Did you know that your body contains over 600 lymph nodes, yet most people have never learned how to properly examine them? These small, bean-shaped structures serve as crucial checkpoints in your immune system, filtering harmful substances and fighting infections. Learning how to check your lymph nodes is an essential health skill that can help you detect changes early and maintain better awareness of your body's condition.
Lymph nodes can provide valuable insights into your health status. When they become swollen, tender, or change in consistency, they may signal anything from a minor infection to more serious health concerns. Understanding the proper technique for lymph node examination empowers you to take an active role in monitoring your health and knowing when to seek medical attention.
• Regular self-examination of lymph nodes helps detect changes early and promotes better health awareness
• Normal lymph nodes are typically small, soft, mobile, and painless when healthy
• Swollen lymph nodes often indicate your immune system is fighting an infection or responding to inflammation
• Proper examination technique involves using gentle pressure with fingertips in circular motions
• Medical consultation is necessary when lymph nodes remain enlarged for more than two weeks or show concerning characteristics
The lymphatic system represents one of the body's most important defense mechanisms. This complex network of vessels, nodes, and organs works tirelessly to protect against infections, maintain fluid balance, and support overall immune function.
Lymph nodes are small, oval-shaped structures that act as filters for lymphatic fluid. They contain immune cells called lymphocytes, which help identify and destroy harmful substances like bacteria, viruses, and abnormal cells. These nodes are strategically positioned throughout the body, with clusters located in areas where infections commonly occur.
Primary functions of lymph nodes include:
The lymphatic system consists of several key components working together:
ComponentFunctionLocationLymph vesselsTransport lymphatic fluidThroughout the bodyLymph nodesFilter fluid and fight infectionNeck, armpits, groin, chest, abdomenSpleenFilters blood and stores immune cellsLeft side of abdomenThymusProduces T-cellsBehind the breastboneTonsilsFirst line of defense against airborne pathogensThroat
Understanding where lymph nodes are located helps ensure thorough examination. The body contains several major lymph node groups, each serving specific regions and functions.
The head and neck contain numerous lymph node groups that drain different areas:
Cervical lymph nodes form the largest group in this region and include:
Other head and neck nodes include:
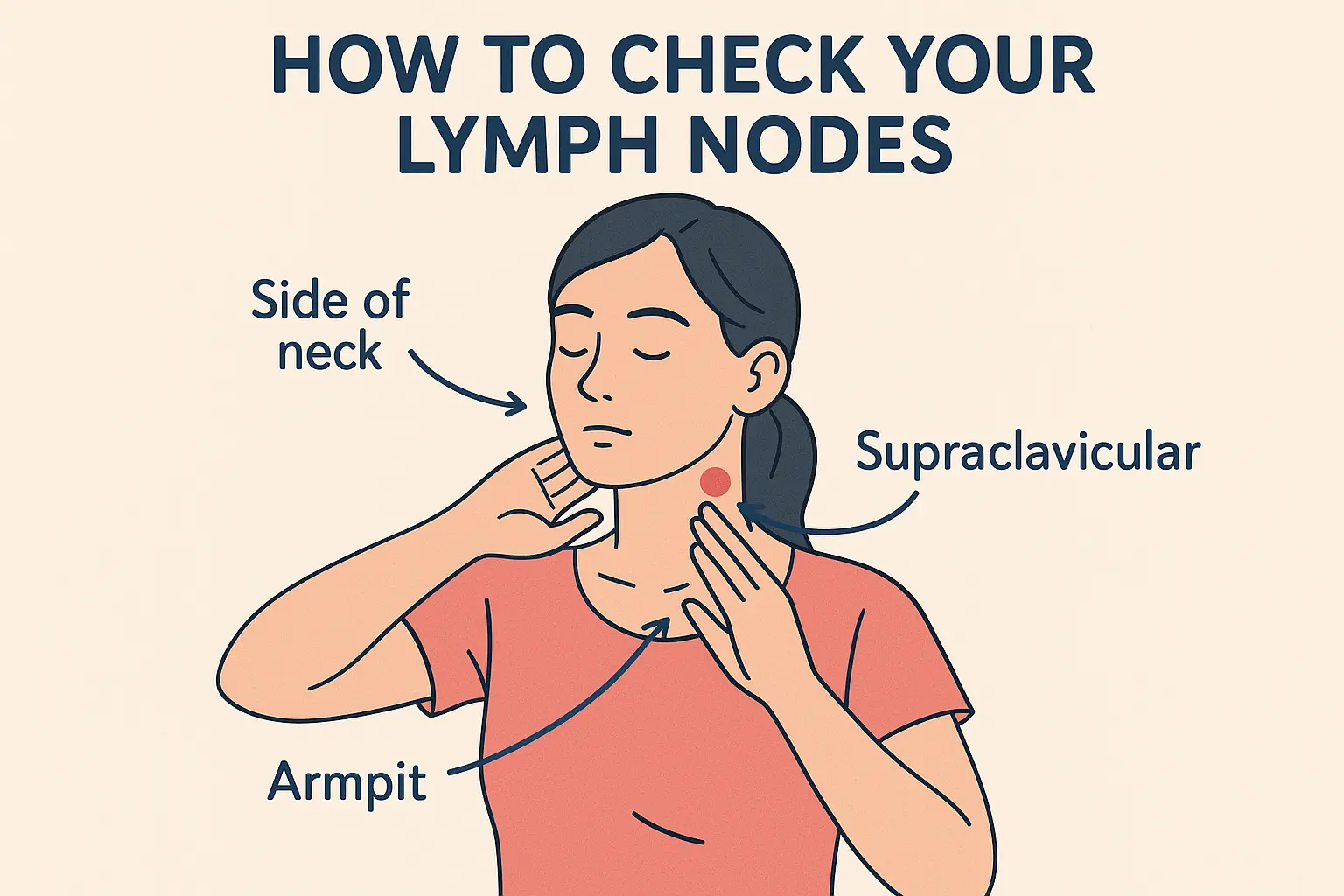
Axillary lymph nodes in the armpit area drain the arms, chest wall, and breast tissue. These nodes are particularly important for breast health monitoring and are divided into three levels based on their relationship to the pectoralis muscle.
