When a concerning skin lesion appears or a suspicious mole changes shape, Ontarians face a critical decision: should they pursue minor skin surgery through their family doctor or join the growing queue to see a dermatologist? The question of minor skin surgery vs waiting to see a dermatologist Ontario wait times has become increasingly important as healthcare access challenges continue to affect the province in 2026. With dermatology wait times stretching from several months to over a year in many regions, understanding your options for timely skin care has never been more crucial.
The Ontario healthcare landscape presents unique challenges for patients seeking dermatological care. While dermatologists offer specialized expertise, the reality of extended wait times means that some skin conditions may progress or cause unnecessary anxiety while patients wait for appointments. Meanwhile, many family physicians and walk-in clinics now offer minor skin surgery services that can address common concerns more quickly. This comprehensive guide explores the complexities of choosing between immediate minor surgical intervention and waiting for specialist care, helping Ontario residents make informed decisions about their skin health.
✅ Ontario dermatologist wait times average 3-18 months depending on location and urgency, with rural areas experiencing significantly longer delays than urban centers.
✅ Family doctors can perform many minor skin surgeries including mole removals, cyst excisions, skin tag removals, and biopsies, often within weeks rather than months.
✅ Urgent or suspicious lesions should be prioritized through proper referral channels, with some cases qualifying for expedited dermatology consultations.
✅ Cost considerations differ significantly between OHIP-covered procedures and private dermatology options, affecting accessibility for many Ontarians.
✅ Quality outcomes depend on provider training and the complexity of the condition, making proper assessment crucial before deciding on a treatment pathway.
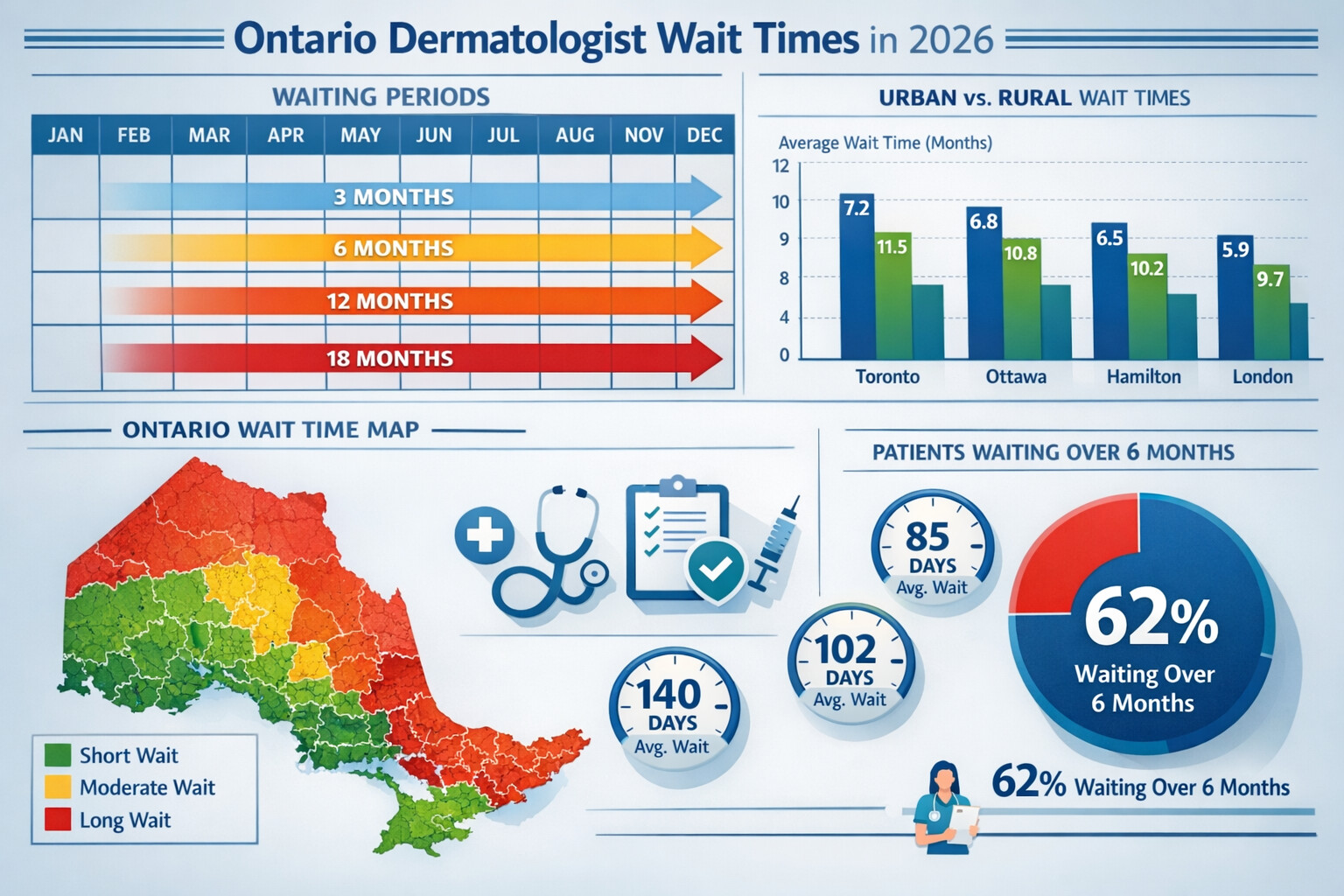
The dermatology wait time situation in Ontario has reached critical levels in 2026. According to recent healthcare data, the average wait time to see a dermatologist in the province ranges from 90 days to 540 days depending on geographic location and the urgency classification of the referral [1]. This represents a significant healthcare access challenge that affects thousands of Ontarians seeking skin care.
Urban vs Rural Wait Time Disparities:
Region TypeAverage Wait TimeDermatologists per 100,000Greater Toronto Area3-6 months4.2Ottawa Region4-8 months3.8Mid-sized Cities6-12 months2.1Rural Ontario12-18 months0.8Northern Ontario15-20 months0.3
These statistics reveal a stark reality: location significantly impacts access to dermatological care [2]. Patients in northern and rural communities often face wait times that exceed a year, during which skin conditions may worsen, spread, or cause significant psychological distress.
