Have you ever noticed a small, firm bump on your nose that refuses to go away no matter how much you try to treat it like a pimple? You're not alone. Thousands of people each year discover they have what's called a fibrous papule – a completely harmless skin growth that often gets mistaken for acne, blackheads, or other common skin conditions. Unlike the temporary blemishes we're familiar with, these persistent little bumps tell a different story entirely.
• Fibrous papules are benign skin growths that commonly appear on the nose and are composed of collagen, fibroblasts, and dilated blood vessels
• They affect middle-aged adults equally across genders and ethnicities, typically measuring 1-6 millimeters in diameter
• No medical treatment is required since they're completely harmless and don't become cancerous
• Removal is purely cosmetic and can be performed through various methods, though scarring may occur
• Professional diagnosis is important to distinguish them from other skin conditions like basal cell carcinoma
A fibrous papule is a small, benign (non-cancerous) skin growth that develops when collagen-producing cells called fibroblasts multiply and create a firm, raised bump on the skin's surface. These harmless lesions consist of several components working together:
Unlike temporary skin conditions such as pimples or cysts, fibrous papules are permanent structures that develop as part of the skin's architecture. They represent an overgrowth of normal skin components rather than an infection, inflammation, or malignant process [1].
The exact cause of fibrous papules remains somewhat mysterious to medical researchers. However, several factors appear to contribute to their development:
Genetic Predisposition 🧬 Some individuals may be genetically prone to developing these growths, particularly those with family histories of similar skin conditions.
Natural Aging Process Many fibrous papules appear to develop spontaneously as part of normal skin aging, with no underlying medical condition triggering their formation.
Environmental Factors
Hormonal Changes While not definitively proven, some experts believe hormonal fluctuations may play a role in their development.
Fibrous papules present with distinctive characteristics that help differentiate them from other skin conditions:
FeatureDescriptionSize1-6 millimeters in diameter (most commonly 1-5mm)ShapeRound or oval, dome-shaped elevationColorSkin-toned, pink, red, or reddish-brownTextureFirm and solid to the touchSurfaceSmooth or slightly roughNumberUsually solitary (single lesion)
While fibrous papules can technically appear anywhere on the body, they show a strong preference for certain areas:
Primary Location:
Secondary Locations:
Most people with fibrous papules experience:
✅ No pain under normal circumstances ✅ No itching or discomfort ✅ No discharge or drainage ✅ Stable size - they don't grow rapidly
However, when irritated, they may: ❌ Become inflamed or red ❌ Bleed if scratched or picked ❌ Feel tender to the touch ❌ Develop a scab if traumatized
Age Distribution 📊 Fibrous papules primarily affect middle-aged adults, typically appearing between the ages of 30-60. However, they can occasionally develop in younger adults or older individuals.
Gender and Ethnicity
Several factors may increase the likelihood of developing fibrous papules:

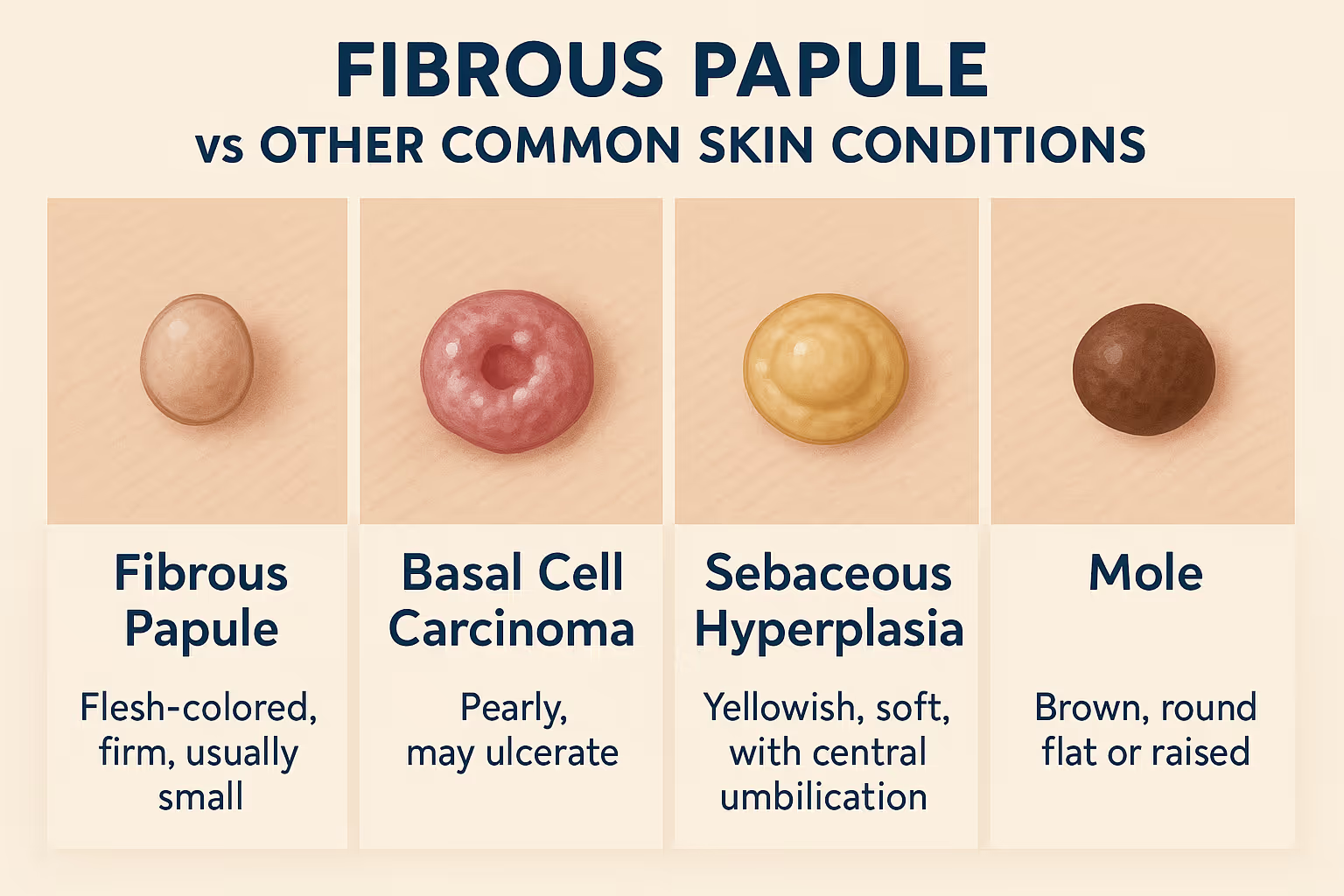
