You glance down at your fingernails and notice something new—a dark, vertical line running from the cuticle to the tip. It wasn't there before. Should you be worried? That dark streak has a name: melanonychia. While it's often harmless, understanding what causes these pigmented bands and when to seek medical attention can give you peace of mind and protect your health.
Melanonychia affects people of all ages and backgrounds, but it's particularly common in certain populations. Whether you've just noticed a single dark line or you're dealing with multiple bands, this comprehensive guide will help you understand everything you need to know about this nail condition—from its causes and types to diagnosis and treatment options.
Melanonychia is the medical term for brown or black discoloration of the nail plate. The name comes from "melano" (meaning melanin or pigment) and "onychia" (relating to the nail). This condition manifests as longitudinal melanonychia—vertical bands or streaks that run from the base of the nail to the tip.
Think of your nail as a canvas. Normally, it's a pale pink color that lets the blood vessels underneath show through. When melanonychia occurs, specialized cells called melanocytes deposit extra pigment into the nail as it grows, creating visible dark lines or bands.
The prevalence of melanonychia varies significantly by ethnicity:
PopulationPrevalence RateAfrican descent77-100%Asian descent10-20%Hispanic descent10-15%Caucasian descent1-2%
These statistics highlight that melanonychia is extremely common in darker-skinned individuals and is usually a normal variant rather than a cause for concern.
Understanding the different types of melanonychia helps determine whether your condition requires medical attention.
This is the most common presentation—vertical dark bands running the length of the nail. These bands can be:
Rather than distinct bands, the entire nail plate appears darkened. This pattern is less common and may indicate systemic causes like medication side effects or nutritional deficiencies.
Horizontal dark lines across the nail (rather than vertical) are rare and typically result from temporary disruption to nail growth, such as trauma or illness.
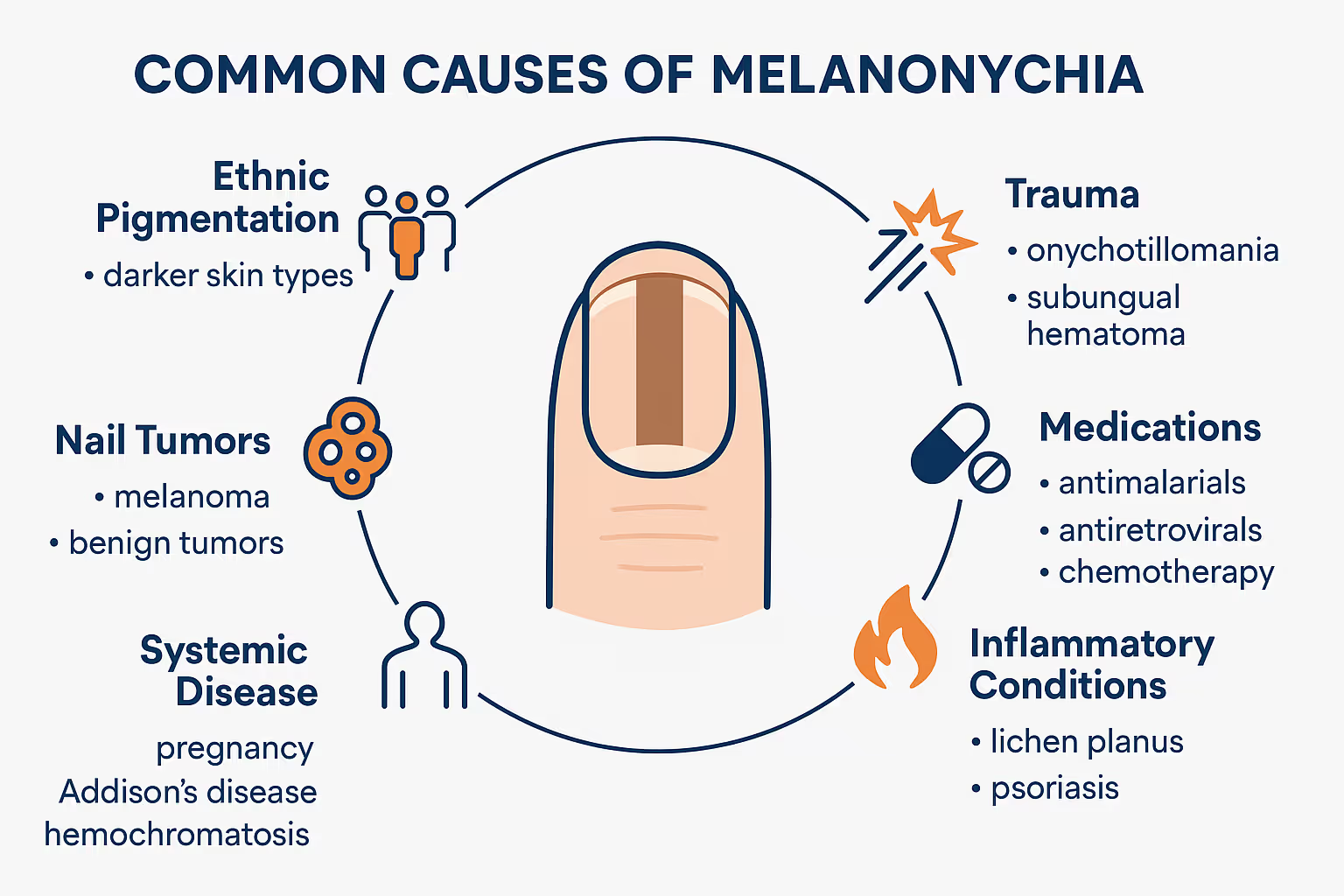
The causes of melanonychia fall into two main categories: benign (harmless) and malignant (potentially dangerous). Let's explore both.
