Picture this: you wake up one morning and notice a small, rough bump on your face that wasn't there before. While it might seem alarming, you're not alone—millions of people worldwide develop facial warts caused by the human papillomavirus (HPV). Understanding HPV on face manifestations can help you make informed decisions about treatment and prevention, ensuring you maintain both your health and confidence.
• HPV on face typically appears as common warts, flat warts, or filiform warts, each with distinct characteristics and treatment approaches
• Facial HPV is highly contagious and spreads through direct contact, making early identification and treatment crucial
• Multiple effective treatment options exist, from topical medications to professional removal procedures
• Prevention strategies, including proper hygiene and avoiding touching affected areas, significantly reduce transmission risk • Professional medical evaluation ensures accurate diagnosis and appropriate treatment selection for optimal outcomes
The human papillomavirus (HPV) represents one of the most common viral infections worldwide, with over 100 different strains identified by medical researchers. When HPV on face occurs, it typically results from specific low-risk HPV types that cause benign skin growths known as warts.
HPV belongs to a family of DNA viruses that specifically target epithelial cells—the cells that form the outer layer of skin and mucous membranes. Unlike high-risk HPV strains associated with cervical and other cancers, the types causing facial warts are generally harmless from a cancer perspective but can cause significant cosmetic and psychological concerns.
Common HPV types affecting facial skin include:
The virus enters the body through microscopic breaks in the skin barrier. These tiny openings can result from:
🔹 Minor cuts or scratches 🔹 Dry or cracked skin 🔹 Shaving-related micro-injuries 🔹 Existing skin conditions like eczema
Once inside, HPV hijacks normal cell reproduction processes, causing infected cells to multiply rapidly and form the characteristic raised, rough growths we recognize as warts.
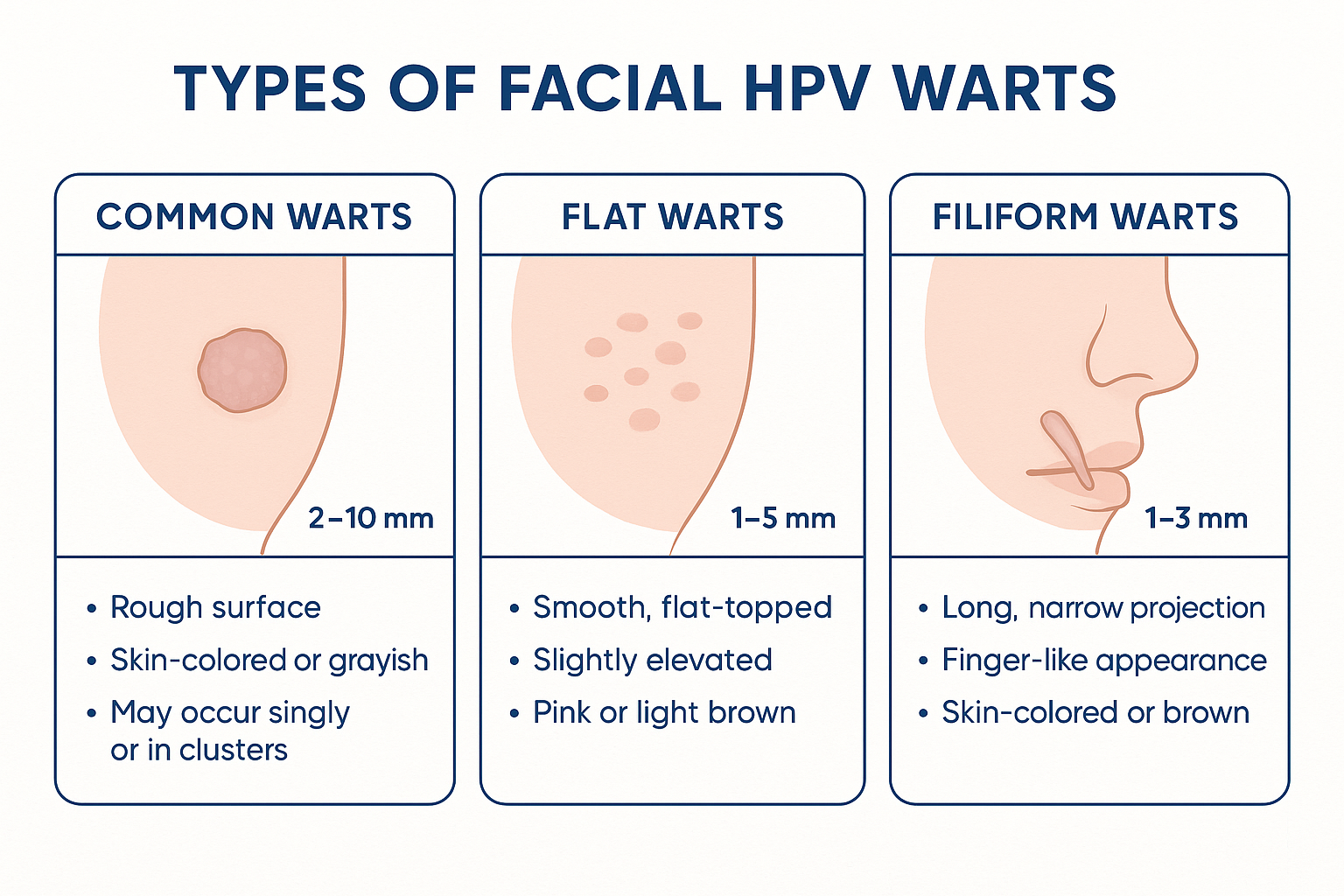
HPV on face manifests in several distinct forms, each with unique characteristics that help healthcare providers determine the most appropriate treatment approach. Understanding these differences empowers individuals to seek timely medical attention and make informed treatment decisions.
