Ever wondered why some people tan effortlessly while others burn after just minutes in the sun? The answer lies in your Fitzpatrick skin type—a classification system that's been helping doctors and patients understand skin behavior for nearly 50 years.
Understanding your skin type isn't just about vanity or beach planning. It's a critical piece of your health puzzle that determines your skin cancer risk, guides your sun protection strategy, and helps your healthcare team deliver expert outpatient care tailored specifically to you.
At The Minor Surgery Center, we see patients every day who've never considered how their skin type affects their long-term health. Whether you're scheduling a routine skin check or seeking treatment for a concerning mole or lesion, knowing your Fitzpatrick classification empowers you to make informed decisions about your skin health.
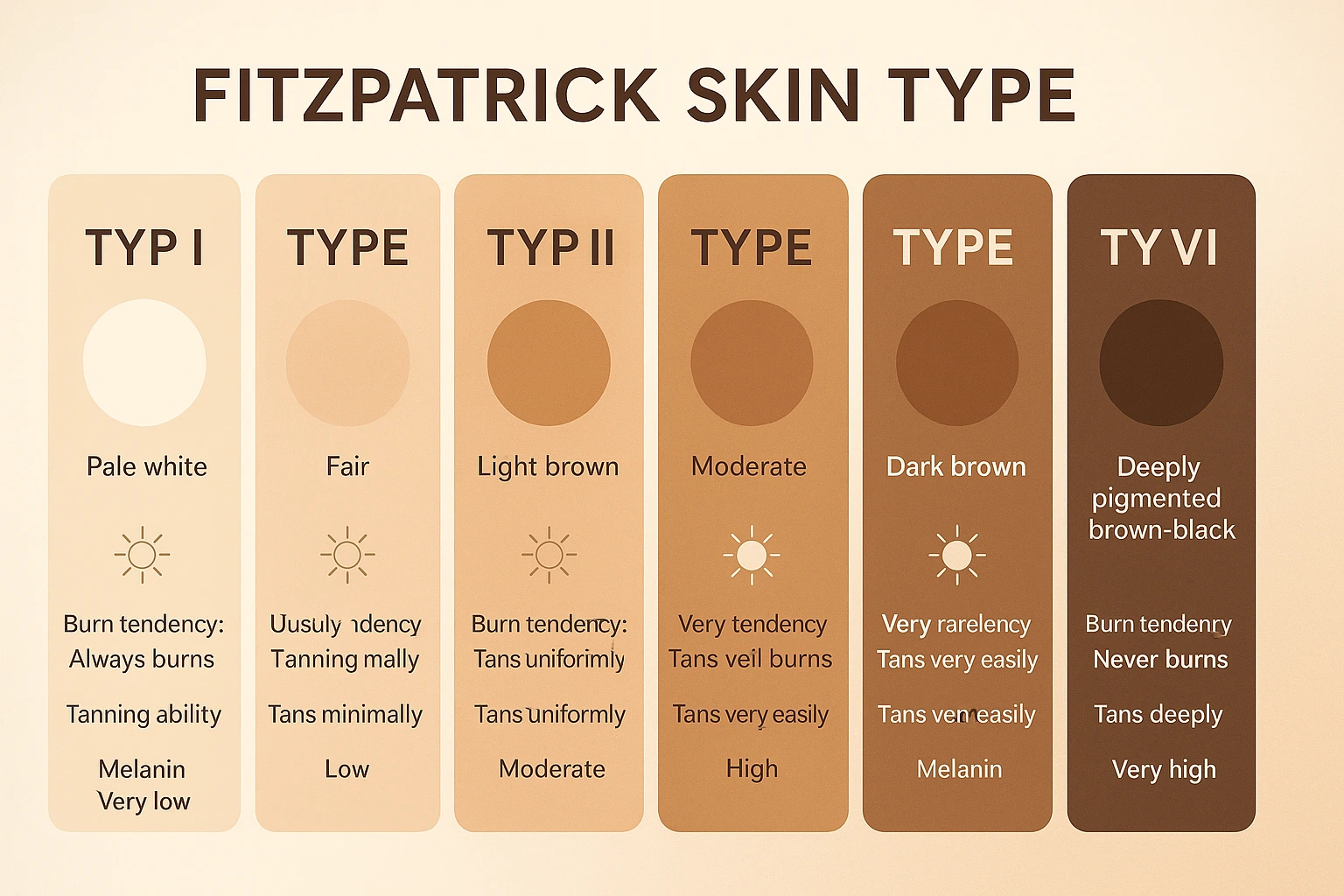
The Fitzpatrick scale is a numerical classification system that categorizes human skin into six distinct types based on two key factors: how much melanin (natural pigment) your skin produces and how your skin reacts to ultraviolet (UV) radiation from the sun[1][2].
