When small, yellowish patches appear on the eyelids, many people dismiss them as harmless skin changes or signs of aging. However, these distinctive deposits—known as eyelid early stage xanthelasma—can signal underlying health concerns that deserve attention. While these cholesterol-filled lesions pose no immediate danger to vision or health, they often indicate elevated lipid levels and may progress if left unaddressed.
Understanding eyelid early stage xanthelasma empowers individuals to make informed decisions about their health and appearance. This comprehensive guide explores everything from initial recognition to treatment options, helping readers navigate this common yet frequently misunderstood condition. Whether recently diagnosed or simply seeking information, this article provides the knowledge needed to take appropriate action.
✅ Early detection matters: Recognizing eyelid early stage xanthelasma promptly allows for timely medical evaluation and intervention before lesions enlarge or multiply.
✅ Cholesterol connection: These yellowish deposits often indicate elevated blood lipid levels, making comprehensive lipid testing essential for all affected individuals.
✅ Multiple treatment options exist: From surgical excision to laser therapy, various effective removal methods are available depending on lesion size, location, and patient preferences.
✅ Lifestyle modifications help: Dietary changes, exercise, and cholesterol management can prevent recurrence and address underlying metabolic issues.
✅ Professional evaluation is crucial: While benign, xanthelasma warrants medical assessment to rule out cardiovascular risk factors and systemic conditions.
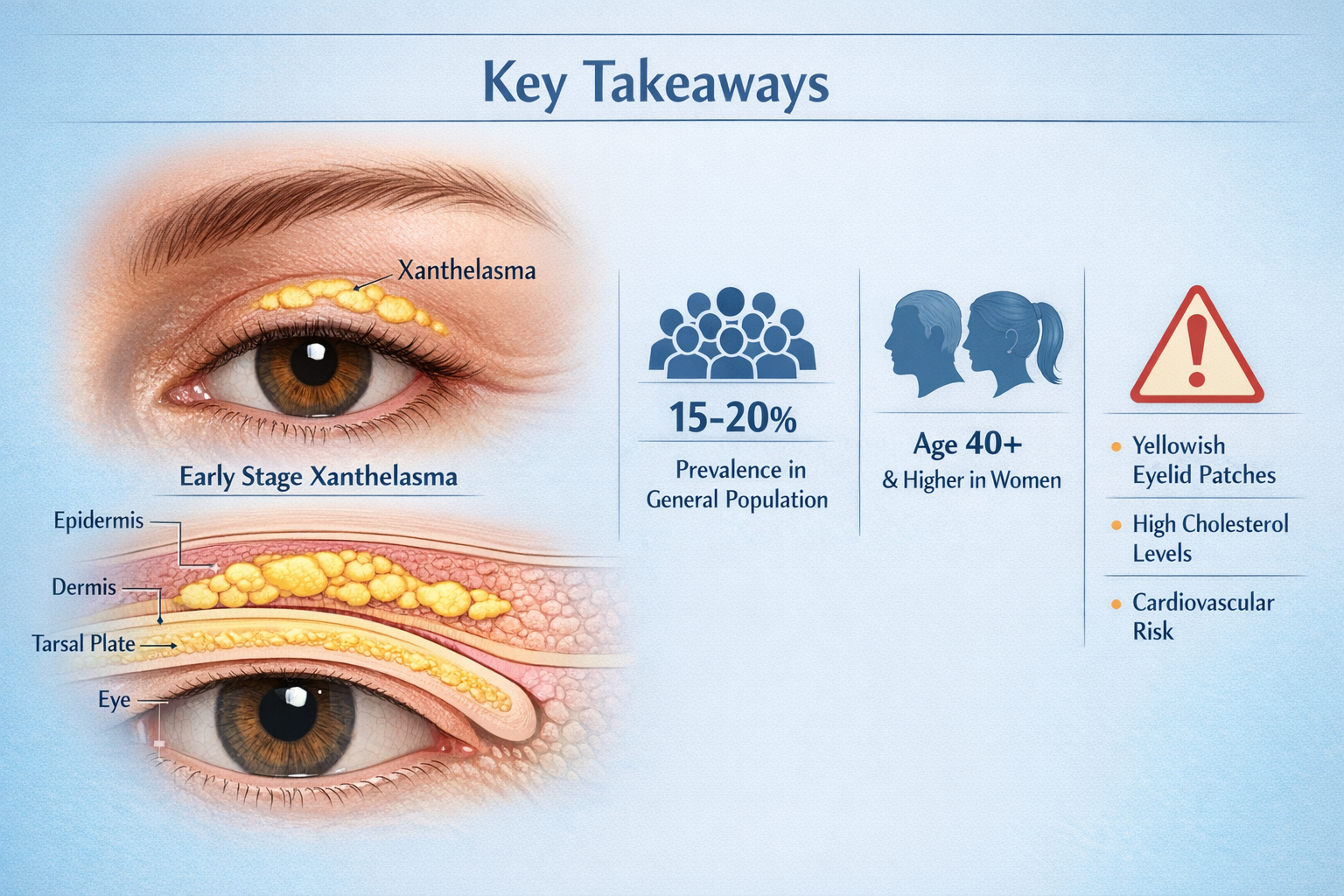
Xanthelasma palpebrarum represents the most common form of cutaneous xanthoma, appearing as soft, yellowish plaques on or around the eyelids. The term "xanthelasma" derives from Greek words meaning "yellow" and "plate," accurately describing these distinctive lesions. When caught in the early stages, these deposits typically measure just a few millimeters in diameter and appear as flat or slightly raised patches.