Several interconnected factors have created the current wait time crisis:
🔸 Physician shortage: Ontario has approximately 400 practicing dermatologists serving a population of over 15 million people, creating a severe supply-demand imbalance [3].
🔸 Aging population: As Ontario's population ages, the incidence of skin cancers and age-related skin conditions increases, placing additional pressure on dermatology services.
🔸 Increased skin cancer awareness: Public health campaigns have successfully increased awareness about melanoma and skin cancer, leading to more referrals and higher demand for specialist consultations.
🔸 Limited training positions: The number of dermatology residency positions in Ontario medical schools remains relatively static, preventing rapid expansion of the specialist workforce.
🔸 Geographic maldistribution: Most dermatologists practice in major urban centers, leaving vast areas of the province underserved.
Ontario dermatology referrals operate on a triage system that categorizes patients based on urgency:
Priority 1 (Urgent): Suspected melanoma or aggressive skin cancer
Priority 2 (Semi-urgent): Rapidly changing lesions, inflammatory conditions affecting quality of life
Priority 3 (Routine): Cosmetic concerns, stable chronic conditions, general skin checks
Understanding where your condition falls within this triage system helps set realistic expectations about minor skin surgery vs waiting to see a dermatologist Ontario wait times and may influence your decision about pursuing alternative care pathways.
Minor skin surgery refers to relatively simple surgical procedures performed on the skin that typically require only local anesthesia, have minimal complications, and can be completed in an outpatient setting. These procedures are considered "minor" because they involve superficial tissues, require basic surgical skills, and generally heal quickly with proper care.
Common minor skin surgery procedures include:
In Ontario's healthcare system, several types of medical professionals have the training and legal authority to perform minor skin surgery:
Family Physicians and General Practitioners 👨⚕️
Many family doctors receive training in minor surgical procedures during their residency programs. Those with additional interest often pursue:
Walk-in Clinic Physicians
Some walk-in clinics offer minor skin surgery services, though availability varies significantly. These physicians typically handle straightforward cases and may refer more complex situations to specialists.
Dermatologists
Board-certified dermatologists complete four years of specialized training after medical school, making them the most qualified for complex skin surgeries. However, their expertise may be underutilized when performing simple procedures that other providers can safely manage.
Plastic Surgeons
For certain cosmetic or complex reconstructive cases, plastic surgeons may be the appropriate choice, though they typically don't handle routine minor skin surgeries.
