Discovering small bumps under your eyes can be alarming, especially when they appear suddenly or persist for weeks. While these tiny formations might cause cosmetic concerns or discomfort, the vast majority are completely harmless and treatable. Understanding what causes these bumps and knowing when to seek professional help can provide peace of mind and guide you toward the most effective treatment approach.
• Most common cause: Milia (keratin-filled cysts) account for the majority of little bumps under eyes and typically resolve on their own
• Infection signs: Red, tender, or pus-filled bumps may indicate styes or other infections requiring medical attention
• Prevention matters: Proper eye hygiene and gentle skincare routines can significantly reduce bump formation
• Professional evaluation: Persistent bumps lasting over 6 weeks or those affecting vision should be examined by a healthcare provider
• Treatment varies: Management ranges from simple home care to minor surgical procedures depending on the bump type and severity
Little bumps under eyes represent one of the most common dermatological concerns affecting people of all ages. These small formations can appear as white, yellow, red, or skin-colored protrusions ranging from barely visible to several millimeters in diameter. While often mistaken for acne or other skin conditions, under-eye bumps typically have distinct characteristics and causes that require specific approaches for effective management.
The delicate skin around the eyes makes this area particularly susceptible to various types of bumps and cysts. The thin tissue, combined with frequent movement from blinking and facial expressions, creates unique conditions that can lead to blocked pores, trapped keratin, or bacterial infections. Understanding these mechanisms helps explain why certain treatments work better than others for different types of bumps.
Most importantly, the majority of little bumps under eyes are benign and pose no serious health risks. However, knowing how to identify different types and when to seek professional care ensures optimal outcomes and prevents potential complications.
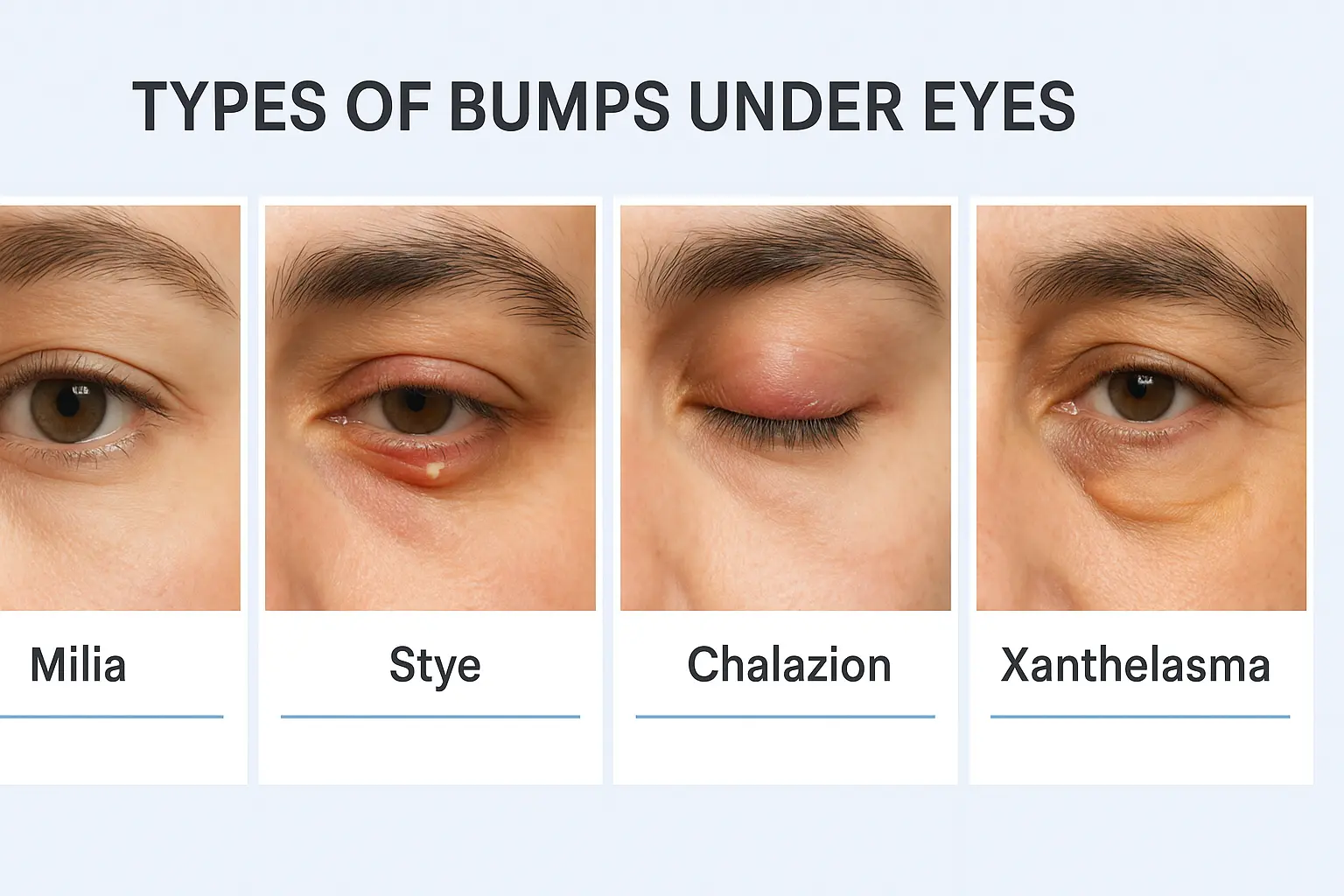
Milia represent the leading cause of small white or yellowish bumps under the eyes [1]. These tiny cysts form when keratin becomes trapped beneath the skin surface, creating firm, pearl-like bumps measuring 1-2 millimeters in diameter [5]. Unlike acne, milia don't have an opening to the skin surface, making them impossible to extract through squeezing.