Common warts represent the most frequently encountered type of HPV on face, typically appearing on areas that experience regular trauma or contact.
Characteristics:
Flat warts present a more subtle appearance but can be particularly troublesome due to their tendency to appear in clusters.
Key features:
These distinctive warts have a unique finger-like appearance that makes them easily recognizable.
Identifying characteristics:
Recognizing HPV on face symptoms early enables prompt treatment and reduces the risk of spreading the infection to other areas or individuals. While facial warts share some common characteristics, each type presents unique identifying features that help distinguish them from other skin conditions.
The most obvious signs of HPV on face include visible changes to the skin's appearance:
Primary visual indicators:
While many facial warts are painless, some individuals may experience:
🔸 Mild itching or irritation 🔸 Tenderness when touched 🔸 Sensitivity during shaving or facial cleansing 🔸 Occasional bleeding if accidentally scratched or injured
HPV on face lesions often evolve over time, displaying:
Several skin conditions can mimic HPV on face symptoms, making professional evaluation important:
ConditionKey DifferencesSeborrheic KeratosisUsually larger, waxy appearance, more common in older adultsSkin TagsSoft, fleshy, attached by thin stalksMolesUsually darker, smoother surface, present from birth or early lifeAcneContains pus, responds to acne treatments, different distribution pattern
For accurate diagnosis and appropriate treatment recommendations, consider consulting with medical professionals who specialize in dermatological conditions.
Understanding transmission mechanisms helps individuals take appropriate preventive measures and avoid inadvertently spreading HPV on face to others or different body areas.
The primary method of HPV facial transmission occurs through direct skin-to-skin contact with infected individuals or contaminated surfaces.
Common transmission scenarios:
Many cases of HPV on face result from spreading the virus from other infected areas on the same person's body.
Self-spreading mechanisms: 🔹 Scratching or picking at warts on hands then touching the face 🔹 Shaving over infected areas and spreading virus through razor contact 🔹 Poor hand hygiene after touching warts elsewhere on the body 🔹 Using contaminated personal items like towels or washcloths
Certain conditions increase the likelihood of HPV transmission and facial infection:
Risk-enhancing factors:
After exposure to HPV, facial warts typically develop within:
Several factors increase an individual's susceptibility to developing HPV on face, ranging from personal habits to underlying health conditions. Recognizing these risk factors enables proactive prevention strategies and early intervention when necessary.
Certain age groups show higher susceptibility to HPV on face infections:
Children and adolescents:
Young adults:
Immune system strength directly correlates with HPV susceptibility and clearance rates.
Conditions affecting immune response: 🔸 HIV/AIDS significantly increases wart development risk 🔸 Organ transplant recipients taking immunosuppressive medications 🔸 Cancer patients undergoing chemotherapy or radiation 🔸 Autoimmune disorders like lupus or rheumatoid arthritis 🔸 Chronic stress leading to elevated cortisol levels
Certain professions and lifestyle choices elevate HPV on face risk:
High-risk occupations:
Lifestyle considerations:
Pre-existing skin conditions create favorable environments for HPV infection:
Predisposing skin conditions:
Understanding these risk factors helps individuals make informed decisions about prevention strategies and seek appropriate medical guidance when needed. For comprehensive evaluation of skin conditions and risk assessment, consider consulting with specialists who can provide personalized recommendations.