Dr. Thomas B. Fitzpatrick developed this system in 1975 at Harvard Medical School. Originally, he created it to predict how patients with different skin tones would respond to ultraviolet A (UVA) phototherapy treatments for conditions like psoriasis and atopic dermatitis[2].
Think of it like a personalized owner's manual for your skin. Just as you wouldn't use the same maintenance schedule for a sports car and a pickup truck, you shouldn't use the same sun protection approach for all skin types.
Your Fitzpatrick skin type is determined by asking specific questions about your skin's behavior:
These questions aren't random. They reveal your skin's melanin production capacity—the biological factor that determines both your appearance and your vulnerability to UV damage[2].
Melanin acts as your skin's natural sunscreen. It absorbs and scatters UV radiation before it can damage the DNA in your skin cells. People with more melanin have built-in protection; those with less melanin need to be more vigilant about external protection measures.
The Fitzpatrick scale isn't just academic—it has real-world clinical applications that affect your care:
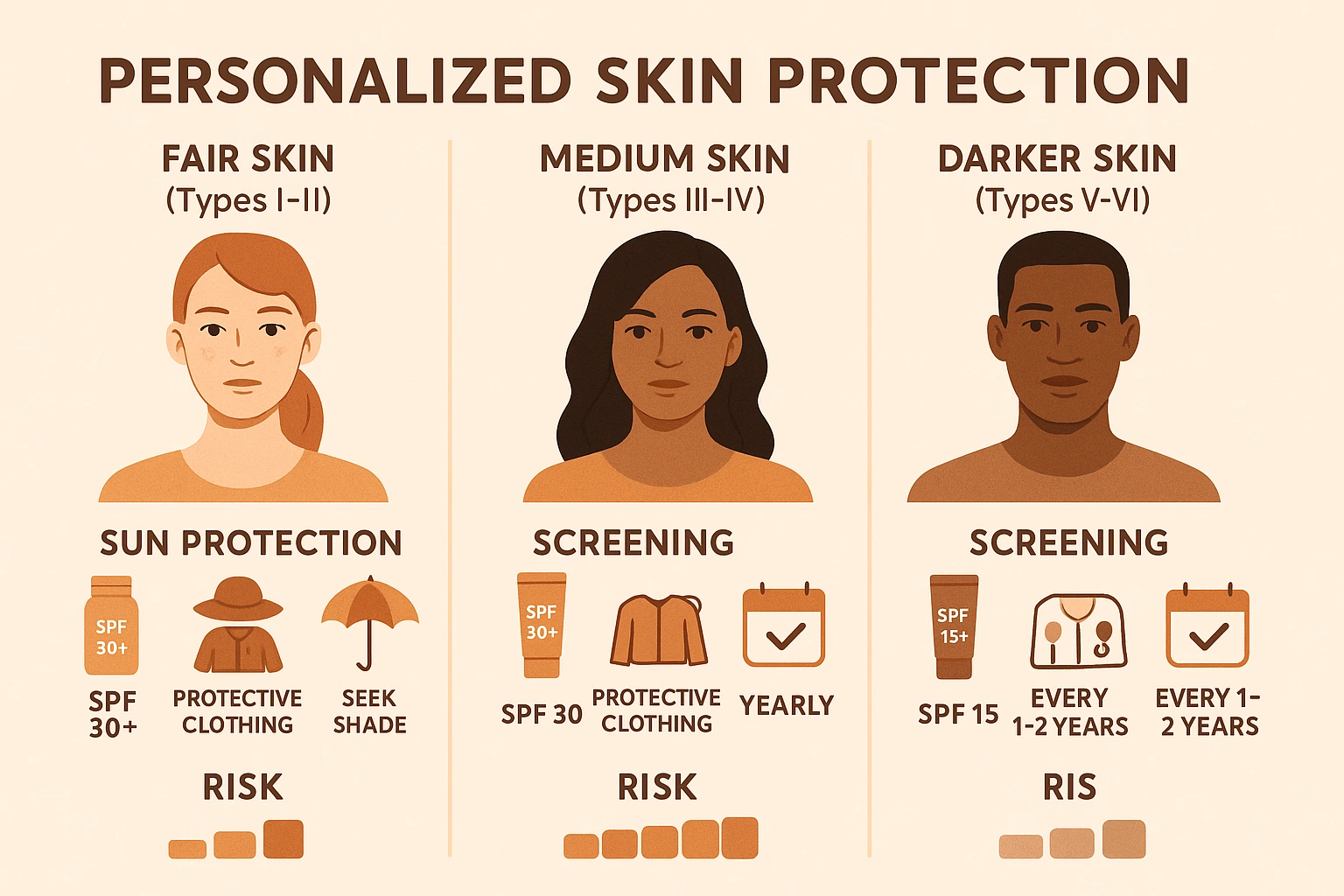
Sun protection counseling: Your dermatologist uses your skin type to recommend specific SPF levels, reapplication schedules, and protective clothing strategies.
Skin cancer risk assessment: Lower Fitzpatrick types (I-II) face significantly higher lifetime risk of melanoma and other skin cancers[1][6].
Treatment planning: When you need procedures like laser therapy, chemical peels, or phototherapy, your skin type determines safe and effective dosing.
Screening frequency: Patients with fair skin types typically need more frequent professional skin examinations to catch concerning changes early.