Key characteristics of milia include:
Milia occur when dead skin cells fail to shed naturally during the skin's renewal process [5]. This keratin accumulation creates small cysts that can persist for months or even years without intervention. While milia can affect anyone, they're particularly common in newborns and tend to resolve spontaneously as the skin matures.
Styes present as red, tender bumps caused by bacterial infections in eyelash follicles or oil glands [1][4]. These inflammatory lesions typically develop when bacteria, most commonly Staphylococcus aureus, invade the hair follicles or sebaceous glands along the eyelid margin.
Stye characteristics include:
There are two main types of styes:
TypeLocationCharacteristicsExternal StyeEyelash follicle or sebaceous glandVisible bump on eyelid edgeInternal StyeMeibomian gland inside eyelidLess visible, more painful
Most styes resolve spontaneously without requiring medical intervention [2]. However, proper care and hygiene can accelerate healing and prevent complications.
Chalazia represent chronic blockages of meibomian glands in the eyelid, often developing from untreated styes [1][3]. Unlike styes, chalazia are typically painless and can persist for weeks or months without proper treatment.
Chalazion features include:
Chalazia form when the meibomian glands, which produce oils that help prevent tear evaporation, become blocked with thickened secretions. This blockage creates a firm, non-tender nodule that can become quite prominent if left untreated.
Xanthelasma appears as yellowish plaques around the eyes and may indicate underlying cholesterol disorders [1]. These deposits of cholesterol can signal systemic health issues requiring medical evaluation.
Syringomas are small, flesh-colored bumps caused by overgrowth of sweat ducts. They're more common in women and tend to appear symmetrically around both eyes.
Sebaceous hyperplasia creates small, yellowish bumps when oil glands become enlarged. These are more common in older adults and areas with high sebaceous gland density.
Understanding the underlying mechanisms behind bump formation helps explain why certain individuals are more susceptible and how prevention strategies work.