Supraclavicular and infraclavicular nodes sit above and below the collarbone, respectively. These nodes can be significant because they may indicate conditions affecting the chest, lungs, or upper abdomen.
Inguinal lymph nodes in the groin area filter lymphatic fluid from the legs, lower abdomen, and pelvic region. These nodes are divided into superficial and deep groups.
Internal lymph nodes within the chest, abdomen, and pelvis cannot be felt during external examination but play crucial roles in filtering lymph from internal organs.
Learning to distinguish between normal and potentially concerning lymph node characteristics is essential for effective self-examination.
Healthy lymph nodes typically exhibit these characteristics:
Size: Usually less than 1 centimeter (about the size of a pea) Texture: Soft and somewhat rubbery Mobility: Move freely when gently pressed Pain: Generally painless to touch Shape: Oval or bean-shaped Consistency: Uniform throughout
💡 Important Note: Some people naturally have more prominent lymph nodes that can be felt even when healthy. This is particularly common in children and thin adults.
Certain characteristics may indicate the need for medical evaluation:
Size changes: Nodes larger than 1-2 centimeters or significant enlargement Texture changes: Hard, firm, or rubbery consistency Mobility issues: Fixed or immobile nodes that don't move when pressed Pain or tenderness: Especially when persistent Skin changes: Redness, warmth, or inflammation over the node Multiple affected areas: Swollen nodes in several locations simultaneously
Lymph nodes commonly swell in response to:
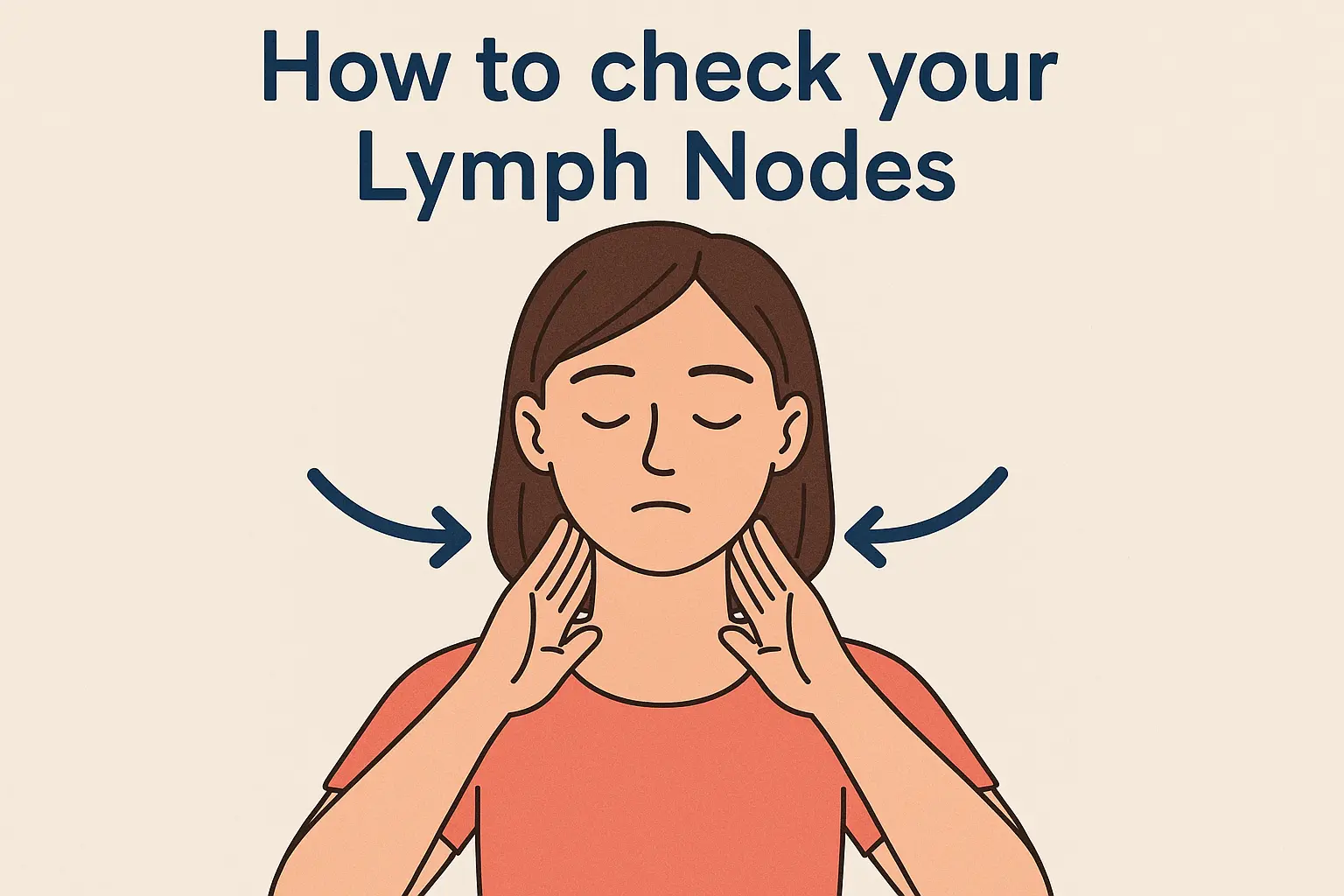
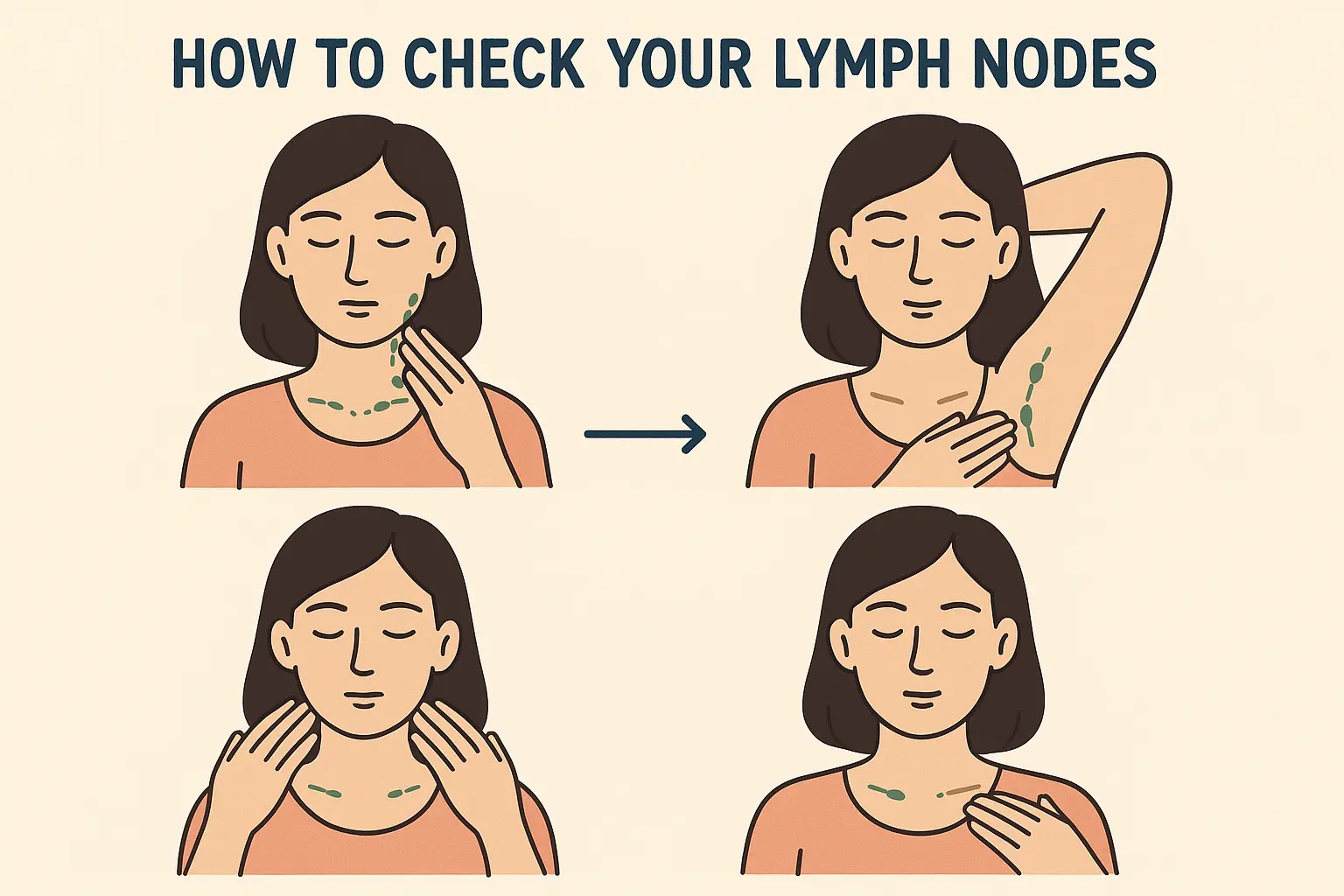
Proper lymph node examination requires systematic technique and gentle pressure. Following a consistent approach ensures thorough evaluation and helps establish baseline knowledge of your normal lymph node characteristics.