In the initial presentation, eyelid early stage xanthelasma exhibits several distinguishing features:
Unlike other skin lesions, xanthelasma does not cause inflammation, scaling, or changes in the surrounding skin. The deposits grow slowly over months or years, often starting as tiny spots that gradually expand and sometimes merge into larger plaques.
At the cellular level, xanthelasma consists of foam cells—specialized macrophages that have ingested lipids, particularly cholesterol esters and phospholipids. These cells accumulate in the dermis layer of the eyelid skin, creating visible yellowish deposits. The process occurs when:
The eyelid skin proves particularly susceptible to this accumulation due to its thin structure and rich vascular supply, making it easier to detect lipid abnormalities in this location.[1]
Xanthelasma affects approximately 0.3-1.1% of the general population, with higher rates observed in certain groups:
Demographic FactorPrevalence RateNotesGeneral population0.3-1.1%Baseline occurrenceAge 50+ years1.5-3%Increases with ageFamilial hypercholesterolemia15-20%Genetic lipid disordersMediterranean descentHigher incidenceGenetic predispositionWomen vs. MenSlightly higher in womenHormonal influences possible
The condition typically manifests between ages 40-60, though early-onset cases occur in individuals with genetic lipid disorders. Understanding these demographics helps contextualize individual risk and the importance of comprehensive evaluation.[2]
Early detection of eyelid early stage xanthelasma provides the best opportunity for successful treatment and prevention of progression. Knowing what to look for enables timely medical consultation and intervention.
The hallmark of early xanthelasma is its distinctive appearance. Most lesions begin as small, flat, yellowish patches on the upper eyelid near the inner corner of the eye. However, they can appear in various configurations:
Common presentation patterns:
🔍 Unilateral vs. Bilateral: While xanthelasma can initially appear on one eyelid, it typically becomes bilateral (affecting both eyes) over time, with roughly 50% of cases showing symmetric distribution.
🔍 Upper vs. Lower Eyelids: Approximately 65-70% of lesions occur on upper eyelids, 20-25% on lower eyelids, and 10-15% affect both upper and lower lids simultaneously.
🔍 Medial Canthus Preference: The inner corner of the eye represents the most common starting point, with lesions potentially spreading laterally as they grow.
