Imagine discovering a familiar dark spot reappearing exactly where you had a mole removed months or years ago. That sinking feeling in your stomach isn't just anxiety—it's your body's way of telling you to pay attention. A mole growing back in scar tissue isn't just a cosmetic concern; it can be a critical warning sign that demands immediate medical evaluation.
While most mole removals are successful and permanent, the unexpected return of pigmented tissue in a surgical scar can indicate anything from incomplete removal to something far more serious. Understanding why this happens, when to worry, and what steps to take can literally be the difference between early intervention and a missed opportunity for treatment.
• Incomplete removal is the most common reason for a mole growing back in scar tissue, often due to residual pigmented cells left behind during the initial procedure
• Immediate medical evaluation is essential when any pigmented growth appears in a surgical scar, as it could indicate malignant transformation
• Proper surgical technique and complete excision with clear margins significantly reduce the likelihood of mole recurrence
• Regular monitoring of all surgical sites is crucial for early detection of any concerning changes
• Professional assessment can distinguish between benign regrowth and potentially dangerous developments
When a mole growing back in scar occurs, it's typically because some melanocytes (pigment-producing cells) remained in the deeper layers of skin after the initial removal. These cells can become active again, leading to the reformation of pigmented tissue within the healing scar.
Common reasons for mole recurrence include:
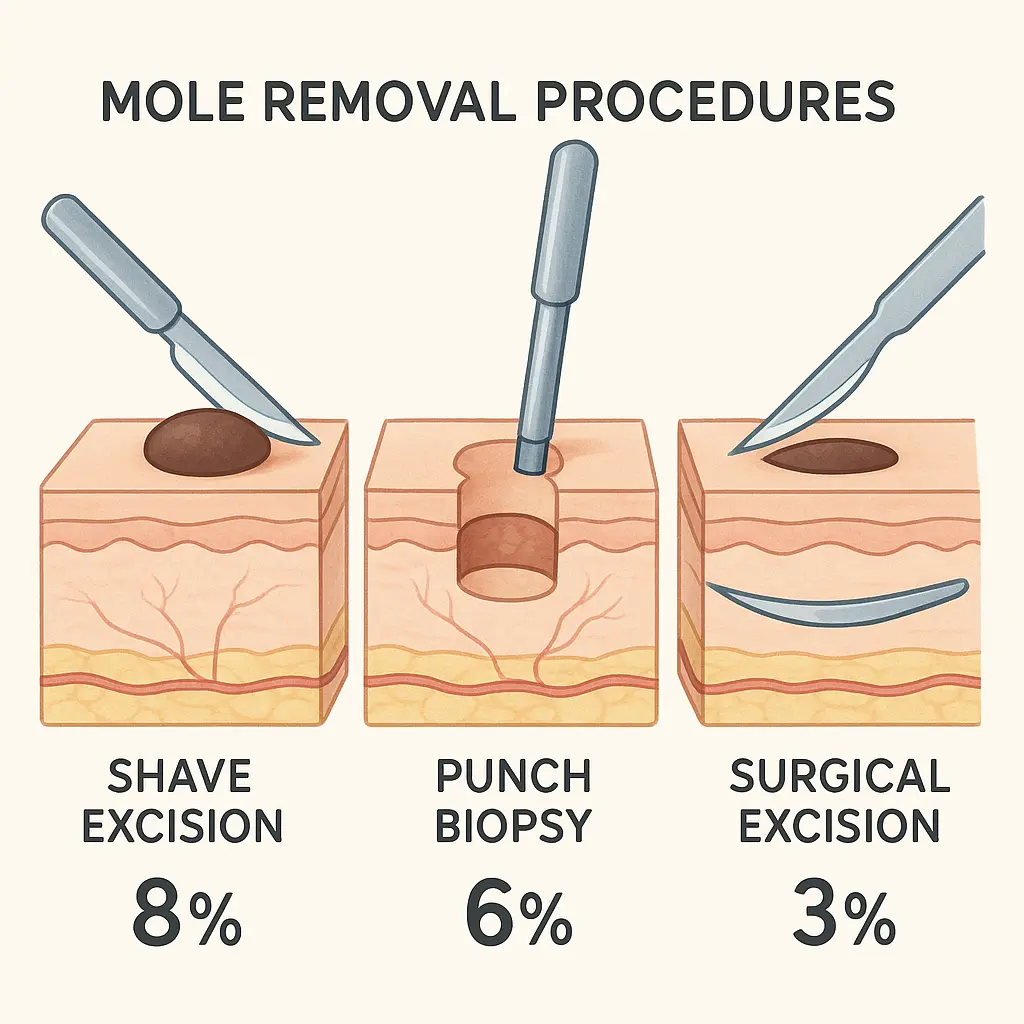
Different removal methods carry varying risks for recurrence:
Removal MethodRecurrence RiskWhy Recurrence HappensShave excisionHigher (10-20%)May not remove deep melanocytesPunch biopsyModerate (5-15%)Limited by punch sizeSurgical excisionLower (2-5%)Complete removal with marginsLaser removalVariableDepth penetration limitations
Not all mole recurrences are created equal. Certain characteristics should trigger immediate medical attention:
Visual changes that demand urgent evaluation:
When evaluating a mole growing back in scar tissue, healthcare professionals use an adapted version of the ABCDE rule:
A - Asymmetry: One half doesn't match the other B - Border: Irregular, scalloped, or poorly defined edges C - Color: Multiple colors or unusual pigmentation D - Diameter: Larger than a pencil eraser (6mm) E - Evolving: Any change in size, shape, color, or symptoms
"The most concerning sign is rapid change. A mole that reappears and evolves quickly within scar tissue should be evaluated immediately, as this pattern can indicate malignant transformation." - Dermatological Surgery Guidelines
When you notice a mole growing back in scar, the evaluation process typically follows these steps:
Modern dermatology employs sophisticated tools for evaluating suspicious growths:
Dermoscopy (Dermatoscopy):
Digital imaging:
Confocal microscopy:
When a mole growing back in scar requires treatment, several surgical options are available:
Wide local excision:
Mohs micrographic surgery:
In select cases of benign recurrence, non-surgical options may be considered:
The best treatment for a mole growing back in scar is prevention through proper initial removal:
Factors to discuss with your surgeon:
Proper wound care and monitoring significantly impact outcomes:
Essential post-operative steps:
Certain situations require immediate medical attention when dealing with a mole growing back in scar tissue:
🔴 Seek emergency care if:
Even without concerning symptoms, regular check-ups are essential:
Recommended timeline:
For comprehensive evaluation and treatment of concerning moles, consider consulting with specialists at The Minor Surgery Center, where experienced professionals can provide expert assessment and treatment options.
Several factors influence the likelihood of experiencing a mole growing back in scar tissue:
Patient-specific risk factors:
Anatomical considerations:
Understanding your condition empowers better decision-making. Valuable resources include:
Advanced technology now enables better tracking of mole changes:
Digital dermoscopy mapping:
Smartphone applications:
AI-powered diagnostic tools are revolutionizing mole evaluation:
Discovering a mole growing back in scar can trigger significant emotional distress:
Common psychological responses:
Healthy coping strategies:
Making informed decisions requires:
For personalized care and expert guidance, the experienced team at The Minor Surgery Center provides comprehensive support throughout the evaluation and treatment process.
The prognosis for patients with a mole growing back in scar depends on several factors:
Factors influencing outcomes:
Statistical outcomes:
Successful management of mole recurrence involves more than just medical treatment:
Factors affecting quality of life:
Children and adolescents require special consideration when dealing with mole recurrence:
Unique factors in young patients:
Hormonal changes during pregnancy can affect mole behavior:
Special considerations:
Patients with compromised immune systems face additional challenges:
Enhanced risk factors:
The financial aspect of managing a mole growing back in scar varies significantly:
Typical cost ranges:
Most insurance plans cover medically necessary mole treatments:
Covered services typically include:
Documentation requirements:
For information about insurance coverage and payment options, contact The Minor Surgery Center to discuss your specific situation.
Scientific advancement continues to improve outcomes for patients with mole recurrence:
Promising developments:
Patients with challenging cases may benefit from clinical trial participation:
Types of research studies:
Managing a mole growing back in scar often requires a multidisciplinary approach:
Key healthcare professionals:
Successful treatment requires excellent communication between providers:
Essential coordination elements:
The comprehensive care team at The Minor Surgery Center specializes in coordinated, patient-centered approaches to mole management and removal.
Q: How quickly can a mole grow back in scar tissue? A: Recurrence can happen anywhere from weeks to years after initial removal, depending on the underlying cause and completeness of the original procedure.
Q: Does mole recurrence always mean cancer? A: No, most mole recurrences are benign. However, any pigmented growth in a surgical scar requires professional evaluation to rule out malignant transformation.
Q: Can I prevent mole recurrence? A: While not always preventable, choosing experienced surgeons, ensuring complete excision, and following post-operative care instructions significantly reduce recurrence risk.
Q: What's the difference between recurrence and a new mole? A: Recurrence appears within or immediately adjacent to the original surgical scar, while new moles develop in previously unaffected areas.
For answers to additional questions, visit the comprehensive FAQ section or speak directly with medical professionals.
A mole growing back in scar tissue represents a significant medical concern that demands prompt, professional evaluation. While not every recurrence indicates malignancy, the potential for serious complications makes immediate assessment crucial for optimal outcomes.
The key to successful management lies in understanding the warning signs, seeking appropriate medical care, and working with experienced healthcare professionals who can provide accurate diagnosis and effective treatment. Modern medical technology and surgical techniques offer excellent outcomes for patients who receive timely, appropriate care.
Your next steps should include:
Remember, early detection and appropriate treatment provide the best possible outcomes. Don't wait to address concerning changes—your health and peace of mind depend on taking prompt action when a mole shows signs of returning in scar tissue.
For expert evaluation and treatment of mole recurrence, the specialists at The Minor Surgery Center offer comprehensive care with the latest diagnostic and treatment technologies. Taking action today can make all the difference in your long-term health and well-being.