For many people—especially those with darker skin tones—melanonychia is simply a normal variant. It's part of your genetic makeup, like having brown eyes or curly hair. These bands typically:
Repeated friction or a single traumatic event can stimulate melanocytes in the nail matrix (the growth zone beneath the cuticle). Common causes include:
Certain medications can trigger melanonychia as a side effect, including:
This type usually affects multiple nails and resolves when you stop taking the medication.
Skin diseases affecting the nail area can cause pigmentation changes:
Certain medical conditions may present with nail pigmentation:
Non-cancerous growths in the nail matrix can produce pigment:
This is the most serious cause of melanonychia—a type of skin cancer that develops beneath the nail. While rare (accounting for only 0.7-3.5% of all melanomas), it's crucial to identify early.
Warning signs include:
Important: If you notice any of these warning signs, seek evaluation from a healthcare professional immediately. Early detection of melanoma significantly improves treatment outcomes.
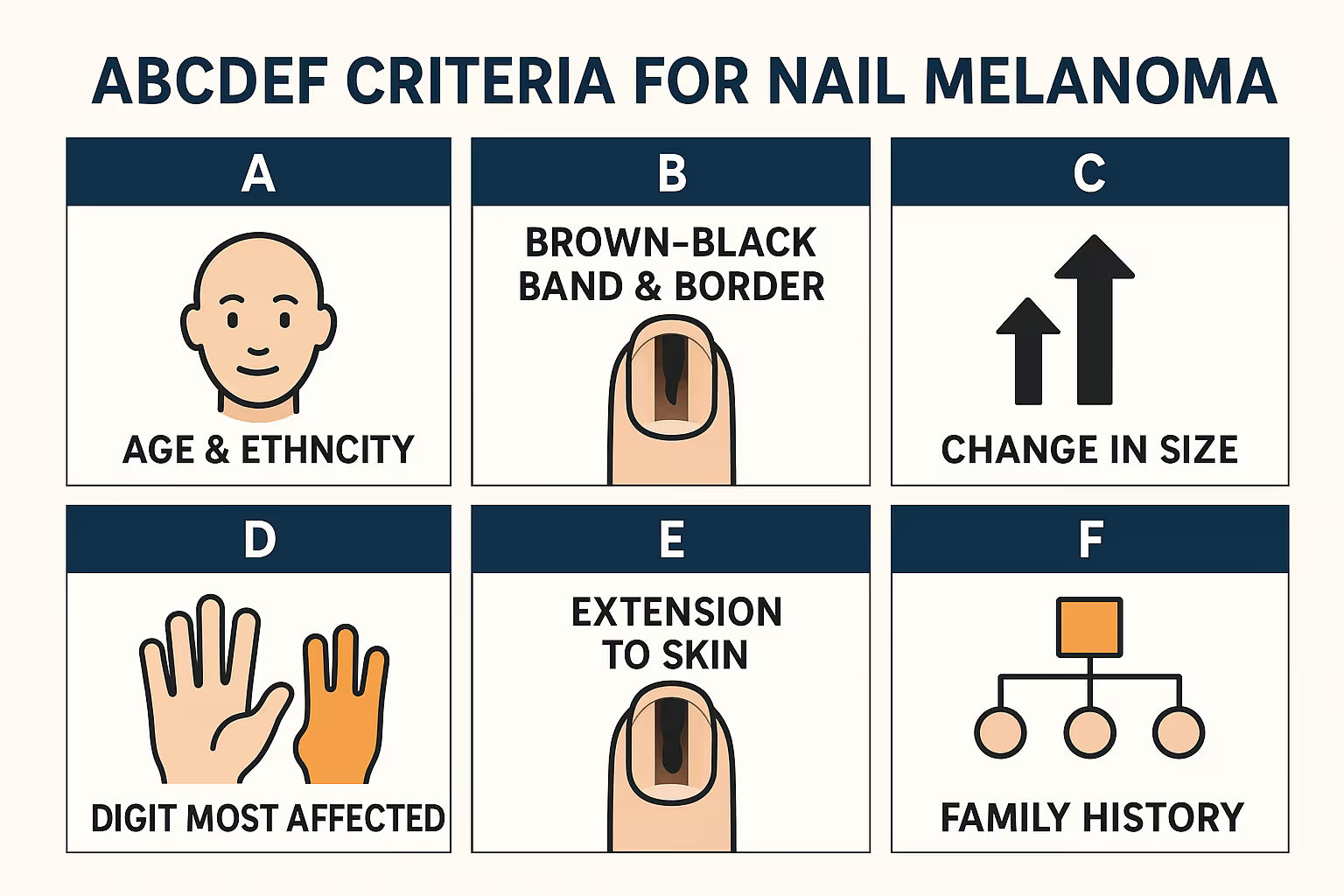
Dermatologists use the ABCDEF criteria to assess suspicious melanonychia:
If multiple criteria are present, medical evaluation is essential.
When you visit a healthcare professional at The Minor Surgery Center, they'll use several approaches to determine the cause of your melanonychia.
Your doctor will carefully inspect the affected nail(s) and ask about:
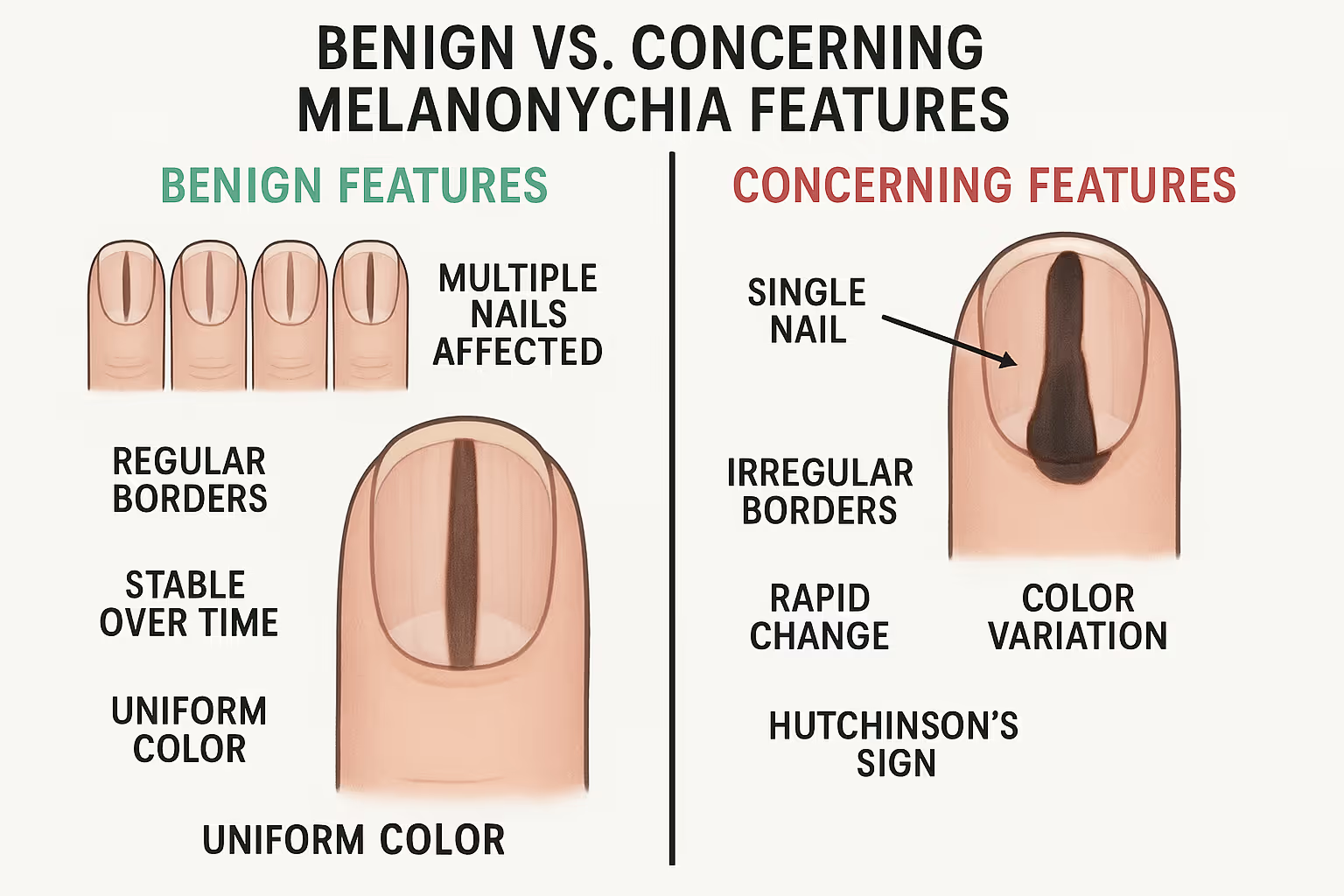
This non-invasive technique uses a specialized magnifying device to examine the nail in detail. Dermoscopy can reveal patterns that help distinguish benign from malignant causes:
When there's uncertainty about the diagnosis—especially if melanoma is suspected—a biopsy may be necessary. This procedure involves:
While the thought of a nail biopsy might sound uncomfortable, it's a straightforward procedure performed in an outpatient setting. Our experienced surgeons specialize in making minor surgical procedures safe, quick, and as comfortable as possible.