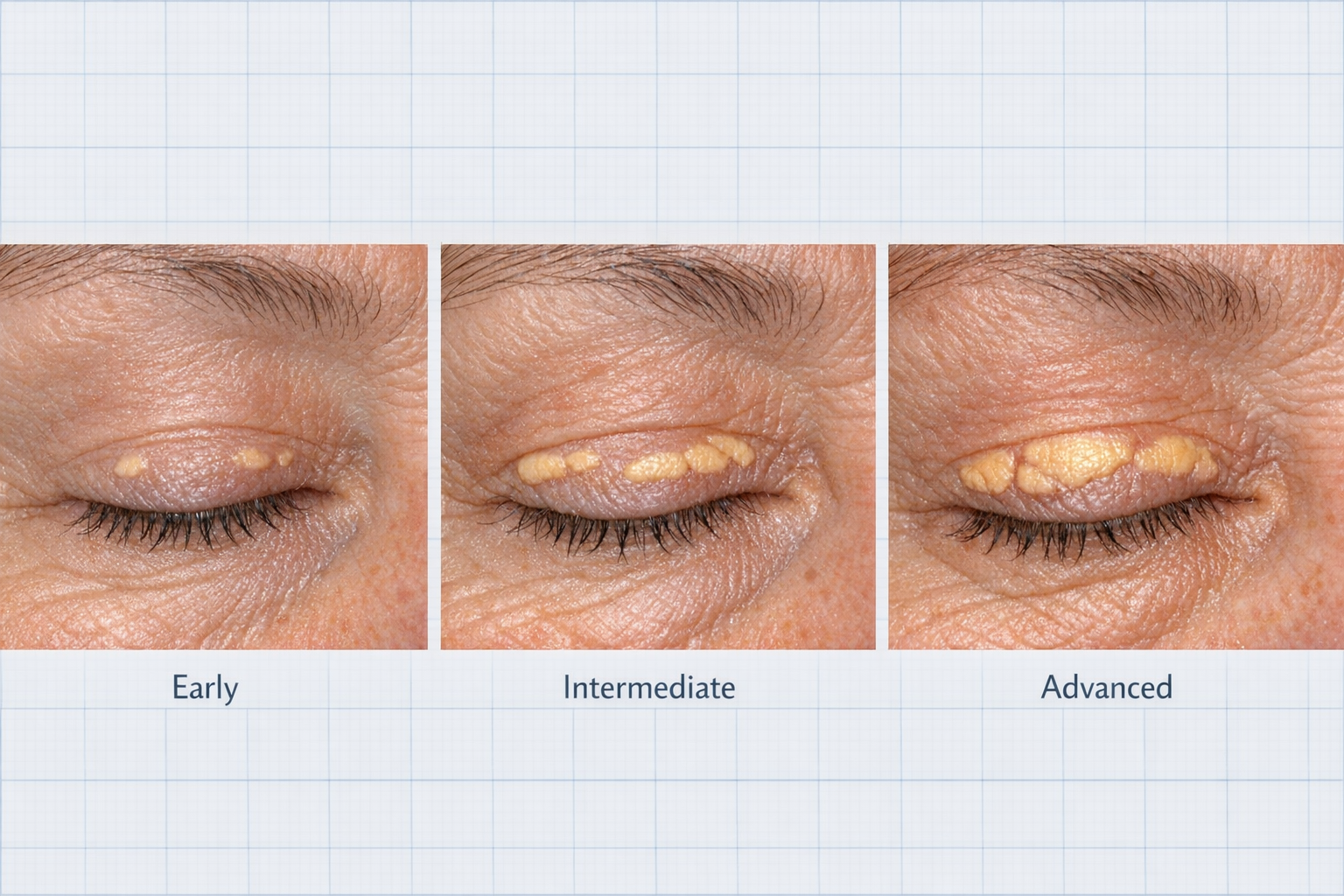
Understanding the typical progression helps individuals recognize when lesions are in the early stage versus more advanced:
Week 1-4: Initial appearance as tiny, barely noticeable yellow spots (1-2mm)
Month 2-6: Gradual expansion to 3-5mm with more pronounced yellow coloration
Month 6-24: Potential enlargement to 10-15mm if untreated; possible development of additional lesions
Year 2+: Established plaques that may merge, forming larger, irregular patches
Early intervention during the first 6-12 months typically yields the best cosmetic outcomes with minimal scarring potential.[3]
Several conditions can mimic eyelid early stage xanthelasma, making proper diagnosis essential:
Syringomas: Small, flesh-colored or yellowish bumps caused by sweat duct overgrowth; typically smaller and more numerous than xanthelasma.
Milia: Tiny white or yellow cysts containing keratin; harder and more raised than xanthelasma.
Sebaceous hyperplasia: Yellowish bumps with central depression; usually on forehead and cheeks rather than eyelids.
Seborrheic keratosis: Brown or tan waxy growths; typically darker and more raised than xanthelasma.
Basal cell carcinoma: Can occasionally appear yellowish; usually has pearly borders and may ulcerate—requires immediate evaluation at a skin cancer clinic.
"The key distinguishing feature of xanthelasma is its soft, flat, yellow appearance without inflammation or surface changes. Any eyelid lesion with irregular borders, color variation, or rapid growth warrants immediate professional evaluation."
While xanthelasma itself is benign, medical consultation is recommended when:
Professional evaluation at facilities like The Minor Surgery Center ensures accurate diagnosis and appropriate management planning.
