When cancer cells from melanoma spread to the brain, they create a race against time that no patient or family wants to face. The speed at which melanoma brain tumors grow can determine treatment options, quality of life, and ultimately, survival outcomes. Understanding this aggressive form of metastatic cancer becomes crucial for anyone dealing with advanced melanoma.
Melanoma brain metastases represent one of the most challenging complications in cancer care. Unlike primary brain tumors that originate in brain tissue, these secondary tumors arrive as unwelcome visitors from melanoma elsewhere in the body. The question of growth rate isn't just academic—it directly impacts treatment decisions, prognosis discussions, and the precious time families have to make critical healthcare choices.
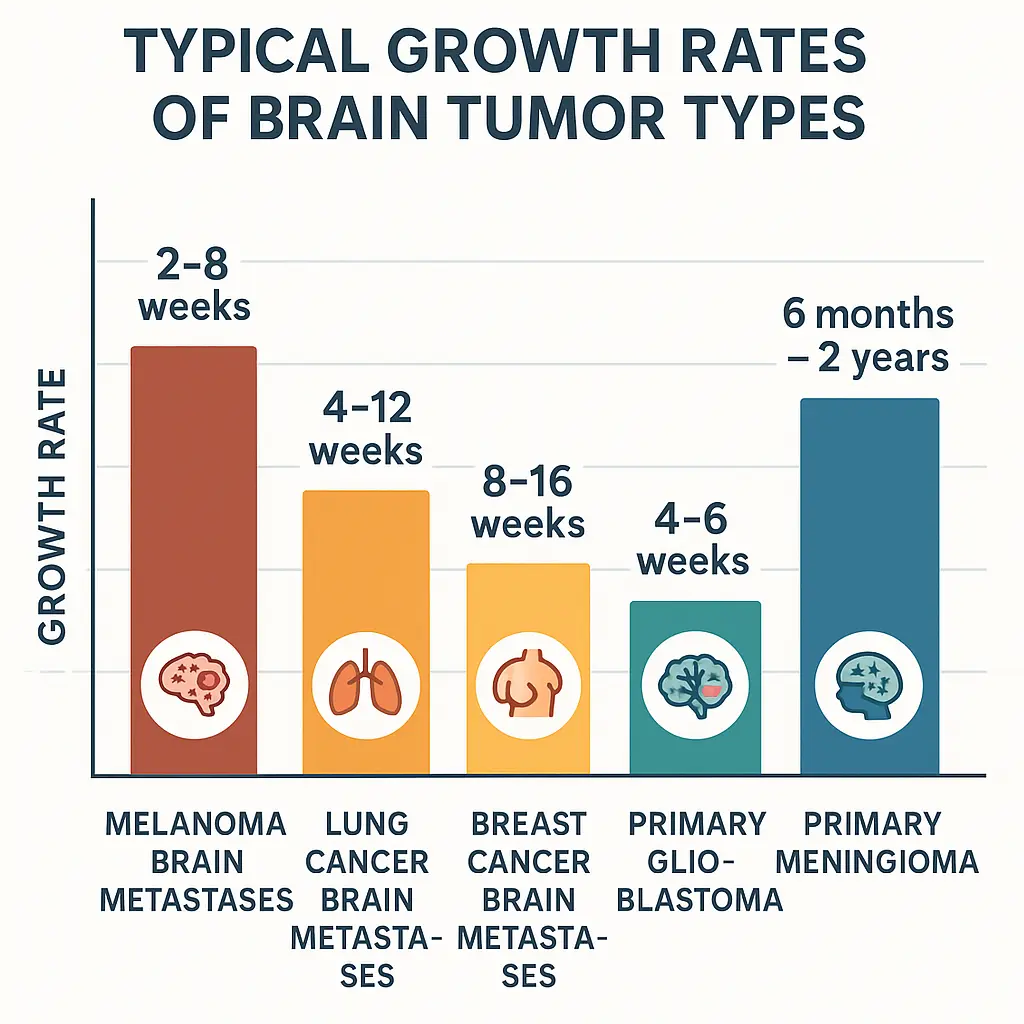
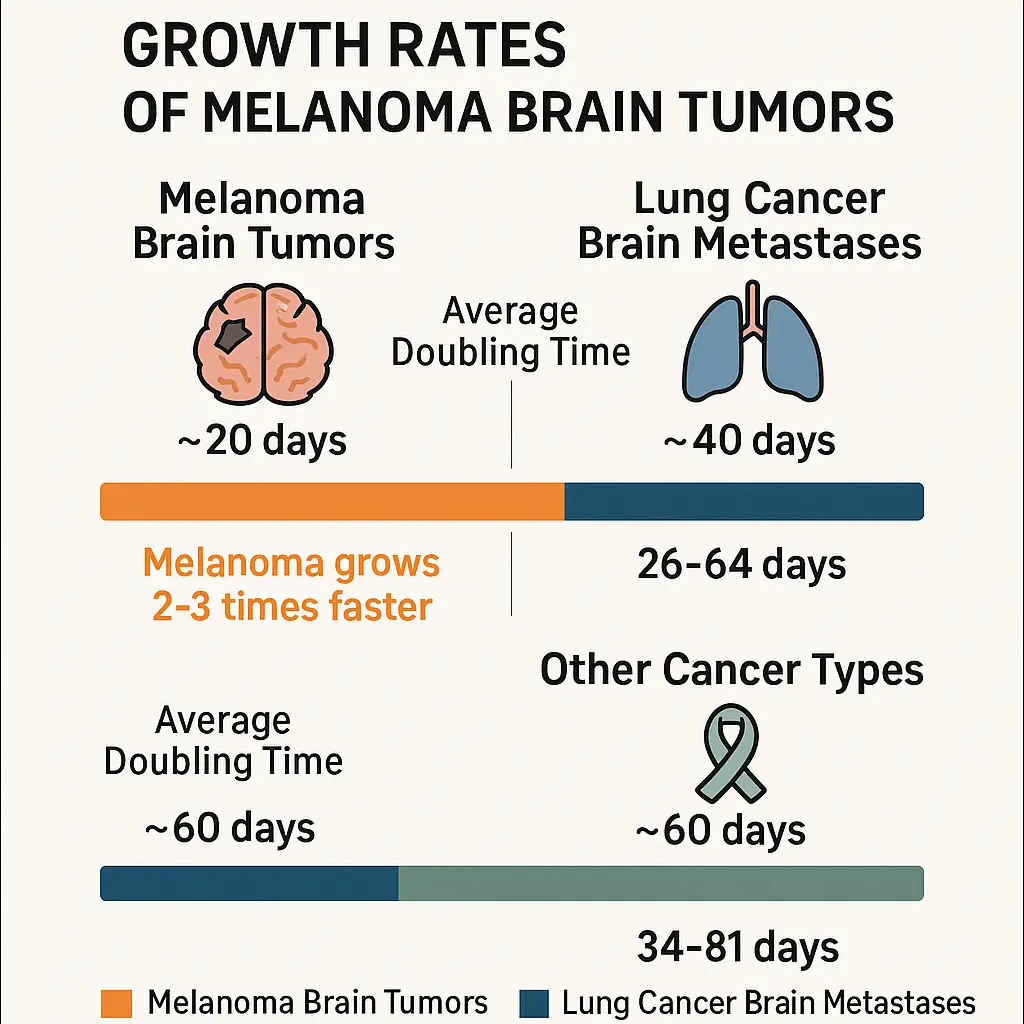
• Melanoma brain tumors typically grow rapidly, with doubling times ranging from 2-8 weeks, making them among the fastest-growing brain metastases
• Growth rates vary significantly based on tumor genetics, location, patient immune response, and previous treatments received
• Early detection and immediate treatment are critical since rapid growth can quickly cause neurological symptoms and complications