Before beginning your lymph node examination:
Choose the right environment: Find a quiet, well-lit space with a mirror Wash your hands: Clean hands prevent introducing bacteria during examination Remove jewelry: Take off necklaces, earrings, or other accessories that might interfere Relax: Tension can make lymph nodes more difficult to feel Use proper positioning: Sit or stand comfortably with good posture
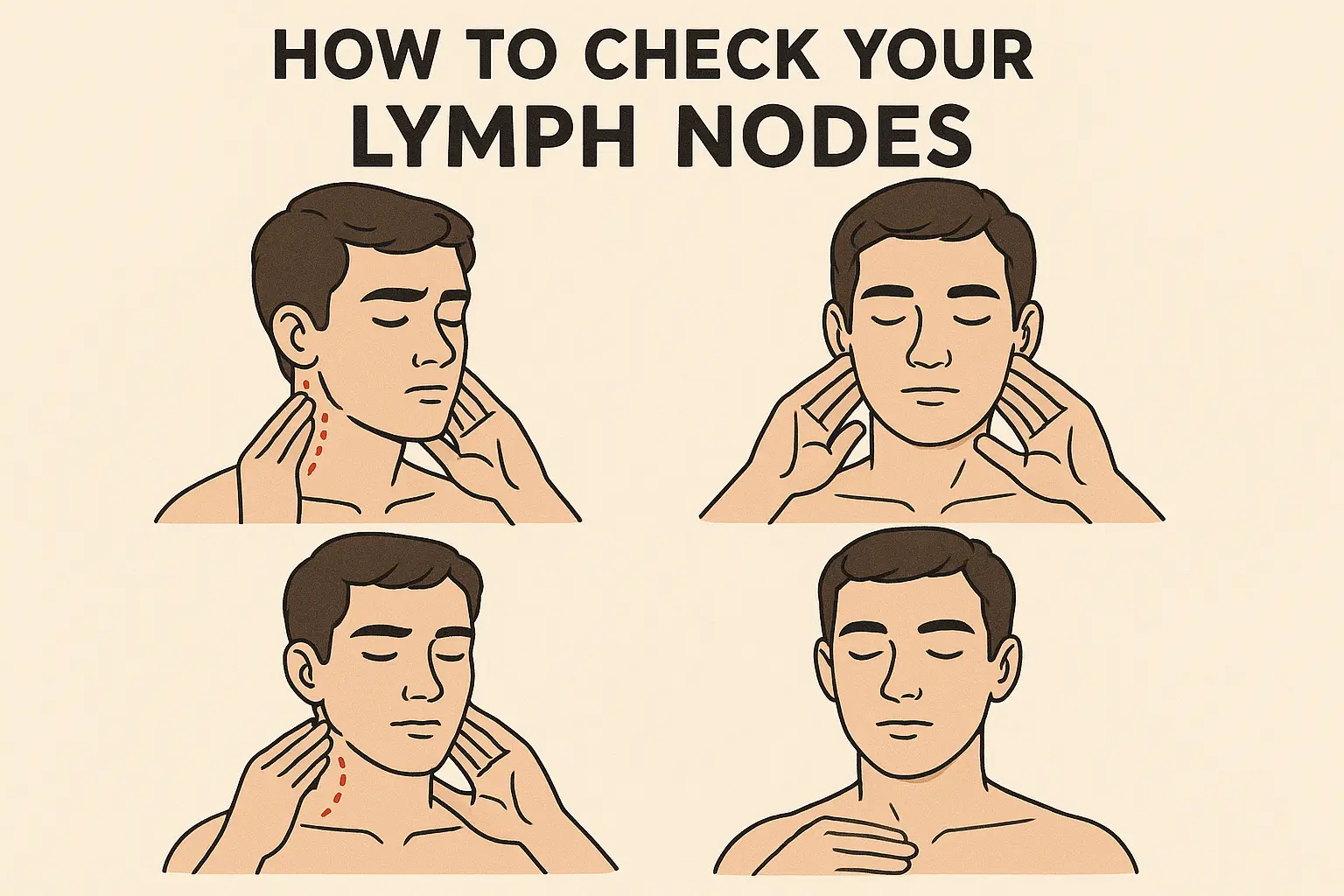
Hand positioning: Use the pads of your index, middle, and ring fingers rather than fingertips. This provides better sensitivity and prevents applying too much pressure.