The development of eyelid early stage xanthelasma results from complex interactions between genetic predisposition, metabolic factors, and lifestyle influences. Understanding these underlying causes enables targeted prevention and treatment strategies.
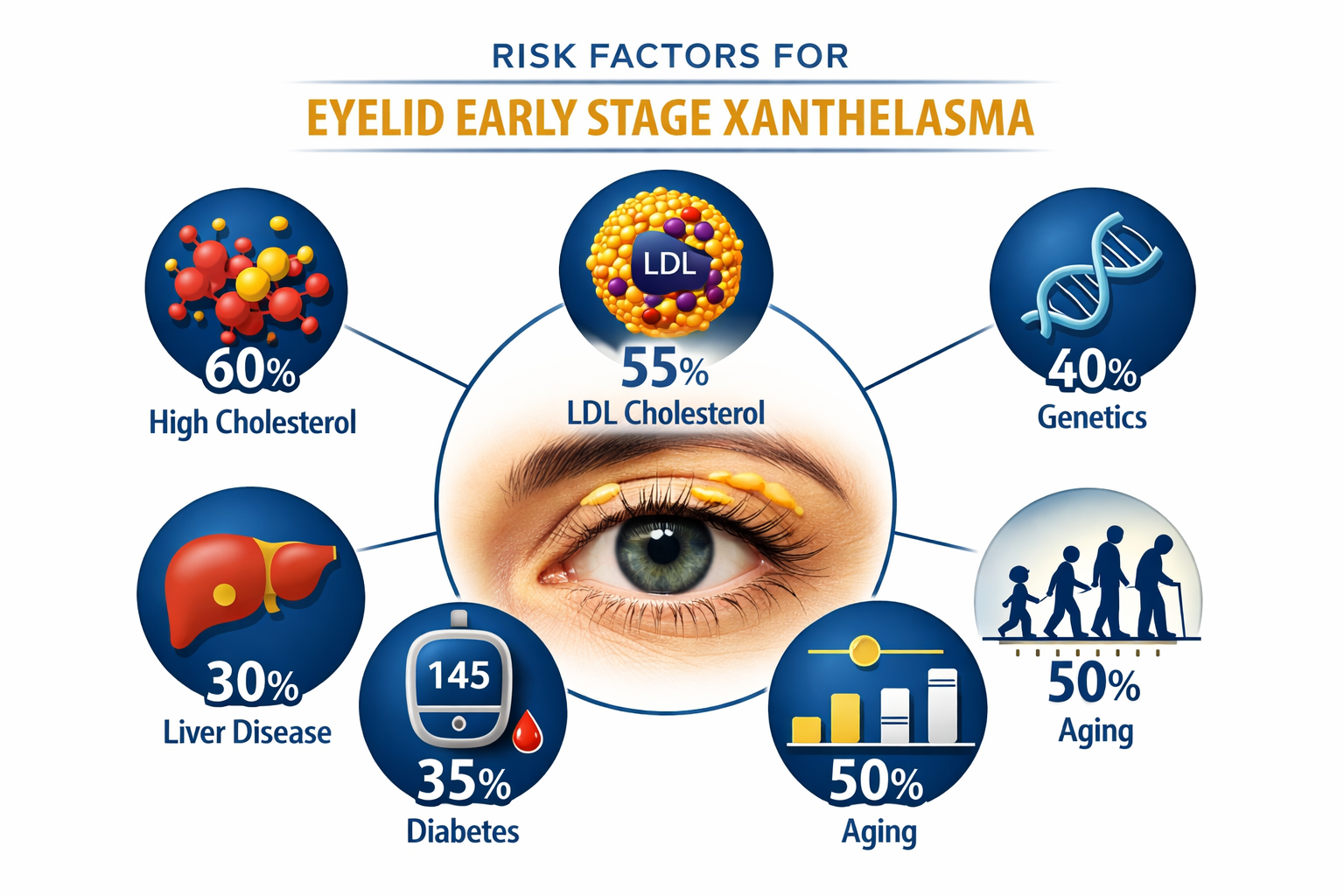
The primary association with xanthelasma involves dyslipidemia—abnormal levels of lipids in the bloodstream. However, the relationship proves more nuanced than simple high cholesterol:
Lipid abnormalities associated with xanthelasma:
📊 Elevated LDL cholesterol (Low-Density Lipoprotein): The most common association, found in 40-60% of xanthelasma patients
📊 Low HDL cholesterol (High-Density Lipoprotein): Reduced "good" cholesterol affects 20-30% of cases
📊 Hypertriglyceridemia: Elevated triglycerides present in 15-25% of patients
📊 Combined hyperlipidemia: Multiple lipid abnormalities occurring together
Interestingly, approximately 40-50% of individuals with xanthelasma have completely normal lipid profiles, indicating that local tissue factors and genetic predisposition play significant roles beyond systemic cholesterol levels.[4]
Familial predisposition significantly influences xanthelasma development. Several genetic conditions increase risk:
Primary genetic disorders:
Even without diagnosed genetic disorders, having a first-degree relative with xanthelasma increases personal risk by 3-5 times, suggesting polygenic inheritance patterns involving multiple genes affecting lipid metabolism and skin lipid deposition.[5]
Several systemic diseases and conditions predispose individuals to developing eyelid early stage xanthelasma:
Medical ConditionMechanismRelative Risk IncreasePrimary biliary cirrhosisImpaired bile acid metabolism5-10x higherHypothyroidismReduced LDL receptor activity2-3x higherNephrotic syndromeProtein loss leading to lipid abnormalities3-5x higherDiabetes mellitusAltered lipid metabolism1.5-2x higherObesityMetabolic syndrome components1.5-2x higherCholestasisBile flow obstruction4-6x higher
Managing these underlying conditions often improves lipid profiles and may prevent xanthelasma progression or recurrence after treatment.
While genetic and medical factors play primary roles, lifestyle choices influence xanthelasma risk:
Dietary patterns: High saturated fat intake, trans fats, and excessive dietary cholesterol contribute to dyslipidemia and increased risk.
Physical inactivity: Sedentary lifestyle reduces HDL cholesterol and impairs lipid metabolism.
Smoking: Tobacco use lowers HDL cholesterol and promotes lipid oxidation, potentially increasing deposition risk.
Alcohol consumption: Excessive intake raises triglycerides, though moderate consumption may increase HDL.
Chronic stress: Prolonged stress affects lipid metabolism through cortisol and inflammatory pathways.