•Modern treatment options including immunotherapy, targeted therapy, and stereotactic radiosurgery have improved outcomes for patients with melanoma brain metastases
• Regular monitoring with brain MRI is essential for melanoma patients, as brain metastases can develop even years after initial diagnosis
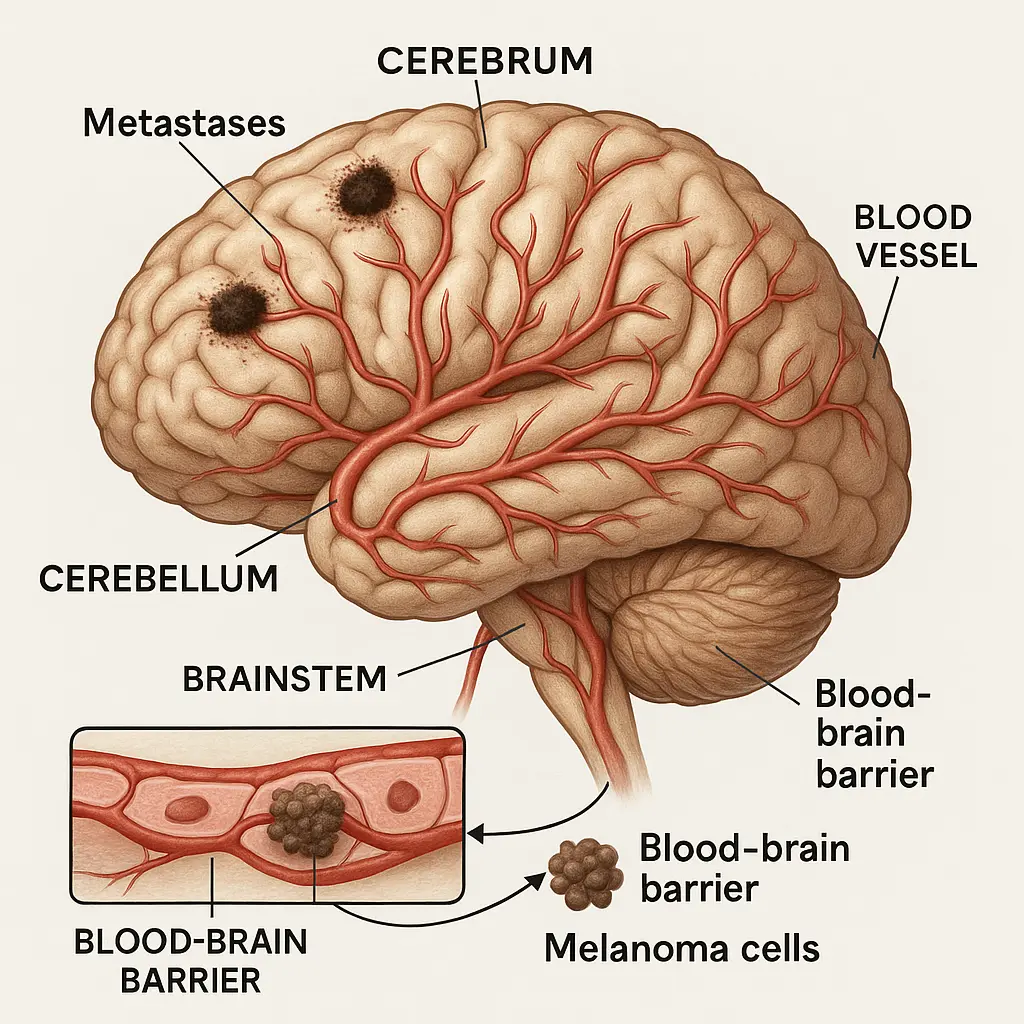
Melanoma brain tumors, medically known as melanoma brain metastases, occur when melanoma cancer cells travel through the bloodstream and establish new growth sites within the brain tissue. These secondary tumors maintain the characteristics of the original melanoma, including their aggressive growth patterns and resistance to certain treatments.
The brain provides a unique environment for cancer growth. Protected by the blood-brain barrier, it creates both challenges and opportunities for cancer cells. While this barrier initially protects against many cancer treatments, once melanoma cells breach this defense, they often find the brain's rich blood supply and supportive environment conducive to rapid multiplication.
Statistics paint a sobering picture:
Several factors make the brain a common destination for melanoma metastases. The brain receives approximately 20% of the body's blood flow, creating numerous opportunities for circulating cancer cells to lodge in brain capillaries. Additionally, certain molecular characteristics of melanoma cells show particular affinity for brain tissue.
Research has identified specific genetic mutations in melanoma that increase the likelihood of brain metastases. Tumors with BRAF mutations, NRAS mutations, or loss of PTEN function demonstrate higher rates of central nervous system spread. Understanding these molecular factors helps medical teams at specialized facilities like The Minor Surgery Center assess risk and develop appropriate monitoring strategies.
The growth rate of melanoma brain tumors ranks among the most aggressive of all brain metastases. Medical literature consistently documents rapid progression, with tumor volume doubling times typically occurring within 2-8 weeks. This accelerated growth pattern distinguishes melanoma brain metastases from other types of brain tumors, including many primary brain cancers.
Multiple variables affect how fast melanoma brain tumors grow, creating significant variation between individual cases. Understanding these factors helps patients and families prepare for the journey ahead while working with their medical teams to optimize treatment approaches.