Pressure application: Apply gentle, steady pressure using circular motions. The pressure should be firm enough to feel beneath the skin but not so hard as to cause discomfort.
Movement pattern: Move your fingers in small circles, gradually covering the entire area. Don't press too quickly or move your fingers too rapidly.
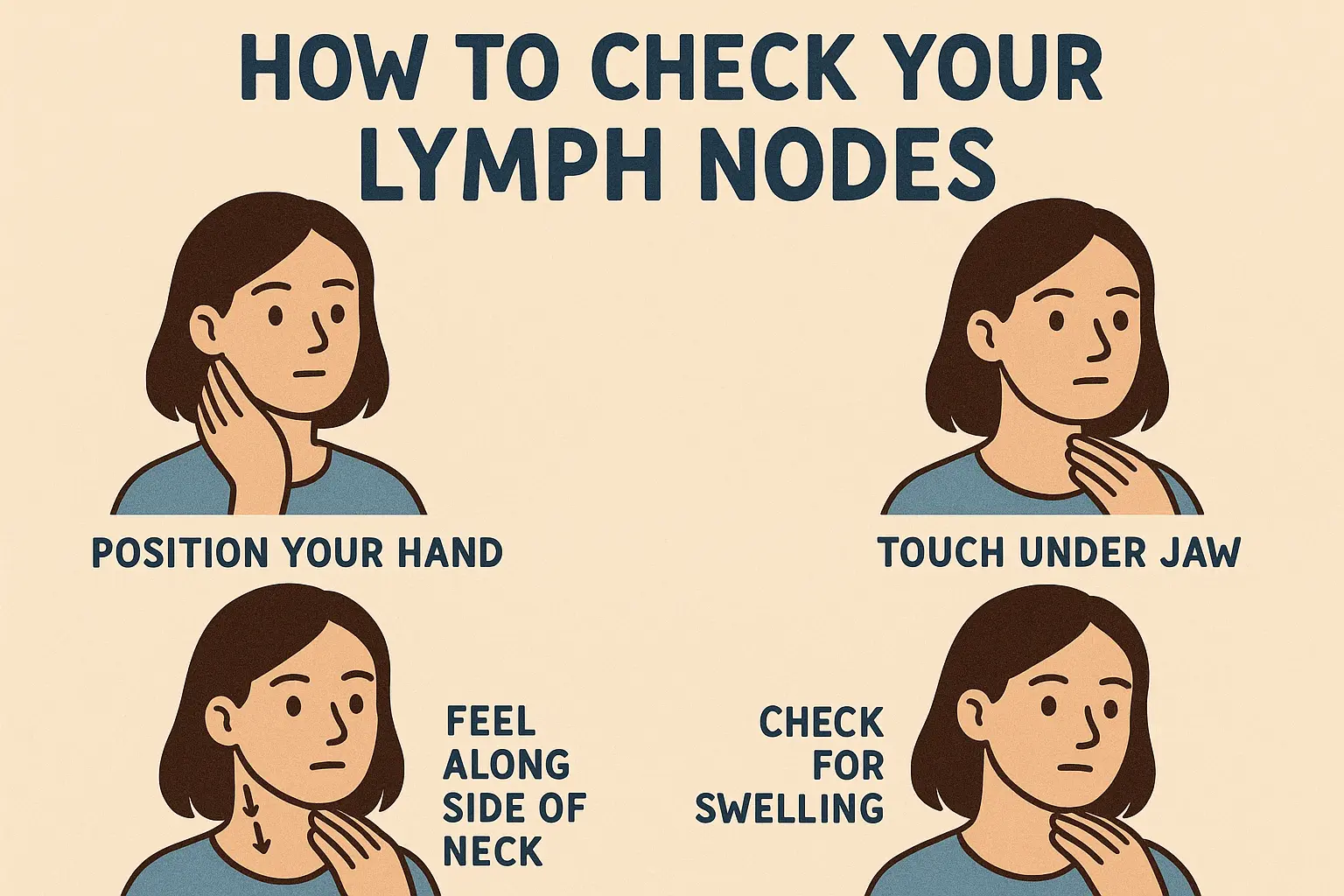
Step 1: Submental and Submandibular Nodes
Step 2: Cervical Chain Examination
Step 3: Posterior Cervical Nodes
Step 4: Supraclavicular Nodes
Positioning: Raise one arm slightly and support it with your opposite hand. This relaxes the muscles and makes nodes easier to feel.
Examination process:
Important considerations: Axillary examination can be challenging due to muscle tension. Practice relaxation techniques and gentle pressure application.
Positioning: Lie down or stand with legs slightly apart for better access.
Examination technique:
Effective lymph node examination involves understanding what normal variations feel like and recognizing potentially concerning changes.
Size fluctuations: Lymph nodes may vary in size throughout the day or during different times of the month. Hormonal changes, activity levels, and recent illnesses can all influence node size.