At The Minor Surgery Center, we incorporate your Fitzpatrick classification into every personalised treatment plan. This ensures we deliver safe and efficient surgery tailored to your unique biology.
Let's break down each skin type in detail. Remember—these are general guidelines, and individual variation exists within each category.
Characteristics:
Sun Reaction:
Cancer Risk: Highest risk category for all types of skin cancer, including melanoma, basal cell carcinoma, and squamous cell carcinoma[1][6].
Protection Strategy:
If you have Type I skin, think of sun protection as non-negotiable—like wearing a seatbelt. Your skin simply doesn't have the biological tools to defend itself against UV damage.
Characteristics:
Sun Reaction:
Cancer Risk: Very high risk for skin cancer, second only to Type I[1][6].
Protection Strategy:
Type II skin offers slightly more melanin protection than Type I, but not enough to rely on. Consistent sun protection remains critical for long-term skin health.
Characteristics:
Sun Reaction:
Cancer Risk: Moderate risk for skin cancer—lower than Types I and II but still significant[6].
Protection Strategy:
Type III represents a middle ground. While you have more natural protection than fairer skin types, you're not immune to UV damage or skin cancer.
Characteristics:
Sun Reaction:
Cancer Risk: Lower risk than Types I-III, but skin cancer still occurs and is often diagnosed at later stages[6].
Protection Strategy:
Even with Type IV skin, complacency is risky. Your natural melanin provides protection, but it's not a force field against all UV damage.
Characteristics:
Sun Reaction:
Cancer Risk: Low risk overall, but when skin cancer develops, it's often detected late because of lower awareness and screening rates[6].