Accurate diagnosis of HPV on face requires professional medical evaluation to distinguish viral warts from other skin conditions and determine the most appropriate treatment approach. While some cases may seem straightforward, proper diagnosis ensures effective treatment and prevents unnecessary procedures.
Healthcare providers use several diagnostic approaches to identify HPV on face lesions:
Visual assessment includes:
Physical examination techniques: 🔹 Dermoscopy: Magnified examination revealing characteristic features 🔹 Palpation: Assessing texture and firmness 🔹 Comparative analysis: Examining similar lesions elsewhere on the body 🔹 Photography: Documenting baseline appearance for treatment monitoring
Medical professionals must distinguish HPV on face from various other conditions:
ConditionDistinguishing FeaturesDiagnostic TestsSeborrheic KeratosisWaxy, "stuck-on" appearanceVisual examination, dermoscopyBasal Cell CarcinomaPearly borders, central depressionBiopsy if suspiciousSquamous Cell CarcinomaRapid growth, ulcerationBiopsy requiredMolluscum ContagiosumCentral dimple, smooth surfaceClinical appearance
In uncertain cases, additional testing may be necessary:
Specialized diagnostic approaches:
Certain situations warrant immediate medical evaluation:
Red flag symptoms: 🚨 Rapid growth or size changes 🚨 Bleeding or ulceration 🚨 Pain or significant discomfort 🚨 Color changes to black or multiple colors 🚨 Irregular borders or asymmetry
Professional diagnosis ensures appropriate treatment selection and helps avoid complications from misidentified conditions. Healthcare providers specializing in dermatological conditions can provide comprehensive evaluation and treatment planning.
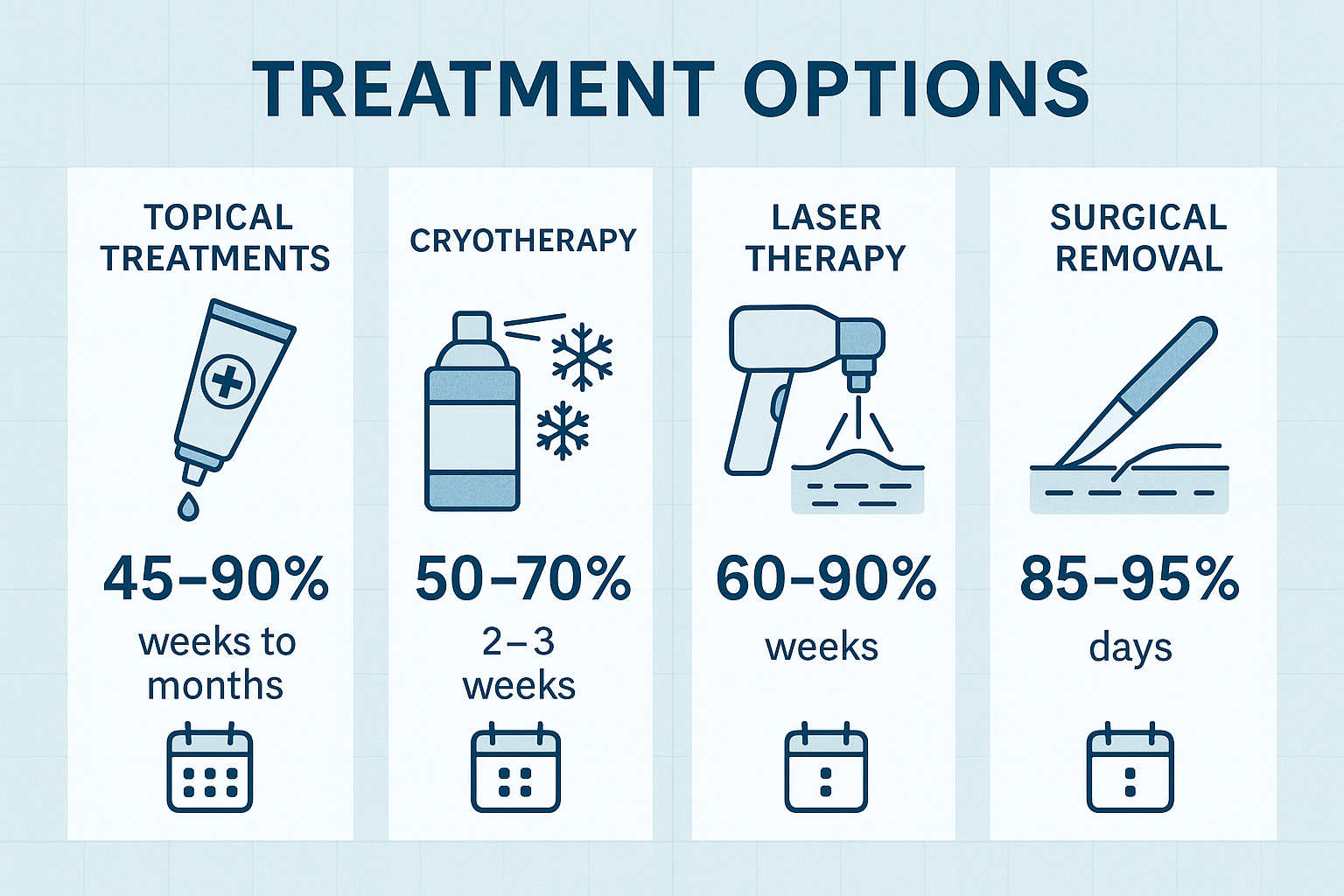
Treating HPV on face requires careful consideration of multiple factors, including wart type, size, location, and individual patient preferences. Modern medicine offers numerous effective treatment approaches, ranging from conservative topical therapies to advanced surgical procedures.