Asymmetry: It's normal for lymph nodes on one side to feel slightly different from the other side. Perfect symmetry is not expected.
Age-related changes: Children and young adults often have more easily palpable lymph nodes than older adults. This is normal and reflects active immune system development.
Soft and mobile: Normal lymph nodes feel somewhat like a grape or small bean that moves freely under the skin.
Firm but not hard: Healthy nodes have some resistance but aren't rock-hard or completely rigid.
Smooth surface: Normal lymph nodes have relatively smooth, regular surfaces without lumps or irregularities.
Understanding size parameters helps determine when lymph node enlargement warrants attention:
LocationNormal SizeConcerning SizeNeck< 1 cm> 1.5 cmArmpit< 1 cm> 2 cmGroin< 1.5 cm> 2 cmSupraclavicularNot palpableAny palpable node
Keep a simple record: Note the date, location, size (compare to familiar objects like peas or grapes), and any associated symptoms.
Track changes over time: Regular documentation helps identify patterns and provides valuable information for healthcare providers.
Photo documentation: Consider taking photos of any visible swelling for comparison over time.
Lymph node enlargement occurs for various reasons, ranging from minor infections to more serious conditions. Understanding common causes helps put findings into perspective and guides decisions about seeking medical care.
Upper respiratory infections represent the most common cause of cervical lymph node swelling. Cold viruses, flu, and bacterial throat infections frequently cause nodes in the neck to enlarge temporarily.
Skin infections can cause regional lymph node swelling. A cut, scrape, or insect bite that becomes infected may cause nearby lymph nodes to swell as they work to filter bacteria from the affected area.
Dental problems often cause submandibular and cervical lymph node enlargement. Tooth infections, gum disease, and dental procedures can trigger lymph node responses.
Systemic infections like mononucleosis (mono) can cause widespread lymph node swelling affecting multiple regions simultaneously.
Autoimmune conditions such as rheumatoid arthritis, lupus, and inflammatory bowel disease can cause chronic lymph node enlargement.
Allergic reactions to medications, foods, or environmental allergens may trigger lymph node swelling as part of the immune response.
Vaccination responses commonly cause temporary lymph node enlargement near injection sites. This is a normal immune system response and typically resolves within a few weeks.
Several medications can cause lymph node enlargement as a side effect:
Physical stress from intense exercise, illness, or injury can temporarily affect lymph node size and sensitivity.
Emotional stress may also influence immune system function and lymph node characteristics, though this connection is less well understood.
Sleep deprivation and poor nutrition can affect immune system function and potentially influence lymph node behavior.
While most lymph node changes are benign and temporary, certain characteristics warrant prompt medical evaluation. Recognizing these red flags ensures appropriate and timely medical care.
Rapidly enlarging nodes: Lymph nodes that double in size within days or weeks require urgent evaluation.
Very large nodes: Nodes larger than 2-3 centimeters (about the size of a walnut) should be evaluated promptly.
Hard, fixed nodes: Lymph nodes that feel rock-hard or don't move when pressed need immediate medical assessment.
Supraclavicular involvement: Any palpable lymph node above the collarbone requires prompt evaluation, as these may indicate serious conditions.
Associated systemic symptoms: Fever, night sweats, unexplained weight loss, or persistent fatigue accompanying lymph node enlargement warrant urgent medical attention.
Persistent enlargement: Lymph nodes that remain enlarged for more than 2-3 weeks without obvious cause should be evaluated.
Progressive symptoms: Gradually worsening lymph node enlargement or associated symptoms require medical assessment.
Multiple region involvement: Swollen lymph nodes in several different areas of the body simultaneously may indicate systemic conditions requiring evaluation.
Skin changes: Redness, warmth, or visible swelling over lymph nodes suggests possible infection requiring treatment.
Baseline documentation: If you have chronically enlarged but stable lymph nodes, discuss these with your healthcare provider during routine visits.
Family history concerns: Those with family history of lymphoma or other cancers should discuss lymph node monitoring strategies with their healthcare provider.
Occupational exposures: People with occupational exposures to chemicals, radiation, or infectious agents should maintain regular medical monitoring.
Developing effective self-examination habits maximizes the benefits of lymph node monitoring while avoiding unnecessary anxiety or missed findings.
Monthly examinations: Perform systematic lymph node examinations once monthly, ideally on the same date each month.
Consistent timing: Choose a time when you're relaxed and not rushed. Many people find bedtime or morning routines work well.
Avoid examination during illness: Skip routine examinations when you have active infections, as temporary lymph node changes are expected and may cause unnecessary concern.
Systematic approach: Always examine lymph node groups in the same order to ensure consistency and avoid missing areas.
Environmental consistency: Use the same lighting and mirror setup for each examination to improve detection of changes.
Relaxation techniques: Practice deep breathing or other relaxation methods before examination to reduce muscle tension and improve accuracy.
Simple recording system: Keep a basic log noting date, locations examined, and any findings. Smartphone apps or simple calendars work well.