Protection Strategy:
At The Minor Surgery Center, we've treated patients with Type V skin who assumed they were immune to skin problems. While your risk is lower, vigilance still matters—and early detection saves lives.
Characteristics:
Sun Reaction:
Cancer Risk: Lowest risk category, but skin cancer still occurs and is frequently diagnosed at advanced stages when treatment is more complex[6].
Protection Strategy:
Important note: Research shows that people with darker skin types often face delayed diagnosis of skin cancer because both patients and healthcare providers may not recognize warning signs as quickly[6]. This makes education and awareness even more critical.
Let's be direct: your Fitzpatrick skin type is one of the most significant predictors of your lifetime skin cancer risk.
Melanin isn't just responsible for your skin color—it's your body's first line of defense against UV radiation damage. Here's how it works:
When UV rays penetrate your skin, they can damage the DNA in your skin cells. This DNA damage, when it accumulates over time, can trigger the mutations that lead to skin cancer.
Melanin absorbs and scatters UV radiation before it reaches the deeper layers of your skin where cell division occurs[6]. Think of melanin like a natural umbrella—the bigger your umbrella (more melanin), the better protected you are from the storm (UV radiation).
People with Type I and II skin have small umbrellas. People with Type V and VI skin have large, sturdy umbrellas. But even the best umbrella isn't perfect—which is why everyone needs additional protection.
The numbers tell a clear story:
Types I and II (very fair to fair skin):
Types III and IV (medium to olive skin):
Types V and VI (dark brown to black skin):
Skin cancer isn't the only reason to protect your skin from UV damage:
Premature aging: UV exposure breaks down collagen and elastin, leading to wrinkles, sagging, and leathery texture—regardless of your skin type.
Hyperpigmentation: Darker skin types (III-VI) are particularly prone to uneven pigmentation, dark spots, and melasma from UV exposure.
Eye damage: UV radiation affects your eyes too, increasing risk of cataracts and macular degeneration.
Immune suppression: Excessive UV exposure can suppress your skin's immune function, making you more vulnerable to infections and slower to heal.
When patients come to The Minor Surgery Center for mole removal or skin cancer screening, we always discuss their Fitzpatrick type and personalized prevention strategies. Prevention is always easier than treatment.
Curious about your classification? Here's how to determine your Fitzpatrick skin type with reasonable accuracy.
Answer these questions honestly, thinking about your skin's natural behavior without tanning products or extensive sun protection:
Question 1: What is your natural skin color (on areas rarely exposed to sun, like your inner arm)?
Question 2: What color are your eyes?
Question 3: What is your natural hair color?
Question 4: Do you have freckles on unexposed areas?
Question 5: How does your skin react after 45-60 minutes of first summer sun exposure without protection?
While self-assessment provides a good starting point, a professional evaluation offers more precision—especially if you're planning medical treatments that depend on accurate skin typing.
During a consultation at The Minor Surgery Center, our experienced surgical team can:
This becomes particularly important if you're considering procedures like laser treatments, chemical peels, or phototherapy where incorrect skin typing could lead to complications or suboptimal results.
Some factors can make self-assessment tricky:
Mixed ancestry: If you have parents with very different skin types, you might fall between categories or have characteristics of multiple types.
Tanned skin: Assess your skin type based on your natural, untanned color—not your current appearance after summer sun exposure.
Age-related changes: Your skin's behavior may change as you age, though your underlying Fitzpatrick type remains constant.
Medical conditions: Certain conditions and medications can affect your skin's sun sensitivity independent of your Fitzpatrick type.
When in doubt, seek professional guidance. Understanding your skin type accurately is the foundation for effective, safe skin care and medical treatment.
Now that you understand your Fitzpatrick classification, let's translate that knowledge into action. Here's your personalized sun protection roadmap based on your skin type.