Topical medications represent the first-line treatment for many cases of HPV on face, offering convenience and minimal invasiveness.
Prescription topical options:
Imiquimod (Aldara):
Tretinoin:
5-Fluorouracil:
Several non-prescription treatments can effectively address HPV on face lesions:
Salicylic acid preparations: 🔸 Concentration: 17-40% for wart treatment 🔸 Application: Daily after soaking and filing 🔸 Duration: 4-12 weeks typically required 🔸 Precautions: Avoid contact with healthy skin
Cryotherapy kits:
Healthcare providers offer several advanced treatment options for stubborn or extensive HPV on face cases:
Cryotherapy (Liquid Nitrogen):
Electrosurgery:
Laser therapy:
Surgical excision:
For recurrent or treatment-resistant HPV on face cases, immunotherapy options may be considered:
Intralesional immunotherapy:
Oral immunomodulators:
The choice of treatment depends on various factors, and consultation with experienced healthcare providers ensures optimal outcomes. For comprehensive treatment planning and professional procedures, consider consulting with medical specialists who can evaluate individual cases and recommend the most appropriate approach.
While professional medical treatment remains the gold standard for HPV on face management, some individuals seek complementary natural approaches. Understanding both the potential benefits and limitations of home remedies helps people make informed decisions about their treatment journey.
Several natural treatments have shown promise in supporting HPV on face treatment, though scientific evidence varies:
Tea tree oil:
Garlic extract:
Apple cider vinegar:
Strengthening overall immune function may help the body naturally clear HPV on face infections:
Nutritional approaches: 🌟 Vitamin C: 1000-2000mg daily for immune support 🌟 Zinc: 15-30mg daily to enhance immune function 🌟 Vitamin E: Antioxidant support for skin health 🌟 Beta-carotene: Supports skin barrier function
Lifestyle modifications:
Traditional herbal medicine offers several options that some people find helpful:
Echinacea:
Calendula:
When considering home remedies for HPV on face, several safety factors require attention:
Potential risks: ⚠️ Skin irritation or allergic reactions ⚠️ Delayed professional treatment ⚠️ Incomplete viral clearance ⚠️ Scarring from inappropriate applications
Safety guidelines:
Many healthcare providers support integrating safe natural approaches with conventional treatment:
Complementary strategies:
For guidance on safe and effective treatment combinations, consider discussing options with healthcare professionals who can provide personalized recommendations based on individual circumstances.
Preventing HPV on face requires a comprehensive approach addressing both direct transmission prevention and overall immune system support. Implementing effective prevention strategies significantly reduces infection risk and helps maintain healthy, clear facial skin.
Maintaining excellent personal hygiene forms the foundation of HPV on face prevention:
Daily hygiene essentials: 🧼 Hand washing: Thorough washing with soap for 20+ seconds 🧼 Facial cleansing: Gentle daily cleansing with appropriate products 🧼 Clean towels: Using fresh, clean towels for face drying 🧼 Personal items: Avoiding sharing razors, towels, or makeup
Advanced hygiene strategies:
Understanding and avoiding high-risk scenarios significantly reduces HPV on face transmission probability:
Environmental precautions:
Social considerations:
A strong immune system provides the best defense against HPV on face infections:
Nutritional support:
NutrientDaily RecommendationFood SourcesVitamin C75-90mgCitrus fruits, berries, leafy greensVitamin D600-800 IUSunlight, fortified foods, supplementsZinc8-11mgMeat, nuts, seeds, legumesVitamin A700-900 RAEOrange vegetables, dark leafy greens
Lifestyle factors: 🏃 Regular exercise: 150 minutes moderate activity weekly 😴 Quality sleep: 7-9 hours nightly for immune recovery 🧘 Stress management: Meditation, yoga, relaxation techniques 🚭 Avoid smoking: Tobacco use weakens immune function 🍷 Limit alcohol: Excessive consumption impairs immunity
Maintaining healthy skin barriers prevents viral entry and reduces HPV on face risk:
Protective skin care:
Shaving safety:
Creating environments that discourage viral transmission supports prevention efforts:
Home environment:
Workplace considerations:
For additional prevention guidance and professional advice, healthcare providers can offer personalized recommendations based on individual risk factors and circumstances. Consider consulting with medical professionals for comprehensive prevention planning.
