When a simple surgical procedure becomes a lifetime of raised, thick scar tissue that grows beyond the original wound site, the impact extends far beyond cosmetic concerns. For individuals with keloid-prone skin, every incision carries the risk of developing these aggressive, overgrown scars that can cause pain, itching, and significant emotional distress. Understanding how to prevent and manage keloids through strategic pre- and post-operative care can mean the difference between successful healing and years of scar revision attempts.
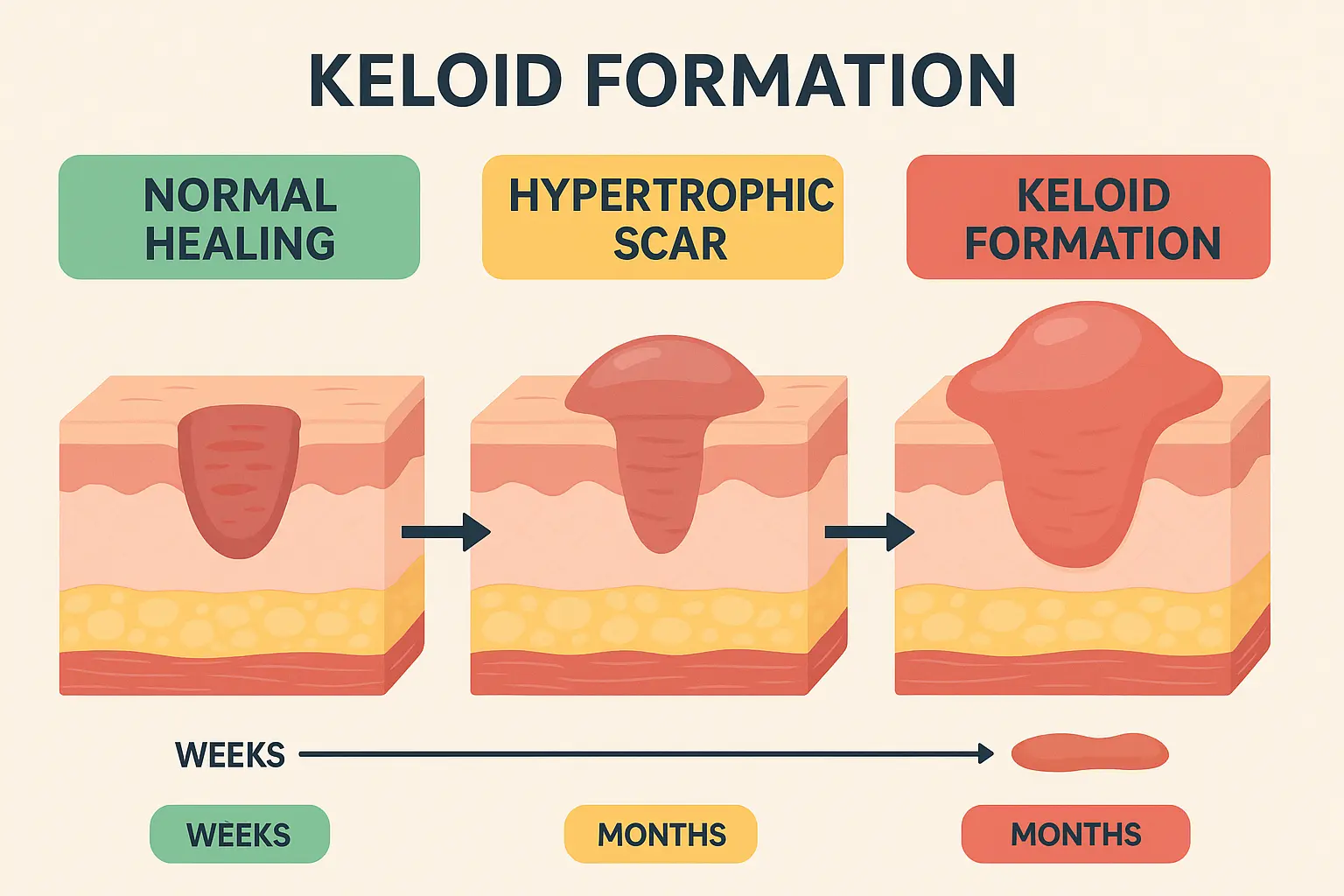
Keloids affect millions of people worldwide, with certain ethnic groups experiencing significantly higher rates of occurrence. Unlike normal scars that heal within the boundaries of the original wound, keloids continue growing beyond these limits, creating raised, often darkly pigmented tissue that can be both physically uncomfortable and psychologically challenging. The key to managing keloid-prone skin lies in proactive prevention strategies and comprehensive post-operative care protocols.