Before we dive into type-specific strategies, remember these rules apply to everyone, regardless of skin type:
✅ Broad-spectrum protection is essential—choose sunscreens that block both UVA and UVB rays
✅ Reapplication matters more than SPF—even SPF 100 fails if you don't reapply every two hours during sun exposure
✅ Protective clothing is your best defense—tightly woven fabrics, wide-brimmed hats, and UV-blocking sunglasses provide reliable protection
✅ Shade is your friend—seek shade during peak UV hours (10 AM to 4 PM)
✅ No such thing as a "safe tan"—any tan indicates DNA damage in your skin cells
✅ Cloudy days still require protection—up to 80% of UV rays penetrate clouds
✅ Water and snow amplify exposure—reflective surfaces increase your UV dose significantly
Your comfort-first approach to sun protection should be comprehensive and non-negotiable:
Daily sunscreen: Apply broad-spectrum SPF 50+ every morning, even when staying indoors (UVA penetrates windows). Use at least one ounce (shot glass full) for full body coverage.
Reapplication schedule: Every 90-120 minutes during any outdoor activity, immediately after swimming or heavy sweating.
Protective clothing:
Behavioral strategies:
Screening schedule: Annual full-body skin examination with a dermatologist or qualified healthcare provider. Monthly self-examinations to monitor for new or changing spots.
When to seek care: Schedule an appointment at The Minor Surgery Center if you notice:
Your skin has more natural protection, but don't let that create complacency:
Daily sunscreen: Broad-spectrum SPF 30 minimum for daily use, SPF 50 for extended outdoor exposure. Apply generously to all exposed areas.
Reapplication schedule: Every two hours during prolonged outdoor activities, after swimming or sweating.
Protective clothing:
Behavioral strategies:
Screening schedule: Professional skin examination every 1-2 years, or annually if you have personal or family history of skin cancer. Self-examinations every 2-3 months.
When to seek care: Don't ignore unusual spots because you assume your skin type makes you "safe." Visit our skin cancer clinic for evaluation of any concerning changes.
Your melanin provides significant natural protection, but you're not immune to UV damage or skin cancer:
Daily sunscreen: SPF 15-30 for daily use. Higher SPF during beach days, tropical vacations, or high-altitude activities. Sunscreen also prevents hyperpigmentation and uneven skin tone.
Reapplication schedule: Every 2-3 hours during extended sun exposure.
Protective clothing:
Behavioral strategies:
Screening schedule: Professional skin examination every 3-5 years, or more frequently if you have risk factors. Self-examinations focusing on palms, soles, nail beds, and mucous membranes where acral melanoma is more likely to occur.
When to seek care: Pay special attention to:
Our team provides expert outpatient care for patients of all skin types, with cultural competence and understanding that skin cancer awareness is critical across all communities.
Vitamin D considerations: Some people worry that sun protection will cause vitamin D deficiency. The truth: you can maintain healthy vitamin D levels through diet (fatty fish, fortified foods) and supplements while still protecting your skin. Brief, incidental sun exposure (walking to your car, etc.) provides adequate vitamin D for most people.
Sunscreen selection: Choose formulas appropriate for your skin:
After-sun care: If you do get sun exposure:
Your Fitzpatrick classification isn't just about sun protection—it directly influences how medical professionals approach various dermatological and cosmetic procedures.
Remember, the Fitzpatrick scale was originally developed to guide UV phototherapy for conditions like psoriasis and eczema[2]. Here's why that matters:
Type I-II patients require:
Type V-VI patients require:
Incorrect dosing based on skin type can lead to treatment failure (dose too low) or burns and increased cancer risk (dose too high).
Laser treatments for hair removal, pigmentation, vascular lesions, and skin resurfacing must be carefully calibrated to your Fitzpatrick type:
Fair skin (Types I-III):
Darker skin (Types IV-VI):
At The Minor Surgery Center, we carefully assess your skin type before recommending any laser-based treatment to ensure both safety and optimal results.