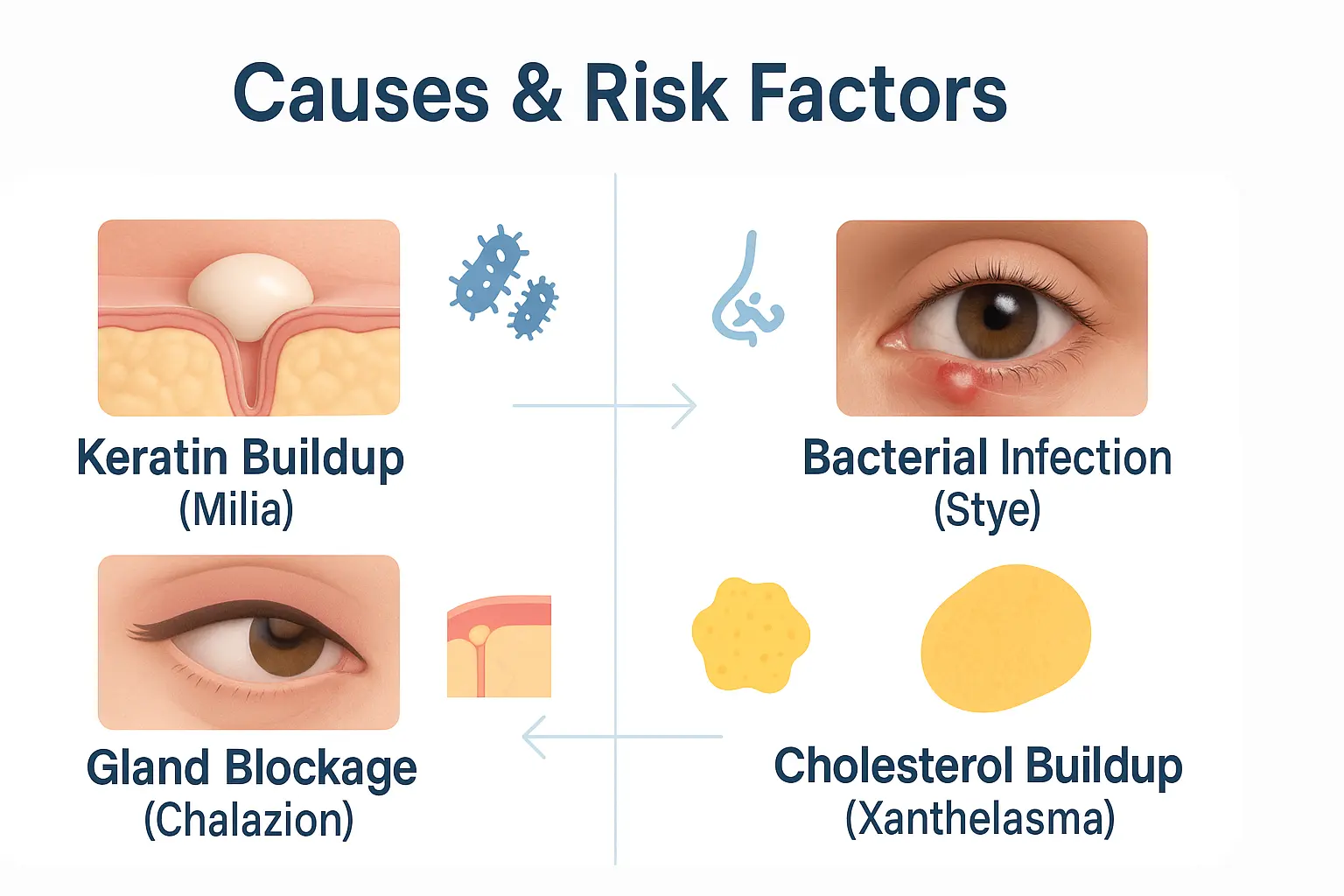
Keratin Accumulation 🔬 The most common cause involves natural skin turnover processes where keratin becomes trapped beneath the skin surface [5]. When dead skin cells fail to shed properly during exfoliation, they can accumulate in pores and hair follicles, creating the characteristic white or yellowish bumps associated with milia.
Bacterial Infections 🦠 Styes develop when bacteria invade eyelash follicles or oil glands [4]. Staphylococcus aureus represents the most frequent culprit, though other bacterial species can also cause infections. Poor hygiene, touching the eyes with dirty hands, or using contaminated makeup can introduce bacteria and trigger infections.
Gland Dysfunction ⚙️ Meibomian gland dysfunction plays a central role in chalazion formation [3]. These glands produce oils essential for tear film stability, but when secretions become thick or glands become blocked, cysts can develop.
Several factors increase the likelihood of developing little bumps under eyes:
Blepharitis significantly increases susceptibility to both styes and chalazia [1]. This chronic inflammatory condition affects eyelid margins and creates an environment conducive to bacterial growth and gland dysfunction.
Rosacea patients often experience increased rates of ocular complications, including various types of eyelid bumps. The inflammatory nature of rosacea can affect the delicate eye area and predispose individuals to secondary infections.
Hormonal fluctuations can trigger bump formation by affecting:
FactorImpactPrevention StrategyPoor hygieneIncreases bacterial exposureRegular gentle cleansingContaminated makeupIntroduces bacteria and irritantsReplace products regularlyEye rubbingSpreads bacteria, causes irritationAvoid touching eyesStressAffects immune function and hormonesStress management techniquesContact lens useCan harbor bacteria if not properly cleanedProper lens hygiene
Certain systemic conditions can predispose individuals to under-eye bumps:
Diabetes affects immune function and wound healing, potentially increasing infection risk and slowing resolution of existing bumps.