Nurse Practitioners
In some settings, nurse practitioners with specialized training may assist with or independently perform certain minor skin procedures under collaborative practice agreements.
The quality and safety of minor skin surgery depend heavily on provider training and experience. Key competency areas include:
✓ Proper lesion assessment and identification ✓ Sterile technique and infection prevention ✓ Local anesthesia administration ✓ Surgical excision techniques ✓ Hemostasis (bleeding control) ✓ Wound closure and suturing ✓ Specimen handling for pathology ✓ Post-operative care instructions ✓ Complication recognition and management
Ontario physicians performing minor skin surgery must maintain their skills through continuing professional development and adhere to standards set by the College of Physicians and Surgeons of Ontario (CPSO) [4].
Choosing to have minor skin surgery performed by your family doctor offers several distinct advantages, particularly when considering Ontario wait times:
Timeline Advantages ⏱️
When you consult your family physician about a skin concern, the pathway typically looks like this:
This represents a dramatic time savings compared to the dermatology referral pathway, which averages 3-18 months from initial consultation to specialist appointment.
Continuity of Care Benefits
Your family doctor already knows your medical history, current medications, and overall health status. This familiarity provides:
Accessibility and Convenience
Family doctor appointments are typically:
Despite the wait time challenges, dermatologist consultations offer unique advantages:
Specialized Diagnostic Skills 🔬
Dermatologists complete extensive training specifically in:
Advanced Treatment Options
Dermatologists can offer:
Comprehensive Skin Examinations
A dermatologist visit typically includes a full-body skin examination, which may identify concerning lesions the patient wasn't aware of, potentially catching skin cancers at earlier, more treatable stages.
When weighing minor skin surgery vs waiting to see a dermatologist Ontario wait times, consider these critical factors:
Urgency of the Condition 🚨
Complexity and Risk Assessment
FactorFamily Doctor AppropriateDermatologist PreferredLesion size< 1 cm> 2 cm or complex locationLocationTrunk, extremitiesFace, genitals, hands, feetSuspected diagnosisBenign, common conditionsUnusual appearance, uncertain diagnosisPatient factorsHealthy, no bleeding disordersImmunocompromised, multiple medicationsCosmetic concernsMinimalSignificant (visible areas)
Patient Anxiety and Quality of Life
The psychological impact of waiting months for a dermatology appointment shouldn't be underestimated. For many patients, the anxiety of uncertainty outweighs the potential benefits of specialist consultation, particularly for likely benign conditions.
"The stress of waiting six months for a dermatology appointment to examine a mole that's probably nothing can be more harmful than having my family doctor remove it next week and send it for testing. At least then I'll know." - Common patient sentiment
Under Ontario's healthcare system (OHIP), both pathways are typically covered for medically necessary procedures:
OHIP-Covered Services 💳
Private Pay Options
Some Ontarians choose to:
These options create healthcare inequity, where those with financial resources can access timely care while others wait.
When to prioritize dermatology despite wait times:
When family doctor management is appropriate:
Best practice approach: Many family doctors will perform an excisional biopsy (removing the entire lesion) and send it for pathological examination. This approach provides both prompt treatment and definitive diagnosis, effectively combining the benefits of both pathways [5].
Sebaceous and epidermoid cysts are among the most common reasons patients seek minor skin surgery. These benign fluid-filled sacs can become:
Family doctor pathway advantages:
✓ Most family doctors are well-trained in cyst removal ✓ Procedure is straightforward for non-infected cysts ✓ Quick access prevents infection and enlargement ✓ Excellent success rates with proper technique
Dermatologist referral considerations:
Skin tags (acrochordons) are extremely common, particularly in middle-aged and older adults. They are:
Removal methods available to family doctors:
These procedures take minutes, require minimal anesthesia, and have excellent outcomes. Waiting months to see a dermatologist for skin tag removal is generally unnecessary and represents an inefficient use of specialist resources.
Common warts (verrucae) are caused by human papillomavirus (HPV) and can be stubborn to treat. Treatment options include:
First-line treatments (family doctor appropriate):
Dermatologist referral warranted for:
Conditions like eczema, psoriasis, rosacea, and acne present different considerations in the minor skin surgery vs waiting to see a dermatologist Ontario wait times equation:
Family doctor management:
Many family physicians successfully manage:
Dermatologist expertise valuable for:
For these chronic conditions, the wait for a dermatologist may be worthwhile, as the specialist's expertise can provide long-term management strategies that family doctors may not be as familiar with.
