010:129-150.
[10] Kleinert HE, Kutz JE, Fishman JH, McCraw LH. Etiology and treatment of the so-called mucous cyst of the finger. J Bone Joint Surg Am. 1972;54(7):1455-1458.