Chemical peels work by controlled damage to skin layers, stimulating regeneration. Your Fitzpatrick type determines:
Types I-II:
Types III-IV:
Types V-VI:
Your Fitzpatrick type influences screening protocols:
Screening frequency:
Examination focus:
Biopsy technique: When we perform skin biopsies at The Minor Surgery Center, we consider skin type when selecting biopsy method and discussing scarring risk. Darker skin types have higher risk of keloid formation, which influences our approach and post-procedure care recommendations.
Your Fitzpatrick type affects healing and scarring:
Types I-III:
Types IV-VI:
When you undergo minimally invasive solutions like mole removal or cyst excision with us, we discuss your skin type and implement strategies to minimize scarring and optimize cosmetic outcomes.
Let's clear up some persistent myths that can lead to poor decisions about skin health:
Reality: While Types V and VI have significantly more natural protection than fair skin, they're not immune to UV damage. Darker skin can still develop:
Everyone benefits from sun protection, regardless of skin type[6].
Reality: A tan is your skin's damage response to UV radiation. The ability to tan (Types III-VI) doesn't mean UV exposure is safe—it just means your skin produces melanin in response to DNA damage. That damage accumulates over time, increasing cancer risk and accelerating aging.
Reality: While Type I skin requires the most protection, complete sun avoidance isn't necessary or healthy. With proper protection (sunscreen, clothing, shade), people with very fair skin can safely enjoy outdoor activities. The key is being smart and consistent about protection.
Reality: Skin type is one factor among many that influence cancer risk. Other important factors include:
Two people with the same Fitzpatrick type can have very different actual risk levels based on these other factors.
Reality: Your Fitzpatrick type is determined by your genetics and doesn't change (though tanning can temporarily alter your skin color). You're born with a certain melanin production capacity, and while sun exposure can increase melanin temporarily, it doesn't change your underlying skin type or reduce your cancer risk.
Reality: SPF measures protection level, not protection duration. SPF 30 blocks about 97% of UVB rays, while SPF 50 blocks about 98%. The difference is minimal. What matters more is:
Reality: While most skin cancers develop on chronically sun-exposed skin, melanoma can develop anywhere on the body—including areas that rarely see sun. This is especially true for acral melanoma in darker skin types, which commonly appears on palms, soles, and under nails.
Regular full-body skin examinations are important for everyone.
Knowing when to schedule a professional skin check can literally save your life. Here's your guide to timing and warning signs.
Based on your Fitzpatrick type and risk factors:
High-risk (Types I-II, or any type with personal/family history):
Moderate-risk (Types III-IV with no significant history):
Lower-risk (Types V-VI with no significant history):
Remember: These are general guidelines. Your healthcare provider may recommend different timing based on your individual situation.
Schedule an immediate evaluation if you notice a spot with any of these characteristics:
A - Asymmetry: One half doesn't match the other half
B - Border irregularity: Edges are ragged, notched, or blurred
C - Color variation: Multiple colors or uneven color distribution (brown, black, tan, red, white, blue)
D - Diameter: Larger than 6mm (pencil eraser), though melanomas can be smaller
E - Evolving: Any change in size, shape, color, elevation, or new symptoms (bleeding, itching, crusting)
Beyond the ABCDE rule, seek evaluation for:
When you visit The Minor Surgery Center for a skin check:
Initial consultation: We'll discuss your medical history, sun exposure history, family history, and any specific concerns.
Full-body examination: Our experienced surgical team will examine your skin from head to toe, including areas you might not think to check yourself (scalp, between toes, etc.).
Dermoscopy: We use specialized magnification tools to examine suspicious spots in detail.
Documentation: We may photograph concerning areas for future comparison.
Biopsy if needed: If we identify a suspicious lesion, we can perform a biopsy right away. Our comfort-first approach ensures the procedure is as quick and painless as possible.
Clear communication: We explain our findings in plain language and discuss next steps if treatment is needed.