• Early intervention is crucial - Implementing prevention strategies before surgery significantly reduces keloid formation risk in susceptible individuals
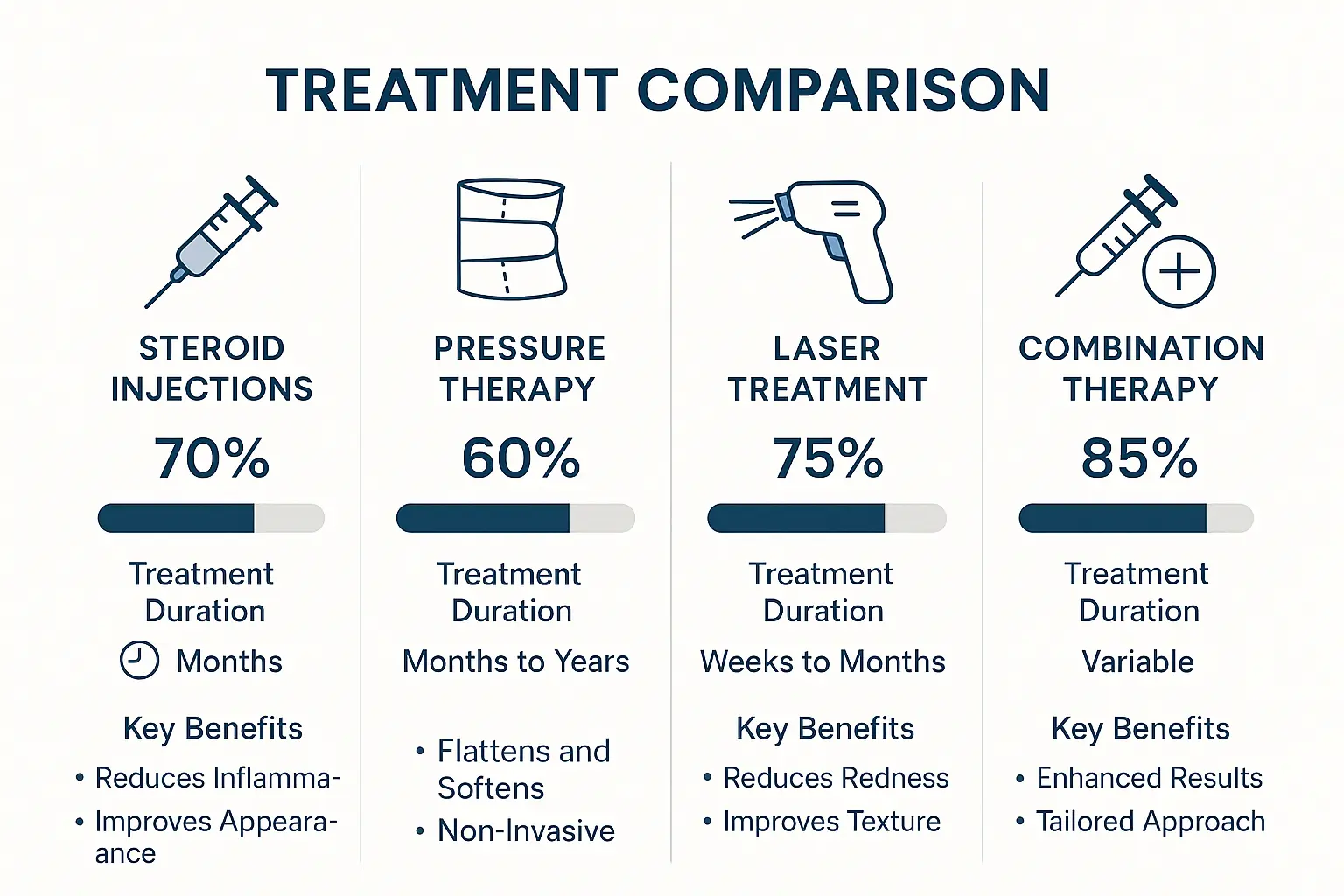
• Multi-modal treatment approaches work best, combining steroid injections, pressure therapy, and laser treatments for optimal results
• Patient education and compliance with post-operative care protocols directly impacts long-term scar outcomes