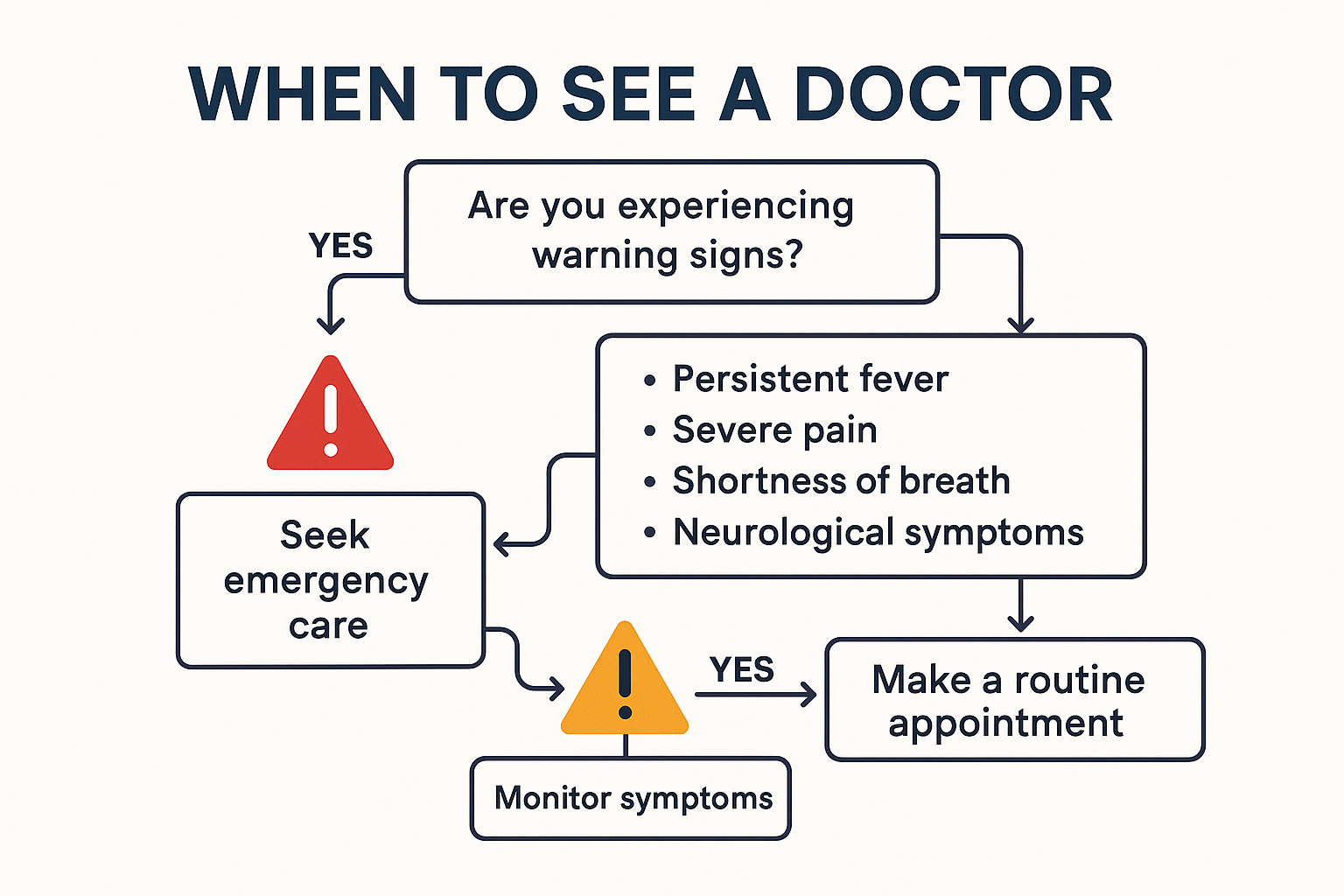
Recognizing when professional medical attention is necessary for HPV on face ensures timely, appropriate treatment and prevents potential complications. While some cases may resolve naturally, certain situations require immediate professional evaluation and intervention.