In rare cases where deeper structures might be involved, imaging such as ultrasound or MRI may be recommended.
The appropriate treatment depends entirely on the underlying cause.
Observation Only
Most cases of benign melanonychia require no treatment at all. If your pigmented band is:
...then simple monitoring is all that's needed. Take photos periodically to track any changes, and report new developments to your doctor.
Addressing Underlying Causes
If melanonychia results from a specific trigger, treatment focuses on that:
Surgical Removal of Benign Lesions
If a benign nevus or other growth is causing the pigmentation and you prefer removal for cosmetic reasons or peace of mind, minor surgery can be performed. The procedure involves:
Surgical Excision
If melanoma is confirmed, the standard treatment involves:
Additional Treatments
Depending on the stage and spread of melanoma, additional therapies may include:
Early-stage melanoma confined to the nail has a much better prognosis than advanced disease, which is why prompt evaluation of suspicious pigmentation is so important.
Not every dark line on your nail requires immediate medical attention, but certain situations warrant professional evaluation:
✅ A new pigmented band appearing, especially if you're over 50
✅ A band that's changing in width, color, or shape
✅ Irregular borders or color variation within the band
✅ Pigmentation spreading beyond the nail onto the skin
✅ A band affecting only one nail (especially thumb, index finger, or big toe)
✅ Nail changes like splitting, cracking, or lifting
✅ Bleeding or pain associated with the pigmentation
✅ A personal or family history of melanoma
✔ You have multiple pigmented bands that have been stable for years
✔ The bands appeared during childhood or adolescence
✔ You have darker skin and the pattern is consistent with ethnic pigmentation
✔ The bands have regular, well-defined borders
✔ There's been no recent change in appearance
When in doubt, it's always better to get checked. The Minor Surgery Center provides expert evaluation in a welcoming, anxiety-free environment—no referral needed.
If you have benign melanonychia that doesn't require treatment, these tips can help you maintain healthy nails and monitor for changes:
Melanonychia in children is usually benign, especially in those with darker skin tones. However, pediatric melanoma—while extremely rare—does occur. Any new or changing pigmented band in a child should be evaluated by a pediatric dermatologist.
This age group may develop melanonychia from:
Maintain awareness of changes and seek evaluation for concerning features.
New melanonychia appearing after age 50 requires careful evaluation, as this is when melanoma risk increases. Don't dismiss new pigmentation as simply "age-related"—get it checked.
Discovering an unexpected dark line on your nail can be unsettling. It's completely normal to feel:
Remember that most melanonychia is harmless. However, your concerns are valid, and seeking professional evaluation is the right step. Our compassionate team understands that even minor health concerns can cause significant worry, and we're here to provide clear answers and expert care.
If you're concerned about the cost of evaluation or treatment for melanonychia, several factors come into play:
The Minor Surgery Center offers transparent pricing and can help you understand your options. We believe you shouldn't have to choose between your health and your budget.
It's helpful to distinguish melanonychia from other types of nail discoloration:
If you're uncertain about what type of discoloration you have, our clinic can provide expert assessment.
Yes, if caused by trauma or medication, melanonychia often fades as the nail grows out. However, this process takes months since nails grow slowly (fingernails: 2-3mm per month; toenails: 1mm per month). Melanonychia from ethnic pigmentation or benign nevi typically persists indefinitely.