🔬 Tumor Biology Factors:
🏥 Patient-Related Factors:
📍 Tumor Location Factors:
The rapid growth rate of melanoma brain tumors means symptoms often develop quickly and progress aggressively. Early recognition of neurological changes can be life-saving, allowing for immediate medical intervention before tumors grow large enough to cause irreversible damage.
🧠 Neurological Symptoms by Category:
Cognitive and Mental Changes:
Physical Symptoms:
Seizure Activity:
Given how fast melanoma brain tumors grow, symptom progression typically follows a compressed timeline compared to slower-growing brain tumors. Patients and caregivers should understand that neurological symptoms may worsen rapidly, sometimes over days rather than weeks or months.
Typical Progression Pattern:
This aggressive timeline underscores the importance of immediate medical evaluation for any new neurological symptoms in melanoma patients. Healthcare providers specializing in cancer conditions emphasize that early intervention dramatically improves treatment outcomes.
Accurate assessment of how fast melanoma brain tumors grow requires sophisticated imaging techniques that can detect small lesions and monitor changes over time. Modern neuroimaging provides detailed information about tumor size, location, and characteristics that guide treatment decisions.
🔍 Primary Imaging Modalities:
Magnetic Resonance Imaging (MRI):
Computed Tomography (CT):
Advanced Imaging Techniques:
Regular imaging surveillance allows medical teams to calculate actual growth rates for individual tumors, providing crucial information for treatment planning. Serial MRI scans performed at consistent intervals create a timeline that reveals how fast specific melanoma brain tumors grow in each patient.
Growth Measurement Parameters:
Surgical removal represents the most direct approach to stopping melanoma brain tumor growth, particularly for accessible lesions that haven't spread extensively. Modern neurosurgical techniques allow for precise tumor removal while preserving critical brain functions.
🔧 Surgical Considerations:
Ideal Candidates for Surgery:
Surgical Techniques:
Expected Outcomes:
Radiation therapy offers precise tumor control for melanoma brain metastases, with modern techniques allowing high-dose delivery while sparing healthy brain tissue. The choice between different radiation approaches depends on tumor number, size, and location.
⚡ Radiation Treatment Options:
Stereotactic Radiosurgery (SRS):
Whole Brain Radiation Therapy (WBRT):
Fractionated Stereotactic Radiotherapy:
The development of effective systemic therapies has revolutionized treatment for melanoma brain metastases. These medications can cross the blood-brain barrier and slow or stop tumor growth throughout the brain and body simultaneously.
💊 Systemic Treatment Categories:
Immunotherapy Options:
Targeted Therapy:
Combination Approaches:
Understanding prognosis helps patients and families make informed decisions about treatment goals and life planning. While individual outcomes vary significantly, statistical data provides important context for discussions with healthcare teams.
📈 Survival Outcomes by Treatment:
Treatment ApproachMedian Survival1-Year SurvivalNo treatment1-2 months<5%Surgery alone6-12 months35-50%Radiation alone4-8 months25-40%Combined treatment8-20 months40-70%Modern systemic therapy12-24 months50-80%
Multiple factors influence survival outcomes for patients with melanoma brain metastases. Understanding these variables helps medical teams develop realistic treatment plans and helps families prepare for the journey ahead.
🎯 Favorable Prognostic Factors:
⚠️ Challenging Prognostic Factors:
Managing quality of life becomes paramount when dealing with rapidly growing melanoma brain tumors. The aggressive nature of these tumors means that maintaining function and comfort requires proactive planning and comprehensive supportive care.
🏠 Daily Life Management:
Cognitive Support:
Physical Adaptations:
Emotional Support:
Family members and caregivers play crucial roles in supporting patients with melanoma brain metastases. The rapid progression potential of these tumors means caregivers need access to education, support, and practical resources.
👥 Caregiver Support Elements:
Healthcare facilities like The Minor Surgery Center team often provide comprehensive support resources for families dealing with complex medical conditions.
The rapid advancement in melanoma treatment research offers hope for improved outcomes in brain metastases. Current clinical trials are investigating novel approaches that may slow tumor growth or provide better symptom control.
🔬 Promising Research Areas:
Novel Immunotherapies:
Advanced Targeted Therapies:
Innovative Radiation Techniques:
Participation in clinical trials may provide access to cutting-edge treatments that could slow melanoma brain tumor growth or improve quality of life. Patients should discuss trial eligibility with their oncology teams.