Several scenarios warrant urgent healthcare consultation for HPV on face concerns:
Emergency situations: 🚨 Rapid growth or size changes over days or weeks 🚨 Bleeding that doesn't stop with gentle pressure 🚨 Signs of infection including pus, red streaking, or fever 🚨 Severe pain or discomfort interfering with daily activities 🚨 Changes in color to black, blue, or multiple colors 🚨 Irregular borders or asymmetrical appearance
Many HPV on face situations benefit from professional assessment even without emergency symptoms:
Diagnostic clarity needs:
Treatment planning situations: 🔹 Large or numerous warts requiring professional intervention 🔹 Location concerns affecting facial expressions or function 🔹 Immune system compromise requiring specialized care 🔹 Occupational considerations for healthcare workers or food handlers 🔹 Psychological impact affecting self-esteem or social interactions
Individuals with diagnosed HPV on face should seek follow-up care in specific circumstances:
Follow-up indicators:
Certain groups require more careful monitoring and professional guidance:
High-risk populations:
Different types of healthcare providers offer varying expertise levels for HPV on face treatment:
Primary care providers:
Dermatologists:
Specialized surgical centers:
For comprehensive evaluation and treatment of facial skin conditions, consider consulting with experienced medical professionals who specialize in dermatological procedures and can provide personalized care recommendations.
Maximizing the value of healthcare consultations requires appropriate preparation:
Pre-appointment preparation: 📝 Symptom documentation: Timeline, changes, treatments tried 📝 Medical history: Previous skin conditions, immune system issues 📝 Medication list: Current prescriptions and supplements 📝 Questions list: Concerns about treatment options and outcomes 📝 Insurance information: Coverage verification for procedures
During the appointment:
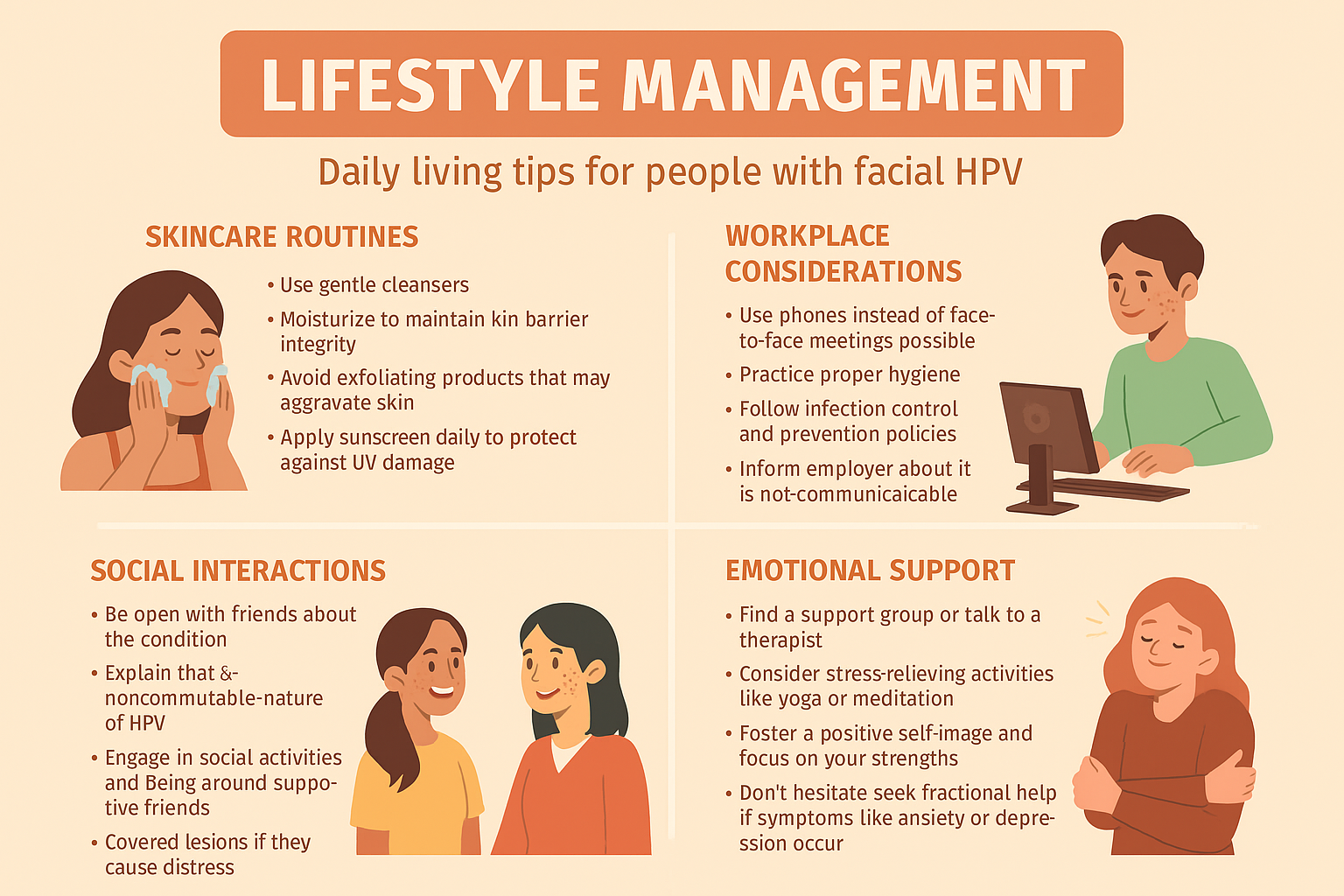
Managing HPV on face involves more than just medical treatment—it requires addressing the psychological, social, and practical aspects of living with a visible skin condition. Understanding how to navigate daily life while managing facial warts helps maintain quality of life and emotional well-being.