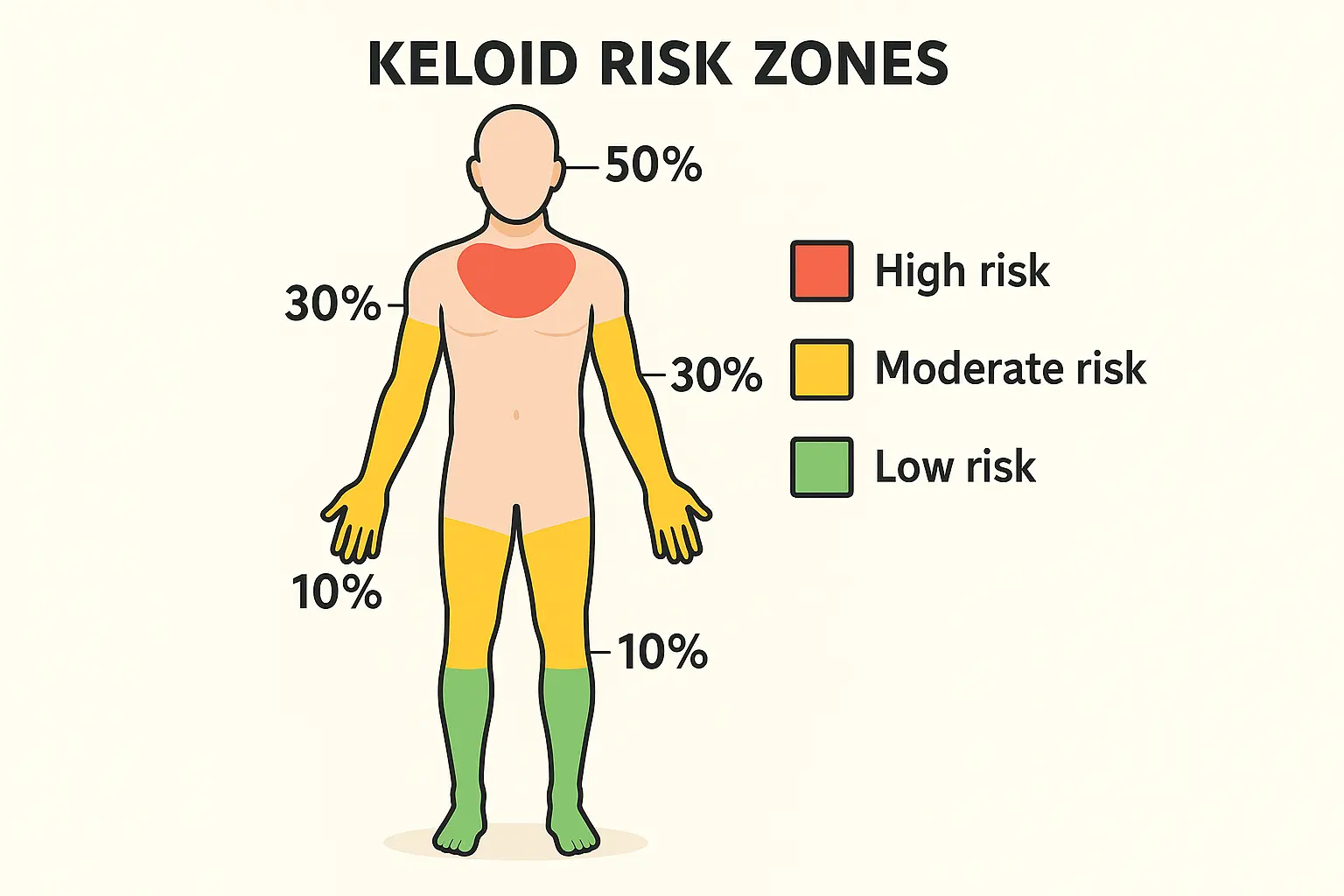
• Genetic predisposition and anatomical location are key factors that influence keloid development and treatment planning
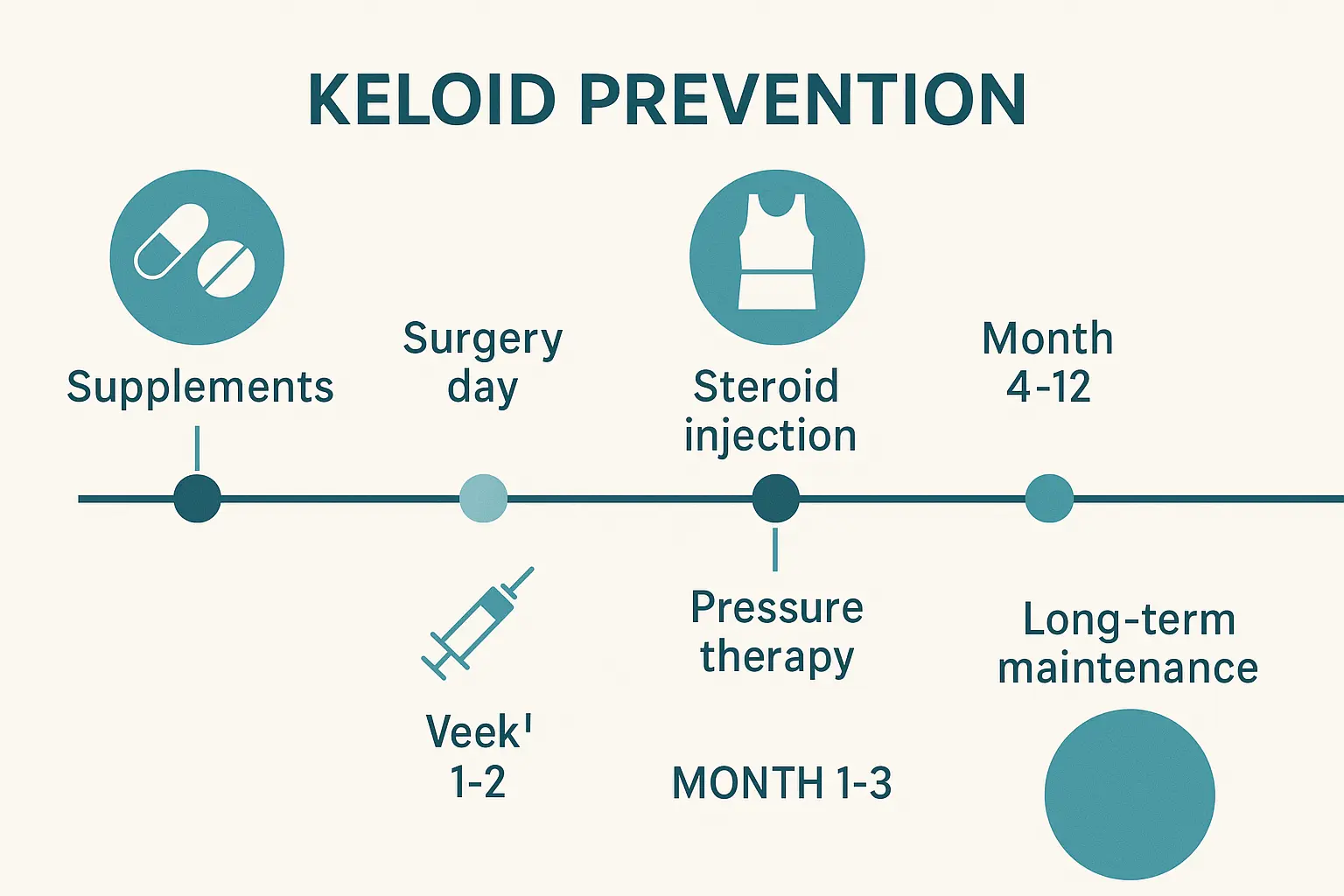
• Timing of interventions matters - starting preventive measures immediately after surgery yields better results than delayed treatment
Keloids represent an abnormal wound healing response characterized by excessive collagen production and deposition. Unlike hypertrophic scars, which remain within the original wound boundaries, keloids extend beyond the initial injury site and rarely regress spontaneously. The pathophysiology involves dysregulated fibroblast activity, increased transforming growth factor-beta (TGF-β) signaling, and altered collagen synthesis patterns.