No, melanonychia is not contagious. It's caused by pigment production within your own nail cells, not by bacteria, viruses, or fungi that could spread to others.
Dark nail polish itself doesn't cause melanonychia, but it can temporarily stain nails (which is different from melanonychia). However, chronic use of nail polish and harsh removers might contribute to nail trauma that could trigger melanonychia.
Never stop prescribed medication without consulting your doctor. If medication is causing melanonychia, your healthcare provider can help you weigh the benefits of the medication against cosmetic concerns and discuss alternatives if appropriate.
A complete fingernail takes about 6 months to grow out entirely, while a toenail can take 12-18 months. If the underlying cause has been addressed, you'll see clear nail growing from the base, gradually replacing the pigmented portion.
Yes, you can use nail polish to cover benign melanonychia for cosmetic reasons. However, it's important to remove the polish periodically to check for any changes in the pigmentation. Never use polish to hide a pigmented band that hasn't been properly evaluated.
For more answers to common questions, visit our FAQ page.
While you can't prevent melanonychia related to genetics or ethnicity, you can reduce your risk of trauma-induced or other preventable forms:
While this guide provides comprehensive information about melanonychia, nothing replaces professional medical evaluation. Here's why seeing a healthcare provider matters:
✨ Accurate Diagnosis: What appears to be melanonychia might be something else entirely
✨ Early Detection: Catching melanoma early dramatically improves outcomes
✨ Peace of Mind: Professional reassurance alleviates anxiety
✨ Personalized Guidance: Your unique situation requires individualized assessment
✨ Appropriate Treatment: If intervention is needed, you'll receive expert care
The Minor Surgery Center specializes in evaluating and treating nail conditions in a comfortable, patient-focused environment. You don't need a referral—just schedule an appointment and get the answers you need.
Understanding what happens during a melanonychia evaluation can ease any nervousness:
Your healthcare provider will:
Depending on the findings, you may:
Our team ensures you leave with clear understanding and a concrete plan forward.
Medical understanding of melanonychia continues to evolve. Current research focuses on:
As research progresses, diagnosis and treatment of melanonychia will become even more precise and patient-friendly.
While every case of melanonychia is unique, understanding common scenarios can help you relate your situation to others' experiences:
Maria, a 28-year-old woman of African descent, noticed dark bands on several fingernails during her teenage years. They've remained stable for over a decade. After evaluation, her doctor confirmed these are normal ethnic variants requiring only periodic monitoring.
James, 55, developed dark lines on multiple nails six weeks after starting chemotherapy. His oncologist confirmed this was an expected side effect. The pigmentation gradually faded several months after completing treatment.
Sarah, an avid runner, noticed a dark band on her big toenail after increasing her training mileage. Examination revealed this was due to repetitive trauma from her running shoes. After switching to properly fitted shoes, new nail growth appeared clear.
Robert, 62, noticed a new dark band on his thumb that widened over three months. Concerned, he sought evaluation. A biopsy revealed early-stage melanoma. Thanks to prompt treatment, the outcome was excellent.
These scenarios illustrate the spectrum of melanonychia presentations and outcomes. Your story matters, and professional evaluation ensures you receive appropriate care for your specific situation.
If you're dealing with melanonychia, here's your action plan:
Review the warning signs discussed in this article. Does your melanonychia have concerning features, or does it appear benign?
Take clear, well-lit photos of the affected nail(s) from multiple angles. Note when you first observed the pigmentation.
If you have any concerns, don't wait. Contact The Minor Surgery Center to schedule a consultation. Early evaluation provides peace of mind and ensures appropriate care.
Gather your medical history, medication list, and questions. Being prepared helps you get the most from your visit.
Whether you need ongoing monitoring, biopsy, or treatment, follow your healthcare provider's recommendations. Your nail health matters.
Continue monitoring your nails and stay aware of changes. Knowledge empowers you to maintain your health.
Melanonychia—those mysterious dark lines on your nails—can range from completely harmless ethnic pigmentation to a warning sign of melanoma. Understanding the difference is crucial for your health and peace of mind.
Remember these key points:
You deserve to feel confident about your health. That's why we make melanonychia evaluation fast, simple, and clear—without the wait. The Minor Surgery Center provides expert care in a welcoming environment where your concerns are heard and addressed with compassion and professionalism.
Don't let uncertainty about a dark line on your nail keep you up at night. Whether you need reassurance that your melanonychia is benign or prompt treatment for a concerning lesion, our experienced surgeons are here to help.
Your skin—and your nails—are our specialty. Schedule your consultation today and get the answers you need.
For more information about the conditions we treat and the services we provide, explore our comprehensive resources or find a clinic near you.