HPV on face can significantly affect self-esteem and emotional health, particularly when lesions are prominently visible:
Common emotional responses: 😔 Self-consciousness about appearance in social situations 😔 Anxiety about others' reactions or judgments 😔 Depression related to changes in self-image 😔 Frustration with treatment timelines and outcomes 😔 Embarrassment affecting social and professional interactions
Coping strategies:
Navigating social situations with HPV on face requires thoughtful approaches to communication and relationship management:
Disclosure considerations:
Communication strategies: 🗣️ Factual information: Sharing accurate medical information 🗣️ Reassurance: Explaining low transmission risk with proper precautions 🗣️ Boundary setting: Establishing comfortable interaction levels 🗣️ Education opportunity: Helping others understand HPV realities
Living with HPV on face requires attention to daily routines and practical considerations:
Skincare adaptations:
Activity modifications:
HPV on face may require workplace accommodations or considerations, particularly in certain professions:
Professional implications:
Legal protections:
Managing HPV on face often involves long-term health considerations and lifestyle adjustments:
Ongoing monitoring: 📊 Regular self-examinations for new lesions or changes 📊 Scheduled follow-up appointments with healthcare providers 📊 Treatment compliance with prescribed regimens 📊 Immune system support through healthy lifestyle choices 📊 Stress management to support overall health
Prevention of recurrence:
Creating strong support systems helps individuals manage the challenges of living with HPV on face:
Support resources:
For ongoing support and comprehensive care management, consider establishing relationships with healthcare providers who understand the multifaceted nature of living with dermatological conditions and can provide both medical treatment and emotional support guidance.
While HPV on face is generally benign, certain complications can arise that require careful monitoring and prompt medical attention. Understanding potential complications helps individuals recognize warning signs and seek appropriate care when necessary.
Several medical complications can develop from HPV on face infections or their treatments:
Infection-related complications: 🔴 Secondary bacterial infections from scratching or poor hygiene 🔴 Rapid spreading to other facial areas or body parts 🔴 Increased size or number indicating immune system compromise 🔴 Bleeding or ulceration suggesting tissue damage or malignant changes 🔴 Pain or discomfort interfering with daily activities
Treatment-related complications:
HPV on face can sometimes interfere with normal facial functions:
Physical function impacts:
The emotional impact of HPV on face can lead to significant psychological complications:
Mental health concerns: 😰 Social anxiety and withdrawal from social situations 😰 Depression related to altered self-image 😰 Body dysmorphic disorder with excessive focus on appearance 😰 Relationship difficulties affecting personal and professional connections 😰 Reduced quality of life impacting overall well-being
While uncommon, certain serious complications require immediate medical attention:
Malignant transformation:
Widespread dissemination:
Preventing complications from HPV on face involves proactive management and careful monitoring:
Preventive strategies: ✅ Proper hygiene to prevent secondary infections ✅ Gentle handling to avoid trauma and bleeding ✅ Professional treatment rather than self-removal attempts ✅ Regular monitoring for changes in appearance or symptoms ✅ Prompt medical attention for concerning developments
Treatment compliance:
Certain complications warrant immediate emergency medical attention:
Emergency indicators: 🚨 Severe bleeding that doesn't stop with pressure 🚨 Signs of systemic infection including fever, chills, red streaking 🚨 Sudden vision changes or severe eye pain 🚨 Difficulty breathing or swallowing 🚨 Severe allergic reactions to treatments
For comprehensive evaluation and management of complications related to facial skin conditions, consider consulting with specialized medical providers who have experience managing complex dermatological cases and can provide appropriate emergency and ongoing care.