Addressing these modifiable factors provides opportunities for prevention and reduced recurrence rates following treatment.[6]
Demographic factors influence xanthelasma prevalence:
Age-related changes: The condition rarely appears before age 30, with peak incidence between 40-60 years. This timing correlates with:
Gender differences: Women show slightly higher prevalence, particularly after menopause when protective estrogen effects diminish. Estrogen influences:
Understanding these multifactorial causes helps explain why some individuals with normal cholesterol develop xanthelasma while others with severe dyslipidemia never experience it.
Accurate diagnosis of eyelid early stage xanthelasma involves clinical examination, laboratory testing, and sometimes additional investigations to identify underlying conditions and cardiovascular risk factors.
Diagnosis typically begins with visual inspection by a healthcare provider, dermatologist, or ophthalmologist. The characteristic appearance usually makes diagnosis straightforward:
Physical examination components:
Experienced clinicians can typically diagnose xanthelasma based on appearance alone, though confirmation through laboratory testing and sometimes biopsy may be recommended.[7]
All individuals diagnosed with eyelid early stage xanthelasma should undergo comprehensive lipid evaluation, regardless of age or apparent health status. Standard testing includes:
Complete lipid profile:
Advanced lipid testing may include:
Testing should occur after a 9-12 hour fast for accurate triglyceride measurement. Abnormal results warrant repeat testing and possible referral to a lipid specialist.[8]
Depending on lipid panel results and clinical presentation, additional testing may include:
Metabolic screening:
Cardiovascular risk assessment:
Genetic testing may be recommended when:
While usually unnecessary, skin biopsy may be performed when:
Biopsy reveals characteristic foam cells (lipid-laden macrophages) in the dermis, confirming the diagnosis. The procedure involves:
Most cases diagnosed at specialized facilities like those offering mole and cyst removal services don't require biopsy, as clinical appearance suffices for diagnosis.
Perhaps the most critical aspect of xanthelasma evaluation involves cardiovascular risk assessment. Research indicates that xanthelasma serves as an independent risk marker for:
This association persists even in individuals with normal cholesterol levels, suggesting xanthelasma may indicate:
Comprehensive cardiovascular evaluation helps determine appropriate preventive strategies beyond xanthelasma treatment itself.[9]
Multiple effective treatments exist for eyelid early stage xanthelasma, ranging from medical management to surgical removal. Treatment selection depends on lesion characteristics, patient preferences, underlying health conditions, and cosmetic goals.