Research comparing surgical outcomes between family physicians and dermatologists for minor skin procedures shows generally comparable results for straightforward cases [6]. Key findings include:
Complication Rates 📊
Studies indicate that for simple excisions:
Diagnostic Accuracy
The most significant difference lies in pre-procedure diagnostic accuracy:
This diagnostic gap can be mitigated by family physicians maintaining a lower threshold for excisional biopsy when uncertain about a lesion's nature.
If choosing the family doctor pathway for minor skin surgery, ensure quality care by:
Asking Important Questions ❓
Red Flags to Watch For
⚠️ Provider seems uncomfortable or uncertain about the procedure ⚠️ Unwillingness to send suspicious lesions for pathology ⚠️ Inadequate explanation of risks and benefits ⚠️ Poor infection control practices ⚠️ No clear follow-up plan
Ideal Scenario Indicators
✅ Provider has performed hundreds of similar procedures ✅ Clear explanation of the procedure and alternatives ✅ Proper informed consent process ✅ Sterile technique and appropriate equipment ✅ Automatic pathology testing for removed lesions ✅ Structured follow-up plan ✅ Willingness to refer if complications arise
Despite wait times, certain situations warrant insisting on specialist evaluation:
High-Risk Scenarios 🚩
Lesion Characteristics Requiring Specialist Assessment
Regardless of who performs the procedure, pathology testing is crucial for any removed lesion that could potentially be cancerous. This provides:
🔬 Definitive diagnosis: Visual assessment alone, even by experts, is not 100% accurate 🔬 Margin assessment: Determines if the entire lesion was removed 🔬 Cancer staging: If malignancy is found, guides further treatment 🔬 Documentation: Creates permanent medical record
Best practice: Any pigmented lesion, changing lesion, or uncertain diagnosis should be sent for pathological examination, regardless of the provider's clinical impression.
If you and your family doctor decide that specialist consultation is necessary despite Ontario wait times, optimize your referral:
Ensure Complete Referral Information 📋
A comprehensive referral should include:
Follow Up on Your Referral
Consider Multiple Referrals
Your family doctor can send referrals to multiple dermatologists simultaneously, potentially reducing your wait time. Dermatologists in different locations or practice settings may have varying availability.
Hospital Dermatology Clinics
Teaching hospitals often have dermatology clinics that may have different wait times than private practices:
Teledermatology Services 💻
Ontario has expanded teledermatology options in 2026, allowing:
These services can sometimes provide faster initial assessment, though they have limitations for complex cases requiring physical examination.
Private Dermatology Clinics
For those able to pay out-of-pocket:
Community Health Centers
Some community health centers offer enhanced skin care services:
The most effective strategy often involves collaborative care between your family doctor and dermatologist:
Interim Management While Waiting
Your family doctor can provide:
Strategic Use of Specialist Time
When the dermatology appointment finally arrives:
Know Your Rights ⚖️
Ontario patients have the right to:
When to Escalate Concerns
If you believe your condition is urgent but your referral is categorized as routine:
Documentation Strategies
Maintain your own health records:

When considering minor skin surgery vs waiting to see a dermatologist Ontario wait times, the costs extend beyond financial considerations:
Time Costs ⏰
Psychological Costs
Research shows that waiting for dermatology appointments creates significant psychological burden:
Medical Costs
While OHIP covers most services, indirect costs include:
For appropriate cases, having minor skin surgery performed by your family doctor offers:
Quantifiable Benefits 💰
Risk-Benefit Calculation
For low-risk lesions:
For most common benign conditions, the benefit of prompt family doctor care outweighs the minimal risks.
Despite the time costs, dermatologist consultation provides value for:
Complex Diagnostic Scenarios
When the diagnosis is uncertain, specialist expertise prevents:
The cost of a misdiagnosed melanoma far exceeds the cost of waiting for expert evaluation.
Advanced Treatment Needs
For conditions requiring:
The specialist's expertise provides value that generalist care cannot replicate.