Autoimmune conditions can alter skin barrier function and immune responses, making individuals more susceptible to various types of skin formations.
Cholesterol disorders may manifest as xanthelasma around the eyes, serving as visible indicators of systemic lipid metabolism issues [1].
Proper identification of little bumps under eyes requires careful observation of specific visual features. Each type has distinctive characteristics that help guide appropriate treatment decisions.
Size Variations 📏
Color Patterns 🎨
Texture and Shape ✨
Different types of under-eye bumps produce varying symptom patterns that aid in identification and treatment planning.
Asymptomatic bumps typically include:
Symptomatic bumps often involve:
Certain symptoms warrant immediate professional evaluation:
Healthcare providers use several approaches to accurately diagnose under-eye bumps:
Visual Examination 👁️ Most diagnoses can be made through careful visual inspection, noting size, color, texture, and location patterns.
Medical History 📋 Previous episodes, family history, associated skin conditions, and medication use provide important diagnostic clues.
Specialized Testing 🔬 In rare cases, providers might recommend:
While most little bumps under eyes are harmless, certain situations require prompt professional evaluation. Understanding these warning signs helps ensure appropriate and timely care.
Vision-Related Concerns 👀 Any bump that affects vision requires immediate attention. Large chalazia can press against the eye, causing:
Signs of Serious Infection 🚨 Systemic infection symptoms include:
Rapid Changes ⚡ Bumps requiring urgent evaluation:
6-8 weeks: Most benign bumps should show signs of improvement or resolution within this timeframe. Persistent lesions warrant professional assessment to rule out:
Pattern recognition becomes important when dealing with:
Different age groups have varying risk profiles and evaluation criteria:
Most little bumps under eyes respond well to conservative treatment approaches that can be safely implemented at home. These methods focus on supporting natural healing processes while preventing complications.
Warm compresses represent the cornerstone of home treatment for many under-eye bumps, particularly styes and early chalazia. The heat helps:
Proper technique:
Proper hygiene plays a crucial role in both treatment and prevention:
Daily cleansing routine:
Specialized eyelid cleansers may benefit individuals with:
Several non-prescription treatments can provide relief:
Treatment TypeBest ForApplication MethodAntibiotic ointmentsEarly styesApply thin layer 2-3 times dailyArtificial tearsAssociated drynessUse as needed for comfortAnti-inflammatory dropsMild swellingFollow package directions
When conservative measures prove insufficient or bumps meet criteria for professional intervention, several medical treatment options are available.
Topical antibiotics for bacterial infections:
Oral antibiotics for severe or recurrent infections:
Steroid treatments for inflammatory conditions:
When medical management fails or bumps cause significant symptoms, surgical intervention may be necessary.
Incision and Drainage 🔪 This procedure involves:
Excision Procedures ✂️ Complete removal may be recommended for:
Laser Treatments ⚡ Advanced laser therapies can address:
Since milia result from trapped keratin, treatment focuses on:
Important Note: Never attempt to extract milia at home, as this can lead to scarring, infection, or further keratin entrapment.
Patients experiencing frequent bumps may benefit from:
Professional dermatologists and ophthalmologists at specialized clinics can provide comprehensive evaluation and treatment planning for persistent or complex cases.
Implementing consistent hygiene routines represents the most effective approach to preventing little bumps under eyes. These practices address the primary risk factors while supporting healthy skin function.
Gentle cleansing should begin each day:
Makeup application best practices:
Complete makeup removal prevents pore blockage:
Moisturizing considerations:
Since bacterial transfer from hands represents a major risk factor:
Proper lens hygiene prevents bacterial accumulation:
PracticeFrequencyImportanceReplace solutionDailyPrevents bacterial growthClean caseWeeklyEliminates biofilm formationReplace lensesAs prescribedReduces protein buildupHand washingBefore handlingPrevents contamination
Quality sleep and stress reduction support immune function:
Key characteristics to look for:
Certain ingredients can increase bump formation risk:
While diet doesn't directly cause under-eye bumps, certain nutritional factors may influence skin health:
Omega-3 fatty acids support:
Vitamin A promotes:
Zinc supports:
Adequate water intake helps:
Regular professional evaluation can identify risk factors and provide personalized prevention strategies. Healthcare providers can assess for underlying conditions that might predispose individuals to recurrent bumps and recommend targeted interventions.
Experienced medical teams can provide comprehensive preventive care plans tailored to individual risk profiles and medical histories.
While most little bumps under eyes resolve without issues, understanding possible complications helps ensure appropriate monitoring and timely intervention when necessary.