Key cellular mechanisms include:
Understanding who is most susceptible to keloid formation helps surgeons and patients make informed decisions about surgical procedures and prevention strategies. Research consistently shows significant demographic and genetic patterns in keloid development.
Demographics at highest risk:
Certain body regions demonstrate higher propensity for keloid formation due to increased skin tension, movement patterns, and sebaceous gland density. Surgical planning must account for these anatomical risk factors when developing prevention strategies.
High-risk anatomical locations:
Lower-risk areas:
Before any surgical intervention, thorough evaluation of keloid risk factors enables personalized prevention planning. This assessment should encompass medical history, family history, previous scar formation patterns, and anatomical considerations specific to the planned procedure.
Essential assessment components:
Assessment AreaKey FactorsClinical SignificanceMedical HistoryPrevious keloids, autoimmune conditions, hormonal statusDetermines baseline risk levelFamily HistoryParental/sibling keloid history, ethnic backgroundIndicates genetic predispositionAnatomical SiteLocation, skin tension, mobilityInfluences surgical approachLifestyle FactorsAge, pregnancy status, medication useAffects healing response
For patients with keloid-prone skin, surgical technique modifications can significantly reduce the risk of abnormal scar formation. These adaptations focus on minimizing tissue trauma, optimizing wound closure, and reducing inflammatory responses.
Technical considerations include:
Certain medications and supplements can influence wound healing and collagen formation. Pre-operative optimization involves adjusting these factors to create the most favorable healing environment possible.
Beneficial pre-operative interventions:
The first 48-72 hours after surgery are critical for establishing proper healing patterns in keloid-prone individuals. Meticulous wound care during this period can significantly influence long-term scar outcomes.
Immediate care priorities:
Starting preventive treatments within the first week post-operatively has shown superior results compared to delayed intervention. Early protocols focus on modulating the inflammatory response and guiding collagen formation toward normal patterns.
Week 1-2 interventions:
Intralesional corticosteroid injections remain the first-line treatment for both prevention and treatment of keloids in high-risk patients. The anti-inflammatory and anti-proliferative effects of steroids directly address the underlying pathophysiology of keloid formation.
Triamcinolone acetonide protocols:
Expected outcomes with steroid therapy:
Continuous pressure application has demonstrated effectiveness in both preventing and treating keloid formation. The mechanism involves reducing blood flow to the scar tissue, decreasing oxygen tension, and promoting collagen remodeling toward normal patterns.
Pressure therapy guidelines:
Benefits of pressure therapy:
Modern laser technologies offer precise, targeted approaches to keloid management. Different laser types address various aspects of keloid pathophysiology, from vascular components to collagen remodeling.
Pulsed Dye Laser (PDL):
Fractional CO2 Laser:
Successful keloid management requires ongoing surveillance and maintenance therapy. Even successfully treated keloids can recur, making long-term follow-up essential for sustained results.
Follow-up schedule recommendations:
Research consistently demonstrates superior outcomes when multiple treatment modalities are combined rather than used in isolation. Synergistic effects between different treatments address the multifactorial nature of keloid pathophysiology.