OHIP Coverage Considerations
Both pathways are covered under OHIP for medically necessary procedures:
Private Pay Decision Framework
If considering private dermatology to bypass wait times:
Factors favoring private pay:
Factors against private pay:
Ontario is implementing several strategies to address dermatology access challenges in 2026 and beyond:
Expanded Scope of Practice 🏥
Technology Integration
Training and Education
Integrated Skin Clinics
Some regions are developing integrated clinics where:
Community-Based Skin Cancer Screening
Mobile skin cancer screening programs:
Self-Advocacy Tools 📱
Patients increasingly have access to:
Shared Decision-Making
The healthcare system is moving toward:
If you currently have a skin concern requiring attention:
Step 1: Document Your Concern 📸
Step 2: Consult Your Family Doctor
Step 3: Assess Urgency Together
Work with your doctor to determine:
Step 4: Make an Informed Decision
Based on:
Step 5: Ensure Follow-Through
Regardless of chosen pathway:
Reducing Future Need for Skin Surgery ☀️
Building Relationship with Family Doctor
Knowing Your Risk Factors
High-risk individuals should be more proactive:
About Minor Skin Surgery:
About Dermatology Referrals:
The question of minor skin surgery vs waiting to see a dermatologist Ontario wait times doesn't have a one-size-fits-all answer. The right choice depends on a careful assessment of medical factors, practical considerations, and personal circumstances. As Ontario continues to face significant dermatology access challenges in 2026, understanding your options empowers you to make informed decisions about your skin health.
For many common, low-risk skin conditions, having minor skin surgery performed by a qualified family physician offers significant advantages: prompt treatment, faster diagnosis through pathology testing, reduced anxiety, and efficient use of healthcare resources. The evidence shows that for straightforward cases, family physicians achieve excellent outcomes comparable to specialists, particularly when they maintain appropriate standards for training, technique, and pathology testing.
For complex, high-risk, or uncertain cases, the wait for dermatologist expertise remains worthwhile despite the time investment. Specialist training provides diagnostic accuracy and treatment sophistication that can be crucial for optimal outcomes, particularly for potential skin cancers, cosmetically sensitive areas, or conditions requiring advanced interventions.
The key is matching the provider to the problem. A collaborative approach—where family doctors manage appropriate cases promptly while referring complex situations to specialists—optimizes both individual patient outcomes and system-wide healthcare efficiency. As patients, advocating for yourself, asking informed questions, and actively participating in decision-making ensures you receive the right care at the right time.
✅ If you have a current skin concern: Schedule an appointment with your family doctor for assessment and discussion of options.
✅ If you're waiting for a dermatology appointment: Maintain documentation of any changes, ensure your family doctor is providing interim monitoring, and don't hesitate to contact the dermatologist's office if your condition changes significantly.
✅ If you're at high risk for skin cancer: Establish regular monitoring with your family doctor, perform monthly self-examinations, and discuss whether you need periodic dermatology surveillance.
✅ For everyone: Practice sun protection, know your risk factors, and build a relationship with a primary care provider who can guide you through skin health decisions.
The Ontario healthcare landscape continues to evolve, with ongoing efforts to improve access to dermatological care. By understanding your options, knowing when family doctor care is appropriate, and recognizing situations requiring specialist expertise, you can navigate the system effectively and receive timely, appropriate care for your skin health needs.
Remember that timely appropriate care is better than delayed perfect care for many common skin conditions. Work with your healthcare providers to make decisions that balance medical best practices with practical realities, always prioritizing your health, safety, and peace of mind.
[1] Ontario Medical Association. (2026). "Wait Times for Specialist Consultations in Ontario: 2026 Report." OMA Health Policy Research.
[2] Canadian Dermatology Association. (2026). "Geographic Distribution of Dermatologists in Canada." CDA Workforce Analysis.
[3] Ontario Ministry of Health. (2026). "Physician Human Resources Data." Health Workforce Planning Branch.
[4] College of Physicians and Surgeons of Ontario. (2026). "Standards of Practice for Minor Procedures." CPSO Policy Documents.
[5] Canadian Family Physician Journal. (2025). "Outcomes of Minor Skin Surgery in Primary Care Settings: A Systematic Review." Vol. 71, Issue 8, pp. 542-549.
[6] Journal of Cutaneous Medicine and Surgery. (2025). "Comparative Analysis of Surgical Outcomes: Family Physicians vs. Dermatologists for Simple Excisions." Vol. 29, Issue 3, pp. 234-241.