Personalized plan: Based on your Fitzpatrick type and findings, we'll recommend an appropriate follow-up schedule and prevention strategies.
One of the biggest mistakes people make is waiting until they're "sure" something is wrong. Early skin cancer often doesn't hurt, itch, or cause obvious symptoms.
If something concerns you—even if you can't articulate exactly why—get it checked. We'd rather reassure you that a spot is benign than have you delay evaluation of something serious.
Our goal is to help you get back to your life with confidence in your skin health. Early detection and treatment of skin cancer have excellent outcomes, while delayed diagnosis complicates treatment and worsens prognosis.
Understanding your Fitzpatrick skin type isn't about living in fear—it's about living informed and empowered.
The best sun protection strategy is one you'll actually follow consistently. Here's how to make it sustainable:
Make it routine: Apply sunscreen as automatically as brushing your teeth. Keep bottles in multiple locations (bathroom, car, desk, bag).
Choose products you like: If you hate how your sunscreen feels, you won't use it. Experiment with different formulations until you find ones that work for your skin type and preferences.
Prep your environment: Stock your home, car, and workplace with sun protection supplies (sunscreen, hats, sunglasses).
Plan ahead: Check UV index forecasts and plan outdoor activities accordingly. Many weather apps include UV index information.
Involve your family: Make sun protection a family value, not just a personal concern. Children who learn good habits early carry them into adulthood.
Monthly self-examinations help you catch changes early:
Timing: Pick a consistent day each month (first of the month, after your birthday, etc.).
Lighting: Use bright, natural light when possible.
Tools: Full-length mirror, hand mirror, and a partner to check hard-to-see areas.
Method: Examine every part of your body systematically:
Documentation: Consider taking photos of any spots you're monitoring, with a ruler for scale. This helps track subtle changes over time.
Know your baseline: Everyone has unique patterns of moles and spots. The goal is to notice what's new or changing for you.
Effective communication with your healthcare providers improves your care:
Be specific: Instead of "I'm worried about this spot," try "This mole on my left shoulder has gotten darker over the past three months."
Ask questions:
Share your full history: Mention childhood sunburns, tanning bed use, family history, and any previous skin treatments or cancers.
Request explanations: If medical jargon confuses you, ask for plain-language explanations. At The Minor Surgery Center, clear communication is a core value.
If you have fair-skinned children (Types I-II), establishing good habits early is critical:
Model behavior: Children learn by watching. If they see you applying sunscreen and seeking shade, they'll internalize these behaviors.
Make it fun: Use colorful sunscreen, fun hats, and UV-detecting beads or bracelets that change color in the sun.
Explain age-appropriately: Even young children can understand "the sun can hurt our skin, so we protect it."
Establish non-negotiables: Sunscreen before outdoor play isn't optional—it's as automatic as wearing a seatbelt.
Regular skin checks: Teach children to tell you about new or changing spots, and conduct gentle skin checks as part of routine care.
School advocacy: Ensure schools have sun-safe policies, including shaded play areas and permission for sunscreen application.
Some people with very fair skin feel self-conscious about their appearance. Remember:
Your skin type is part of your identity—not a flaw to fix.
Healthy skin is beautiful skin—regardless of color or tone.
Makeup and self-tanners can enhance your appearance if desired, but they don't provide sun protection (unless specifically formulated with SPF).
Avoid tanning beds and excessive sun exposure to darken your skin. The damage isn't worth it, and the "healthy glow" of a tan is actually a sign of DNA damage.
If you have concerns about pigmentation, scarring, or skin texture, consult with our team about safe and efficient surgery or cosmetic options appropriate for your skin type.
The Fitzpatrick scale has served dermatology well for nearly 50 years, but the field continues to evolve.
Researchers have identified some limitations of the Fitzpatrick classification:
Oversimplification: Six categories can't capture the full diversity of human skin tones and behaviors.