The foundation of xanthelasma management involves addressing underlying lipid abnormalities. While this approach may not eliminate existing lesions, it prevents progression and reduces recurrence risk.
Statin therapy: HMG-CoA reductase inhibitors (atorvastatin, rosuvastatin, simvastatin) effectively lower LDL cholesterol. Studies show:
Other lipid-lowering medications:
Dietary modifications:
While medical management alone rarely eliminates visible lesions, it remains essential for overall health and preventing new deposits.[10]
Surgical removal represents the gold standard for eyelid early stage xanthelasma, offering the lowest recurrence rates (5-15%) among all treatment modalities.
Procedure details:
Advantages:
Disadvantages:
Surgical excision performed at specialized centers like The Minor Surgery Center typically yields excellent results with minimal scarring.[11]
Various laser modalities effectively treat xanthelasma with good cosmetic outcomes and moderate recurrence rates (20-40%).
CO2 laser ablation:
Erbium:YAG laser:
Pulsed dye laser:
Q-switched lasers:
Laser treatments offer advantages for patients seeking minimal invasiveness, though recurrence rates exceed surgical excision.[12]
Trichloroacetic acid (TCA) application represents a chemical approach to xanthelasma removal:
Procedure:
Outcomes:
Other chemical agents occasionally used include:
Chemical treatments offer lower cost but higher recurrence rates compared to surgical or laser approaches.
Liquid nitrogen cryotherapy freezes and destroys xanthelasma tissue:
Technique:
Considerations:
Cryotherapy suits patients seeking non-invasive options but should understand limitations.
Research continues into novel xanthelasma treatments:
Topical statins: Experimental formulations applied directly to lesions show promise in small studies but remain investigational.
Photodynamic therapy: Light-activated chemicals that selectively destroy lipid-laden cells; early research stage.
Radiofrequency ablation: Heat-based tissue destruction; limited data available.
Intralesional injections: Various substances injected directly into lesions with variable results.
These approaches require further research before becoming standard treatment options.[13]
Choosing the optimal treatment for eyelid early stage xanthelasma involves weighing multiple factors:
FactorSurgical ExcisionLaser TherapyChemical/CryoRecurrence rateLowest (5-15%)Moderate (20-40%)Higher (30-60%)Cosmetic outcomeExcellentVery goodGood to variableDowntime7-14 days7-14 days7-14 daysScarring riskMinimal with expertiseMinimalVariableCostModerate-HighHighLow-ModerateSessions neededUsually one1-31-4
Early-stage lesions generally respond better to all treatment modalities, emphasizing the importance of timely intervention.
Preventing eyelid early stage xanthelasma development and managing recurrence after treatment requires a comprehensive approach addressing underlying metabolic factors and lifestyle modifications.
The most effective prevention strategy involves maintaining optimal lipid levels through:
Target lipid goals for xanthelasma prevention:
Achieving these targets significantly reduces xanthelasma development risk and recurrence after treatment. Regular monitoring (annually or more frequently with abnormal levels) ensures sustained control.[14]
Evidence-based dietary strategies for lipid optimization include:
Foods to emphasize:
Foods to limit or avoid:
Specific dietary patterns with proven lipid benefits:
Dietary changes work synergistically with medications, often allowing lower drug doses or preventing medication need entirely.
Regular physical activity improves lipid profiles and reduces xanthelasma risk through multiple mechanisms:
Recommended exercise parameters:
Lipid benefits of exercise:
Even modest activity levels provide benefits, with greater improvements at higher intensities and durations.[15]
Achieving and maintaining healthy weight significantly impacts lipid profiles:
Weight loss benefits:
Sustainable weight management strategies:
Maintaining weight loss proves more challenging than initial loss, requiring ongoing commitment and sometimes professional support.
Optimal control of secondary conditions that promote xanthelasma reduces risk:
Diabetes management:
Thyroid optimization:
Liver health:
Kidney function:
Addressing these conditions often dramatically improves lipid profiles and reduces xanthelasma recurrence risk.
After successful xanthelasma removal, preventing recurrence requires:
Immediate post-treatment period (0-3 months):
Long-term maintenance (3+ months):
Recurrence rates by treatment modality:
Combining optimal treatment selection with aggressive lipid management minimizes recurrence risk. Patients who achieve and maintain normal lipid levels experience significantly lower recurrence rates across all treatment types.[16]
Individuals with familial lipid disorders may benefit from:
Understanding genetic contributions helps optimize prevention strategies and set realistic expectations for treatment outcomes.