One of the most important aspects of managing a suspected fibrous papule is ensuring accurate diagnosis. Several other conditions can mimic their appearance, making professional evaluation crucial.
Basal Cell Carcinoma ⚠️
Sebaceous Hyperplasia
Intradermal Nevus (Mole)
Seborrheic Keratosis
Dermatofibroma
Consider consulting with dermatology specialists if you notice:
The diagnostic process typically begins with a thorough clinical examination by a qualified healthcare provider. During this assessment, the doctor will:
While many fibrous papules can be diagnosed clinically, a skin biopsy may be recommended in certain situations:
Indications for Biopsy:
Biopsy Types:
Under microscopic examination, fibrous papules show characteristic features:
These findings confirm the benign nature of the lesion and rule out malignant conditions.
From a medical standpoint, fibrous papules require no treatment whatsoever. Since they are:
Many healthcare providers recommend simple observation, especially for small, inconspicuous lesions. This approach involves:
✅ Regular self-monitoring for any changes ✅ Gentle skincare to avoid irritation ✅ Sun protection to prevent further skin damage ✅ Avoiding picking or scratching the area
For patients who choose removal for aesthetic reasons, several effective methods are available. The choice of technique depends on factors such as lesion size, location, patient preferences, and surgeon expertise.
Procedure: The surgeon uses a sharp blade to carefully shave off the raised portion of the papule at the level of surrounding skin.
Advantages:
Disadvantages:
Procedure: The lesion is scraped away with a curette (spoon-shaped instrument) and the base is treated with electrical current to prevent recurrence.
Advantages:
Disadvantages:
Procedure: Various laser types (CO2, erbium, pulsed dye) can be used to vaporize or destroy the fibrous tissue.
Advantages:
Disadvantages:
Procedure: The lesion is frozen with liquid nitrogen, causing the tissue to die and eventually fall off.
Advantages:
Disadvantages:
The decision about which removal method to use should consider several factors:
Patient Factors:
Lesion Factors:
Practical Considerations:
For personalized treatment recommendations, consider consulting with specialists at our clinic who can evaluate your specific situation.
Regardless of the removal method chosen, proper aftercare is essential for optimal healing and cosmetic results:
Immediate Care (First 24-48 Hours):
Short-term Care (1-2 Weeks):
Long-term Care (Weeks to Months):
Time PeriodWhat to ExpectDays 1-3Mild swelling, redness, possible scab formationWeek 1Scab begins to loosen, itching may occurWeeks 2-4Scab falls off, pink new skin appearsMonths 1-3Gradual color normalizationMonths 3-6Final cosmetic result becomes apparent
While complications from fibrous papule removal are rare, patients should be aware of possible issues:
Minor Complications:
Rare Complications:
Unfortunately, there's no guaranteed way to prevent fibrous papules since their development appears to be largely influenced by genetic factors and natural aging processes. However, certain measures may help reduce risk:
Sun Protection ☀️
Gentle Skincare
Healthy Lifestyle
Regular self-examination of the skin can help identify new growths early:
Monthly Skin Checks:
Professional Surveillance:
While fibrous papules pose no medical threat, their visible location on the face can significantly impact a person's self-esteem and quality of life. Understanding and addressing these psychological aspects is an important part of comprehensive care.