Self-reporting bias: The scale relies on patients accurately remembering and reporting their sun reactions, which can be unreliable.
Limited applicability: The scale was developed based on white and light-skinned populations and may not accurately classify all ethnicities.
Binary thinking: The scale emphasizes sun sensitivity but doesn't capture other important skin characteristics like tendency toward hyperpigmentation, scarring, or specific disease risks.
New approaches are being developed:
Objective measurements: Devices that measure melanin content and skin reflectance provide more objective data than self-reporting.
Expanded categories: Some researchers propose more granular classification systems with additional categories or continuous scales rather than discrete types.
Multi-dimensional assessment: New frameworks consider not just sun sensitivity but also factors like:
Genetic testing: As genetic research advances, we may eventually classify skin based on specific genetic markers that predict behavior and disease risk.
The future of skin care is increasingly personalized:
AI-assisted diagnosis: Artificial intelligence tools are being developed to analyze skin images and detect cancer with accuracy rivaling or exceeding human dermatologists.
Customized products: Skincare and sunscreen formulations tailored to your specific skin type, environment, and lifestyle.
Precision medicine: Treatment protocols based on your unique genetic profile, skin characteristics, and disease risk factors.
Telemedicine integration: Remote skin monitoring and consultation, making regular screening more accessible.
At The Minor Surgery Center, we stay current with advances in dermatological care while maintaining our commitment to personalised treatment plans and warm, human care.
Understanding your Fitzpatrick skin type is more than academic knowledge—it's a practical tool for protecting your health and living confidently.
Whether you have the fairest Type I skin that burns at the slightest sun exposure, or deeply pigmented Type VI skin with natural UV protection, you now have the information you need to:
✅ Assess your personal skin cancer risk based on melanin content and sun sensitivity
✅ Implement appropriate sun protection strategies tailored to your specific needs
✅ Schedule regular professional skin examinations at the right frequency for your risk level
✅ Recognize warning signs that warrant immediate professional evaluation
✅ Make informed decisions about cosmetic and medical procedures that depend on skin type
✅ Teach your family about sun safety and skin health
Remember: your Fitzpatrick type is just one piece of your health puzzle. Personal history, family history, lifestyle, and environmental factors all contribute to your overall risk and care needs.
Today:
This week:
This month:
This year:
At The Minor Surgery Center, we understand that skin concerns can feel overwhelming. Whether you need a routine screening, evaluation of a suspicious spot, or removal of a mole or lesion, our team provides expert outpatient care with a comfort-first approach.
We see patients of all Fitzpatrick skin types, and we tailor our approach to your unique needs. Our goal is simple: help you get back to your life with confidence in your skin health.
Don't wait until a small concern becomes a big problem. Early detection and treatment of skin cancer have excellent outcomes, and peace of mind is priceless.
Your skin is the only one you'll ever have—treat it with the care and attention it deserves.
[1] Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124(6):869-871.
[2] Fitzpatrick TB. Soleil et peau [Sun and skin]. J Med Esthet. 1975;2:33-34.
[3] D'Orazio J, Jarrett S, Amaro-Ortiz A, Scott T. UV radiation and the skin. Int J Mol Sci. 2013;14(6):12222-12248.
[4] Roberts WE. Skin type classification systems old and new. Dermatol Clin. 2009;27(4):529-533.
[5] Eilers S, Bach DQ, Gaber R, et al. Accuracy of self-report in assessing Fitzpatrick skin phototypes I through VI. JAMA Dermatol. 2013;149(11):1289-1294.
[6] Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: A review and recommendations for physicians and the public. J Am Acad Dermatol. 2014;70(4):748-762.
[7] Sachdeva S. Fitzpatrick skin typing: Applications in dermatology. Indian J Dermatol Venereol Leprol. 2009;75(1):93-96.
[8] Brenner M, Hearing VJ. The protective role of melanin against UV damage in human skin. Photochem Photobiol. 2008;84(3):539-549.