Understanding common concerns about HPV on face helps individuals make informed decisions about prevention, treatment, and management. These frequently asked questions address the most common concerns patients and their families have about facial HPV infections.
Q: Is HPV on face contagious? A: Yes, HPV on face is highly contagious through direct contact. The virus can spread through touching infected areas and then touching other parts of your face or body, sharing personal items like towels or razors, or close contact with infected individuals. However, transmission can be significantly reduced through proper hygiene and precautionary measures.
Q: How long does it take for facial warts to appear after HPV exposure? A: The incubation period for HPV on face typically ranges from 2-6 months, though it can be as long as 2 years in some cases. Factors affecting this timeline include immune system strength, viral load at exposure, and individual susceptibility. Some people may never develop visible warts despite exposure.
Q: Can HPV on face cause cancer? A: The HPV types that typically cause HPV on face (common warts, flat warts, filiform warts) are low-risk strains that do not cause cancer. These are different from the high-risk HPV types associated with cervical and other cancers. However, any unusual changes in wart appearance should be evaluated by a healthcare provider.
Q: Will facial warts go away on their own? A: Some cases of HPV on face may resolve naturally as the immune system clears the infection. However, this process can take months to years, and there's no guarantee of spontaneous resolution. Treatment is often recommended to prevent spreading, reduce psychological impact, and achieve faster clearance.
Q: What's the most effective treatment for HPV on face? A: Treatment effectiveness varies by individual and wart characteristics. Professional treatments like cryotherapy, laser therapy, or prescription topical medications generally show higher success rates (70-95%) compared to over-the-counter options (50-70%). The best approach depends on wart size, location, number, and patient preferences.
Q: How long does treatment take? A: Treatment duration for HPV on face varies significantly:
Multiple treatment cycles may be necessary for complete clearance.
Q: How can I prevent spreading HPV to other parts of my face? A: Prevention strategies include: 🛡️ Avoid touching or picking at existing warts 🛡️ Wash hands thoroughly after any contact with affected areas 🛡️ Use separate towels for face and body 🛡️ Don't share personal care items 🛡️ Keep warts covered when possible 🛡️ Treat existing warts promptly to reduce viral load
Q: Can I wear makeup over facial warts? A: Makeup can be worn over HPV on face lesions, but precautions are important:
Q: Should I avoid social activities if I have HPV on face? A: HPV on face shouldn't prevent normal social activities. While the virus is contagious, transmission requires direct contact with infected areas. Maintaining good hygiene, avoiding sharing personal items, and being mindful of close contact can allow for normal social interaction while minimizing transmission risk.
Q: Can I exercise with facial warts? A: Exercise is generally safe with HPV on face, but consider these precautions:
Q: How do I explain my condition to others? A: Communication about HPV on face can be straightforward and educational:
For additional questions and personalized guidance about HPV on face, consider consulting with healthcare professionals who can provide specific answers based on individual circumstances and medical history.
Understanding HPV on face empowers individuals to make informed decisions about prevention, treatment, and management of this common skin condition. While facial warts can cause significant cosmetic and psychological concerns, the good news is that numerous effective treatment options exist, ranging from topical medications to advanced professional procedures.
The key to successful management lies in early recognition, appropriate treatment selection, and consistent prevention strategies. Whether dealing with common warts, flat warts, or filiform warts, working with experienced healthcare providers ensures optimal outcomes and minimizes the risk of complications or recurrence.
Essential action steps include:
✅ Seeking professional evaluation for accurate diagnosis and treatment planning
✅ Implementing prevention strategies to reduce transmission and recurrence risk
✅ Following treatment regimens consistently for best possible outcomes
✅ Maintaining realistic expectations about treatment timelines and results
✅ Addressing psychological impacts through appropriate support and counseling when needed
Remember that HPV on face is a manageable condition that affects millions of people worldwide. With proper care, most individuals can achieve complete clearance and return to normal activities without long-term complications. The combination of medical treatment, lifestyle modifications, and emotional support creates the foundation for successful management and improved quality of life.
For comprehensive evaluation and treatment of facial skin conditions, consider consulting with experienced medical professionals who can provide personalized care recommendations based on individual needs and circumstances. Taking proactive steps today leads to better outcomes and greater confidence in managing this treatable condition.