Cellulitis represents the most serious bacterial complication, occurring when infection spreads beyond the initial bump into surrounding tissues. Warning signs include:
Abscess formation can develop when bacterial infections become walled off, creating pockets of pus that may require surgical drainage.
Chronic infection may result from inadequate treatment or antibiotic-resistant organisms, leading to persistent symptoms and potential scarring.
Large chalazia or multiple bumps can cause:
Long-term cosmetic concerns may include:
Understanding recurrence patterns helps set realistic expectations and guide prevention strategies.
Some people experience higher recurrence rates due to:
Many individuals notice seasonal patterns:
The overall outlook for individuals with little bumps under eyes remains excellent, with most people experiencing:
FactorImpact on OutcomeManagement StrategyEarly treatmentBetter cosmetic resultsSeek care promptlyUnderlying conditionsMay affect healingTreat systemic issuesPatient complianceDirectly affects successFollow treatment plansProfessional careReduces complicationsRegular monitoring
While physically benign, under-eye bumps can significantly impact quality of life through:
Patients should track:
Regular professional evaluation helps:
Healthcare providers specializing in various conditions affecting the eye area can provide comprehensive long-term management plans tailored to individual needs and risk factors.
Patients often have specific questions about little bumps under eyes that address both immediate concerns and long-term management strategies.
Milia and most cystic bumps are not contagious as they result from natural skin processes rather than infectious agents.
Styes and bacterial infections can potentially spread through:
Prevention of spread involves:
Generally safe when following proper guidelines:
Temporary avoidance may be recommended for:
Scarring risk factors include:
Minimizing scar risk:
Timeline expectations vary by condition and treatment:
ConditionConservative TreatmentMedical TreatmentMilia6-12 months (natural resolution)1-2 weeks (professional extraction)Styes7-10 days3-5 days with antibioticsChalazia4-6 weeks2-3 weeks with treatment
Consider treatment changes when:
While no specific foods directly cause under-eye bumps, nutritional factors that may help include:
Hormonal influences can affect:
Common hormonal triggers:
Dermatology referral may be appropriate for:
Ophthalmology consultation for:
Patients seeking comprehensive evaluation can find detailed information about available services and specialized care options.
Important topics to discuss:
Typically covered:
Often not covered:
Cost-saving strategies:
Little bumps under eyes, while often concerning to those who develop them, represent largely manageable conditions with excellent outcomes when properly understood and treated. The vast majority of these formations—from common milia to bacterial styes—respond well to appropriate care and rarely cause lasting complications.
Key success factors include:
The journey from initial concern to resolution typically follows a predictable pattern. Most individuals find that simple hygiene measures and conservative treatments effectively address their symptoms, while others benefit from professional interventions that provide rapid relief and prevent complications.
Moving forward, focus on:
✅ Implementing daily prevention strategies through gentle cleansing routines and proper eye hygiene
✅ Monitoring changes in existing bumps and watching for new developments
✅ Seeking timely professional care when bumps persist, worsen, or affect vision
✅ Maintaining realistic expectations about treatment timelines and outcomes
✅ Building a relationship with healthcare providers who understand your specific needs and risk factors
For individuals experiencing persistent or recurrent issues, remember that specialized medical professionals offer comprehensive evaluation and treatment options tailored to individual circumstances. The combination of patient education, appropriate medical care, and consistent preventive practices provides the foundation for optimal long-term outcomes.
Take action today by implementing proper eye hygiene practices and scheduling professional evaluation if you have concerns about existing bumps. With the right approach, little bumps under eyes need not cause ongoing worry or significantly impact your quality of life.
For more information about professional evaluation and treatment options, consider contacting specialized healthcare providers who can provide personalized assessment and care recommendations based on your specific situation and needs.
[1] American Academy of Ophthalmology. (2023). Eyelid Bumps: Styes, Chalazia, Xanthelasma, Milia. Clinical Guidelines for Eye Care.
[2] Mayo Clinic. (2023). Stye (Sty): Symptoms, Causes, and Treatment. Mayo Clinic Proceedings.
[3] Journal of the American Medical Association. (2022). Management of Chalazion: A Systematic Review. JAMA Ophthalmology, 140(8), 785-792.
[4] Dermatology Online Journal. (2023). Periocular Dermatitis: Etiology, Clinical Features, and Management. DOJ, 29(3), 15-22.
[5] American Academy of Dermatology. (2023). Milia: Diagnosis and Treatment Guidelines. AAD Clinical Resources.