Beyond medical management, eyelid early stage xanthelasma affects psychological well-being, social interactions, and daily life. Addressing these dimensions ensures comprehensive care.
The visible nature of xanthelasma creates unique challenges:
Common emotional responses:
Impact factors:
Research indicates that quality of life improvements following successful treatment often exceed expectations based on lesion size alone, highlighting the significant psychological burden these seemingly minor lesions carry.[17]
While pursuing treatment, individuals can minimize xanthelasma visibility through:
Makeup strategies:
Eyewear considerations:
Hair and styling:
These temporary measures provide confidence while awaiting or between treatments.
Xanthelasma may influence various life domains:
Workplace impact:
Social interactions:
Insurance and financial considerations:
Understanding these realities helps individuals plan appropriately and advocate for their needs.
Not all xanthelasma requires immediate treatment. Observation may be appropriate when:
Treatment becomes advisable when:
The decision remains highly personal, with no "wrong" choice. Discussing options with providers at facilities like The Minor Surgery Center helps clarify individual priorities.
Managing eyelid early stage xanthelasma benefits from comprehensive support:
Healthcare team:
Personal support:
Educational resources:
A strong support network improves treatment adherence, emotional well-being, and long-term outcomes.
Spontaneous resolution of xanthelasma occurs rarely, if ever. Once formed, these cholesterol deposits typically persist indefinitely without intervention. However, aggressive lipid management may stabilize very small, early lesions and prevent progression. Complete disappearance without treatment should not be expected, making professional evaluation and treatment consideration important for those desiring removal.
Xanthelasma itself is benign and harmless, causing no direct health problems. However, it serves as an important marker for:
The true danger lies not in the lesions themselves but in what they may indicate about overall cardiovascular health. Comprehensive evaluation and risk factor management prove essential for all affected individuals.
Recurrence rates vary significantly by treatment method:
Factors influencing recurrence:
Optimal lipid management dramatically reduces recurrence risk across all treatment modalities. Patients maintaining normal cholesterol levels experience significantly lower recurrence rates than those with persistent dyslipidemia.
No scientifically validated home remedies exist for xanthelasma removal. Various internet sources suggest:
None of these have proven efficacy, and some may cause skin irritation, burns, or other complications. Additionally, attempting home removal of any skin lesion risks infection, scarring, and delayed proper diagnosis.
Professional treatment provides safe, effective removal with predictable outcomes. Home dietary and lifestyle modifications support lipid management but won't eliminate existing lesions.
Growth rates vary considerably among individuals:
Typical progression:
Factors affecting growth rate:
Early intervention during the initial growth phase typically yields the best cosmetic outcomes with minimal scarring potential.
While uncommon, pediatric xanthelasma does occur, almost always in children with:
Childhood-onset xanthelasma warrants:
Children with xanthelasma face elevated lifelong cardiovascular risk, making early identification and intervention crucial.
Most insurance plans classify xanthelasma removal as cosmetic and therefore not covered. Exceptions may include:
Medical management of underlying lipid disorders is typically covered as cardiovascular disease prevention. Patients should:
Cost should not prevent evaluation and lipid management, even if removal remains self-pay.
Eyelid early stage xanthelasma represents more than a cosmetic concern—it serves as a visible indicator of lipid metabolism and potential cardiovascular risk. Understanding this condition empowers individuals to make informed decisions about their health and appearance.
🔑 Early recognition matters: Identifying yellowish eyelid deposits promptly enables timely intervention and better treatment outcomes.
🔑 Comprehensive evaluation is essential: All individuals with xanthelasma should undergo complete lipid testing and cardiovascular risk assessment, regardless of age or apparent health.
🔑 Multiple effective treatments exist: From surgical excision to laser therapy, various options provide safe, effective removal with varying recurrence rates.
🔑 Lipid management prevents recurrence: Achieving and maintaining optimal cholesterol levels dramatically reduces the likelihood of new lesions or recurrence after treatment.
🔑 Lifestyle modifications make a difference: Diet, exercise, weight management, and overall health optimization support both treatment success and cardiovascular wellness.