Effective combination protocols:
Primary TreatmentSecondary TreatmentTertiary TreatmentSuccess RateSteroid InjectionsSilicone TherapyPressure Garments75-85%Laser TherapySteroid InjectionsTopical Treatments70-80%Surgical ExcisionImmediate SteroidsRadiation Therapy80-90%
Treatment success heavily depends on patient understanding and adherence to prescribed protocols. Comprehensive education programs improve compliance rates and long-term outcomes.
Key educational components:
Current research focuses on identifying new molecular targets for keloid prevention and treatment. Understanding the genetic and molecular basis of keloid formation opens possibilities for more targeted interventions.
Promising research areas:
Innovative drug delivery methods aim to improve treatment efficacy while reducing side effects. These systems provide sustained, localized therapy directly to keloid tissue.
Emerging delivery technologies:
Certain lifestyle factors can influence keloid formation risk and treatment outcomes. Addressing these modifiable factors provides additional prevention opportunities.
Beneficial lifestyle changes:
Environmental factors play significant roles in keloid development and progression. Understanding and modifying these exposures can improve prevention efforts.
Environmental risk factors:
Children and adolescents present unique challenges in keloid management due to ongoing growth, compliance issues, and psychological impacts. Treatment approaches must be modified for this population.
Pediatric-specific considerations:
Hormonal changes during pregnancy can significantly affect keloid formation and existing scar behavior. Special protocols are needed for pregnant patients with keloid-prone skin.
Pregnancy-related factors:
While generally safe, keloid treatments can occasionally result in complications requiring prompt recognition and management.
Common complications:
When initial treatment approaches fail to achieve desired outcomes, systematic evaluation and modified treatment strategies become necessary.
Failure analysis approach:
Understanding the economic impact of different keloid treatment approaches helps patients and healthcare systems make informed decisions about care strategies.
Cost considerations:
Coverage for keloid treatments varies significantly between insurance providers and treatment types. Understanding coverage patterns helps patients navigate treatment options.
Coverage factors:
Treatment recommendations for keloid-prone skin continue evolving based on emerging research and clinical trials. Staying current with evidence-based practices ensures optimal patient outcomes.
High-quality evidence supports:
Multiple research programs worldwide are investigating novel approaches to keloid prevention and treatment. These studies may provide future treatment options for patients with keloid-prone skin.
Active research areas:
Managing keloid-prone skin requires a comprehensive, proactive approach that begins with thorough risk assessment and continues through long-term maintenance strategies. The combination of proper pre-operative planning, immediate post-operative care, and evidence-based treatment modalities offers the best outcomes for patients susceptible to keloid formation.
Success in keloid management depends on several critical factors:
✅ Early identification of high-risk patients through comprehensive assessment
✅ Proactive prevention strategies implemented before and immediately after surgery
✅ Multi-modal treatment approaches combining steroid injections, pressure therapy, and laser treatments
✅ Patient education and compliance with long-term care protocols
✅ Regular monitoring and maintenance therapy to prevent recurrence
The landscape of keloid treatment continues evolving with advancing technologies and deeper understanding of keloid pathophysiology. Emerging therapies including targeted molecular treatments, advanced drug delivery systems, and regenerative medicine approaches offer hope for even better outcomes in the future.
For healthcare providers managing patients with keloid-prone skin, staying current with evidence-based practices while maintaining realistic expectations is essential. Success often requires patience, persistence, and willingness to adjust treatment approaches based on individual patient responses.
Patients with keloid-prone skin should work closely with experienced healthcare providers to develop personalized prevention and treatment strategies. Early intervention, consistent follow-up care, and adherence to prescribed treatments significantly improve the likelihood of achieving flat, aesthetically acceptable scars.
The investment in comprehensive keloid prevention and management strategies pays dividends in improved patient quality of life, reduced need for revision procedures, and better long-term aesthetic outcomes. As research continues advancing our understanding of keloid formation and treatment, the future holds promise for even more effective strategies to keep scars flat in keloid-prone individuals.