Descriptive language: Use consistent terms to describe findings (size of pea, grape, walnut; soft, firm, hard; mobile, fixed).
Symptom tracking: Note any associated symptoms like sore throat, fatigue, or skin changes that might explain lymph node changes.
Excessive pressure: Pressing too hard can cause discomfort and make normal tissues feel abnormal. Use gentle, steady pressure.
Rushing the process: Thorough examination takes time. Allow 10-15 minutes for complete systematic evaluation.
Comparing to others: Everyone's baseline lymph node characteristics are different. Focus on changes from your own baseline rather than comparing to others.
Examination during tension: Muscle tension makes lymph nodes harder to feel and can create false impressions of abnormality.
When medical evaluation becomes necessary, understanding the process helps reduce anxiety and ensures effective communication with healthcare providers.
Medical history: Healthcare providers will ask about symptoms, timing of changes, recent illnesses, medications, travel history, and family medical history.
Physical examination: Doctors use systematic palpation techniques similar to self-examination but with greater experience and sensitivity.
Associated findings: Medical evaluation includes assessment of related organs, skin examination, and evaluation for systemic symptoms.
Blood tests: Complete blood count (CBC), inflammatory markers, and specific tests for infections or autoimmune conditions may be ordered.
Imaging studies: Ultrasound, CT scans, or MRI may be used to evaluate lymph node characteristics and surrounding structures.
Biopsy procedures: When necessary, tissue samples may be obtained through fine needle aspiration, core biopsy, or surgical excision.
Watchful waiting: Many lymph node changes are monitored over time without immediate intervention.
Serial examinations: Regular medical follow-up allows tracking of changes and early detection of concerning developments.
Treatment monitoring: When treatment is necessary, lymph node response often serves as an indicator of treatment effectiveness.
Several lifestyle factors influence lymphatic system function and lymph node health. Understanding these connections empowers better health choices and may improve overall lymphatic function.
Adequate hydration: Proper fluid intake supports lymphatic circulation and helps maintain normal lymph node function. Aim for 8-10 glasses of water daily.
Anti-inflammatory foods: Diets rich in fruits, vegetables, whole grains, and omega-3 fatty acids may support healthy immune function and reduce unnecessary inflammation.
Limit processed foods: Excessive processed foods, sugar, and unhealthy fats may contribute to chronic inflammation and affect immune system function.
Specific nutrients: Vitamin C, vitamin D, zinc, and selenium play important roles in immune system function and lymphatic health.
Regular exercise: Moderate physical activity supports lymphatic circulation, as the lymphatic system lacks a central pump like the cardiovascular system.
Lymphatic massage: Gentle massage techniques may help promote lymphatic drainage and reduce swelling in some situations.
Avoid prolonged immobility: Long periods of sitting or lying down may impair lymphatic circulation and contribute to fluid retention.
Quality sleep: Adequate sleep supports immune system function and may help maintain normal lymph node characteristics.
Stress reduction: Chronic stress may affect immune function and potentially influence lymph node behavior. Practice stress management techniques like meditation, yoga, or deep breathing.
Work-life balance: Maintaining reasonable work schedules and personal time supports overall health and immune system function.
Avoid smoking: Tobacco use impairs immune function and may affect lymphatic system health.
Limit alcohol: Excessive alcohol consumption can suppress immune function and affect lymph node responses.
Chemical exposures: Minimize exposure to unnecessary chemicals, pesticides, and environmental toxins when possible.
Lymph node characteristics and examination considerations vary across different age groups, requiring tailored approaches for optimal health monitoring.
Normal prominence: Children typically have more easily palpable lymph nodes than adults due to active immune system development and frequent exposure to new pathogens.
Rapid changes: Pediatric lymph nodes may change size more quickly than adult nodes in response to infections or other stimuli.
Examination approach: Children may need reassurance and gentle explanation during lymph node examination. Making it part of routine health awareness education can be beneficial.
Common causes: Upper respiratory infections, ear infections, and childhood illnesses frequently cause lymph node enlargement in pediatric populations.
Baseline establishment: Adults should establish their personal baseline lymph node characteristics and monitor for changes from this baseline.
Occupational considerations: Adults with certain occupations may have increased exposure risks requiring more vigilant monitoring.
Hormonal influences: Women may notice lymph node changes related to menstrual cycles, pregnancy, or hormonal medications.
Decreased prominence: Elderly individuals often have less easily palpable lymph nodes due to age-related changes in immune system function.
Medication effects: Older adults often take multiple medications that may affect lymph node characteristics or immune function.
Comorbid conditions: Other health conditions common in elderly populations may influence lymph node behavior or examination findings.
Increased vigilance: Some serious conditions affecting lymph nodes become more common with advancing age, warranting careful monitoring.
Modern technology offers various tools that can enhance lymph node monitoring and health tracking, though they should complement rather than replace proper examination techniques and medical care.
Health tracking apps: Smartphone applications can help maintain examination schedules, record findings, and track changes over time.