For individuals with eyelid early stage xanthelasma, the following steps provide a roadmap forward:
Immediate actions (within 1-2 weeks):
Short-term actions (1-3 months):
Long-term commitments:
Selecting an experienced provider ensures optimal outcomes. Consider:
Facilities like The Minor Surgery Center specialize in minor surgical procedures including xanthelasma removal, offering expertise and comprehensive care.
Perhaps the most important takeaway: xanthelasma signals the need for cardiovascular risk assessment and management. While the visible lesions may motivate initial consultation, the true value lies in identifying and addressing underlying metabolic issues that affect overall health and longevity.
Successful xanthelasma management requires partnership between patient and healthcare team, combining medical expertise with patient commitment to lifestyle optimization. This comprehensive approach not only addresses the cosmetic concern but potentially prevents serious cardiovascular events in the future.
Living with eyelid early stage xanthelasma need not diminish quality of life. With proper evaluation, appropriate treatment, and committed lipid management, individuals can achieve:
The journey begins with recognition and education—both accomplished by reading this comprehensive guide. The next step involves action: scheduling that medical evaluation, committing to lifestyle changes, and taking control of both appearance and health.
Remember that xanthelasma, while visible and sometimes concerning, represents an opportunity—a chance to identify and address cardiovascular risk factors before they cause serious problems. By viewing these yellowish deposits as health messengers rather than mere cosmetic nuisances, individuals transform a challenging diagnosis into a catalyst for positive change.
Whether choosing immediate treatment or careful observation, the key lies in comprehensive evaluation and ongoing management of underlying factors. With modern treatment options and evidence-based lipid management strategies, excellent outcomes are achievable for the vast majority of individuals affected by this common condition.
[1] Bergman R. The pathogenesis and clinical significance of xanthelasma palpebrarum. Journal of the American Academy of Dermatology. 1994;30(2):236-242.
[2] Christoffersen M, Frikke-Schmidt R, Schnohr P, et al. Xanthelasmata, arcus corneae, and ischaemic vascular disease and death in general population: prospective cohort study. BMJ. 2011;343:d5497.
[3] Nair PA, Singhal R. Xanthelasma Palpebrarum. StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
[4] Watanabe A, Yoshimura A, Wakasugi T, et al. Serum lipids, lipoprotein lipids and coronary heart disease in patients with xanthelasma palpebrarum. Atherosclerosis. 1981;38(3-4):283-290.
[5] Segal P, Insull W Jr, Chambless LE, et al. The association of dyslipoproteinemia with corneal arcus and xanthelasma. The Lipid Research Clinics Program Prevalence Study. Circulation. 1986;73(1 Pt 2):I108-118.
[6] Pedace FJ, Winkelmann RK. Xanthelasma palpebrarum. JAMA. 1965;193:893-894.
[7] Rohrich RJ, Janis JE, Pownell PH. Xanthelasma palpebrarum: a review and current management principles. Plastic and Reconstructive Surgery. 2002;110(5):1310-1314.
[8] Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. 2019;139(25):e1082-e1143.
[9] Christoffersen M, Tybjærg-Hansen A. Visible aging signs as risk markers for ischemic heart disease: epidemiology, pathogenesis and clinical implications. Ageing Research Reviews. 2016;25:24-41.
[10] Zak A, Zeman M, Slaby A, Vecka M. Xanthomas: clinical and pathophysiological relations. Biomedical Papers. 2014;158(2):181-188.
[11] Mendelson BC, Masson JK. Xanthelasma: follow-up on results after surgical excision. Plastic and Reconstructive Surgery. 1976;58(5):535-538.
[12] Raulin C, Schoenermark MP, Werner S, Greve B. Xanthelasma palpebrarum: treatment with the ultrapulsed CO2 laser. Lasers in Surgery and Medicine. 1999;24(2):122-127.
[13] Haygood LJ, Bennett JD, Brodell RT. Treatment of xanthelasma palpebrarum with bichloracetic acid. Dermatologic Surgery. 1998;24(12):1027-1031.
[14] Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. European Heart Journal. 2020;41(1):111-188.
[15] Mann S, Beedie C, Jimenez A. Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: review, synthesis and recommendations. Sports Medicine. 2014;44(2):211-221.
[16] Navarrete-Solís J, Castells-Rodellas A, Moreno-Vílchez M, et al. Xanthelasma palpebrarum: treatment with Er:YAG laser. Lasers in Medical Science. 2013;28(1):1-6.
[17] Hintschich C. Xanthelasma and xanthoma. Der Ophthalmologe. 2011;108(8):734-740.