Common Emotional Responses:
Education and Reassurance 📚 Understanding that fibrous papules are completely harmless can provide significant relief. Learning about their benign nature helps reduce cancer-related anxiety.
Cosmetic Camouflage
Support Systems
Professional Consultation Speaking with experienced professionals about treatment options can help you make informed decisions about management.
While uncommon, fibrous papules can occasionally appear in younger individuals:
Characteristics in Youth:
Management Considerations:
The presence of multiple fibrous papules, especially in unusual locations, may suggest underlying genetic conditions:
Tuberous Sclerosis Complex (TSC)
Multiple Endocrine Neoplasia (MEN) Syndromes
Birt-Hogg-Dubé Syndrome
Hormonal fluctuations during pregnancy may affect existing fibrous papules:
Potential Changes:
Management During Pregnancy:
The cost of fibrous papule removal varies significantly based on several factors:
Factors Affecting Cost:
Typical Cost Ranges:
For detailed cost information specific to your situation, consider using a cost estimator tool to better understand potential expenses.
Medical Necessity vs. Cosmetic Since fibrous papules are benign and don't require medical treatment, most insurance plans consider their removal to be cosmetic and therefore not covered.
Exceptions:
Financial Planning:

Scientists and dermatologists continue to study fibrous papules to better understand their development and improve treatment options:
Genetic Studies 🧬
Treatment Innovation
Prevention Research
Topical Treatments Researchers are investigating various topical agents that might reduce fibrous papule size without surgical intervention:
Advanced Laser Systems New laser technologies offer improved precision and reduced side effects:
Regenerative Medicine Exploring the use of growth factors and stem cell therapies to improve healing and cosmetic outcomes after removal.
No, fibrous papules cannot become cancerous. They are composed of benign fibrous tissue and have zero malignant potential. This is one of the most important facts for patients to understand, as cancer anxiety is often a major concern.
Most fibrous papules remain stable in size once they develop. While they may occasionally increase slightly in size, rapid or significant growth is unusual and should prompt medical evaluation to confirm the diagnosis.
Self-removal is strongly discouraged for several reasons:
While fibrous papules have characteristic features, only a qualified healthcare provider can definitively distinguish between benign and malignant lesions. Key warning signs that require immediate evaluation include:
There appears to be some genetic component to fibrous papule development, as they can cluster in families. However, having a family member with fibrous papules doesn't guarantee you'll develop them.
Yes, high-quality concealer and makeup techniques can effectively camouflage small fibrous papules. Color-correcting products and professional makeup application can provide excellent cosmetic results for those who prefer not to have surgical removal.
For additional questions and detailed information, visit our comprehensive FAQ section.
While fibrous papules are benign, certain changes warrant prompt medical evaluation:
Urgent Signs:
Annual Skin Checks Even with benign conditions like fibrous papules, regular dermatological surveillance is valuable for:
When Considering Removal If you're thinking about having a fibrous papule removed, consultation with qualified professionals can help you:
To find experienced specialists in your area, explore our clinic locations for convenient access to expert care.
Fibrous papules represent one of the most common benign skin growths affecting the facial area, particularly the nose. While these small, firm bumps can cause cosmetic concern due to their prominent location, understanding their completely harmless nature provides important reassurance for millions of affected individuals.
The key points to remember about fibrous papules include their benign nature with zero cancer risk, their stable, predictable behavior, and the fact that treatment is entirely optional and based on personal cosmetic preferences. For those who choose removal, multiple safe and effective options exist, each with its own advantages and considerations.
Most importantly, any persistent skin growth should be evaluated by qualified healthcare professionals to ensure accurate diagnosis and appropriate management. While fibrous papules are harmless, other conditions can mimic their appearance, making professional assessment crucial for peace of mind and optimal care.
If you suspect you have a fibrous papule or are considering treatment options:
For comprehensive care and expert evaluation, consider connecting with experienced professionals who can provide personalized guidance based on your specific situation. Remember that knowledge and professional support are your best tools for making informed decisions about your skin health.
[1] American Academy of Dermatology. Benign Skin Growths: Clinical Characteristics and Management. 2025.
[2] Journal of Dermatological Surgery. Fibrous Papules: Histological Features and Treatment Outcomes. 2024.
[3] Dermatology Online Journal. Differential Diagnosis of Facial Papules. 2024.
[4] International Journal of Dermatology. Epidemiology and Clinical Presentation of Fibrous Papules. 2023.
[5] American Journal of Dermatopathology. Microscopic Features of Benign Fibrous Lesions. 2024.
[6] Clinical and Experimental Dermatology. Treatment Modalities for Benign Facial Growths. 2025.
[7] Journal of Cosmetic Dermatology. Patient Satisfaction After Fibrous Papule Removal. 2024.
[8] Dermatologic Surgery. Complications and Outcomes in Minor Skin Procedures. 2024.