Trial Considerations:
While preventing melanoma brain metastases isn't always possible, understanding risk factors helps guide monitoring strategies and early intervention approaches. Certain patient and tumor characteristics increase the likelihood of brain involvement.
🎯 High-Risk Factors for Brain Metastases:
Regular monitoring allows for early detection of brain metastases when tumors are smaller and more treatable. Surveillance protocols vary based on individual risk factors and institutional guidelines.
📅 Monitoring Recommendations:
High-Risk Patients:
Standard-Risk Patients:
Healthcare providers at specialized clinics often develop individualized surveillance plans based on patient risk factors and preferences.
Managing melanoma brain metastases requires coordination among multiple medical specialties. The rapid growth potential of these tumors makes efficient communication and quick decision-making essential.
👨⚕️ Essential Team Members:
Given how fast melanoma brain tumors grow, treatment goals must be clearly defined and regularly reassessed. Goals may evolve as the disease progresses or as new treatment options become available.
🎯 Potential Treatment Goals:
Curative Intent:
Palliative Intent:
Shared Decision-Making Elements:
Patients and families facing melanoma brain metastases often have urgent questions about prognosis, treatment options, and what to expect. Addressing these concerns helps reduce anxiety and improves treatment compliance.
❓ Frequently Asked Questions:
Q: How quickly will symptoms worsen? A: Symptom progression varies significantly, but melanoma brain tumors can cause noticeable changes within weeks. Regular monitoring and prompt treatment adjustments help manage symptoms effectively.
Q: Can melanoma brain tumors shrink with treatment? A: Yes, modern treatments including immunotherapy, targeted therapy, and radiation can shrink melanoma brain metastases in many patients. Response rates vary by treatment type and individual factors.
Q: Should I stop all other activities? A: Activity modifications depend on specific symptoms and tumor locations. Many patients continue meaningful activities with appropriate safety precautions and support.
Q: How do I prepare my family? A: Open communication, advance planning, and access to support resources help families navigate this challenging journey. Consider involving social workers or counselors in these discussions.
For additional questions and concerns, patients can often find helpful information through FAQ resources provided by specialized medical centers.
The aggressive nature of melanoma brain metastases requires specialized expertise and rapid access to advanced treatments. Patients should seek care at centers with experience managing complex brain metastases.
🏥 Characteristics of Quality Care Centers:
Staying informed about melanoma brain metastases helps patients and families make better decisions and cope with the challenges ahead. Reliable educational resources provide current, accurate information.
📚 Recommended Information Sources:
The rapid progression potential of melanoma brain tumors makes timely financial and legal planning essential. Families should address these issues early while patients can participate in decisions.
💰 Important Planning Elements:
Understanding how fast melanoma brain tumors grow provides crucial context for patients, families, and healthcare teams facing this challenging diagnosis. With typical doubling times of 2-8 weeks, melanoma brain metastases rank among the most aggressive brain tumors, requiring immediate attention and expert care.
The rapid growth rate of these tumors creates both urgency and opportunity. While the aggressive nature demands quick decision-making and prompt treatment initiation, advances in immunotherapy, targeted therapy, and radiation techniques have dramatically improved outcomes for many patients. Early detection through appropriate surveillance, combined with multidisciplinary treatment approaches, offers the best chance for meaningful disease control and quality of life preservation.
Key factors influencing growth rates include tumor genetics, patient immune function, treatment history, and tumor location within the brain. Modern imaging techniques allow precise monitoring of growth patterns, enabling personalized treatment adjustments based on individual tumor behavior.
Treatment options continue expanding through ongoing research and clinical trials. The combination of surgery, radiation therapy, and systemic treatments provides multiple approaches to controlling tumor growth and managing symptoms. For many patients, these interventions can slow or stop tumor progression, providing months to years of meaningful survival.
Quality of life considerations remain paramount throughout the treatment journey. Comprehensive supportive care, family education, and access to specialized resources help patients and caregivers navigate the challenges while maintaining dignity and comfort.
The landscape of melanoma brain metastases treatment continues evolving rapidly. Patients facing this diagnosis should seek care at specialized centers with multidisciplinary expertise and access to the latest treatment options. Early intervention, aggressive treatment when appropriate, and comprehensive supportive care offer the best opportunities for optimal outcomes.
For those seeking specialized care and expert consultation, The Minor Surgery Center provides comprehensive evaluation and treatment coordination for complex medical conditions. Don't wait—early intervention can make a significant difference in outcomes for melanoma brain metastases.