Symptom trackers: Apps that monitor associated symptoms like fever, fatigue, or pain can provide valuable context for lymph node changes.
Photo documentation: Smartphone cameras can document visible lymph node enlargement for comparison over time and communication with healthcare providers.
Calipers: Simple measuring tools can provide more accurate size documentation than visual estimation alone.
Flexible rulers: Soft measuring tapes can help document lymph node dimensions and track changes over time.
Reference objects: Using consistent reference objects (coins, beans, nuts) helps standardize size descriptions and improve communication with healthcare providers.
Online tutorials: Video demonstrations of proper examination techniques can supplement written instructions and improve examination quality.
Medical websites: Reputable medical websites provide updated information about lymph node health and when to seek medical attention.
Professional guidance: Healthcare provider demonstrations during routine visits can improve examination technique and confidence.
Several common myths and misconceptions about lymph nodes can lead to unnecessary anxiety or delayed medical care. Understanding accurate information helps make informed health decisions.
Myth: "Swollen lymph nodes always mean cancer" Reality: The vast majority of lymph node enlargement is due to benign causes like infections or inflammatory conditions. Cancer is a relatively uncommon cause of lymph node swelling.
Myth: "You should never touch or examine lymph nodes" Reality: Gentle self-examination is safe and beneficial for health monitoring. Proper technique does not cause harm or spread disease.
Myth: "Lymph nodes should never be felt in healthy people" Reality: Many healthy individuals can feel some lymph nodes, particularly in the neck and groin areas. This is often normal, especially in children and thin adults.
Myth: "Painful lymph nodes are more dangerous than painless ones" Reality: Actually, the opposite is often true. Painful lymph nodes frequently indicate infection or inflammation, while painless enlargement may be more concerning.
Age considerations: While lymph node problems can occur at any age, certain conditions are more common in specific age groups.
Family history: Having family members with lymph node or immune system disorders may increase risk but doesn't guarantee problems will develop.
Environmental factors: Occupational exposures, geographic location, and lifestyle factors may influence lymph node health but don't predetermine outcomes.
Timeline for changes: Most benign lymph node enlargement resolves within 2-6 weeks. Persistent enlargement beyond this timeframe warrants medical evaluation.
Treatment outcomes: When treatment is necessary, most lymph node conditions respond well to appropriate medical care.
Long-term monitoring: Some individuals may have chronically enlarged but stable lymph nodes that require periodic monitoring but no active treatment.
Developing confidence and competence in lymph node self-examination requires practice, education, and realistic expectations about findings and their significance.
Education reduces fear: Understanding normal lymph node characteristics and common causes of changes helps reduce anxiety about findings.
Practice builds confidence: Regular examination practice improves technique and familiarity with personal baseline characteristics.
Professional guidance: Having healthcare providers demonstrate proper technique and discuss findings provides reassurance and improves skills.
Start gradually: Begin with simple examination of easily accessible areas like the neck before progressing to more challenging regions.
Use systematic approach: Following the same examination sequence each time ensures consistency and completeness.
Seek feedback: Discuss examination techniques and findings with healthcare providers during routine visits to improve accuracy and confidence.
Focus on changes: Monitor for changes from personal baseline rather than comparing to others or seeking "perfect" normal findings.
Understand limitations: Self-examination is a screening tool, not a diagnostic procedure. It complements but doesn't replace professional medical care.
Balance vigilance with calm: Stay alert to concerning changes while maintaining reasonable perspective about the significance of minor variations.
Learning how to check your lymph nodes represents an important step in taking active responsibility for your health. This comprehensive guide has provided the knowledge and techniques necessary to perform effective lymph node self-examination, understand normal variations, and recognize when medical attention is needed.
Regular lymph node monitoring offers numerous benefits, including early detection of changes, increased body awareness, and improved communication with healthcare providers. The systematic examination techniques outlined in this guide, when performed monthly, can help establish personal baseline characteristics and identify significant changes that warrant medical evaluation.
Remember that most lymph node changes are temporary and benign, often resulting from common infections or inflammatory conditions. However, understanding the red flags that require prompt medical attention ensures appropriate care when needed. The key characteristics to monitor include persistent enlargement lasting more than two weeks, nodes larger than normal size guidelines, hard or fixed consistency, and associated systemic symptoms.
Take action today by scheduling your first systematic lymph node examination using the techniques described in this guide. Create a simple tracking system to document your findings, and discuss your examination routine with your healthcare provider during your next visit. Consider sharing this information with family members, as lymph node health awareness benefits everyone.
Building confidence in self-examination takes time and practice, but the investment in this health skill pays dividends in improved body awareness and peace of mind. By combining regular self-examination with appropriate medical care when needed, you can maintain optimal lymphatic health and contribute to your overall wellness strategy.
The lymphatic system serves as a crucial component of immune function, and understanding how to monitor its health empowers better health decisions throughout life. Whether you're establishing a new health routine or enhancing existing practices, proper lymph node examination skills represent valuable additions to your health toolkit.