Dupuytren's contracture is a benign yet often misunderstood condition that affects the connective tissue beneath the skin of your palm and fingers. While it's not life-threatening, its impact on daily life can be significant—from struggling to wear gloves and shake hands to difficulty performing work tasks and personal care activities. Understanding this condition is the first step toward managing it effectively and maintaining your quality of life.
Dupuytren's contracture, also known as Dupuytren's disease or palmar fibromatosis, is a progressive hand condition that affects the fascia—the layer of connective tissue located just beneath the skin of your palm. This condition was first described by French surgeon Baron Guillaume Dupuytren in the 1830s, and it remains one of the most common inherited disorders affecting the hands.
In healthy hands, the palmar fascia is a thin, flexible layer of tissue that helps you grip objects and provides structural support. When Dupuytren's contracture develops, this tissue gradually thickens and tightens, forming rope-like cords and hard nodules. Over time, these cords contract and pull one or more fingers toward the palm, creating a permanent bend that cannot be straightened voluntarily.
The progression of Dupuytren's contracture typically follows a predictable pattern, though the speed and severity vary significantly from person to person:
Stage 1 - Nodule Formation: Small, firm lumps (nodules) appear in the palm, usually at the base of the ring or little finger. These may be tender initially but often become painless over time.
Stage 2 - Cord Development: The nodules gradually extend into thick, cord-like bands of tissue that run from the palm toward the fingers.
Stage 3 - Finger Contracture: The cords tighten and begin pulling the affected fingers toward the palm, limiting extension and creating functional impairment.
Stage 4 - Advanced Contracture: Severe bending occurs, with fingers pulled tightly against the palm, significantly impacting hand function and daily activities.
The condition most commonly affects the ring finger and little finger, though any finger can be involved. In some cases, both hands develop contractures, and the condition can even affect the feet (Ledderhose disease) or penis (Peyronie's disease), though these are separate manifestations.
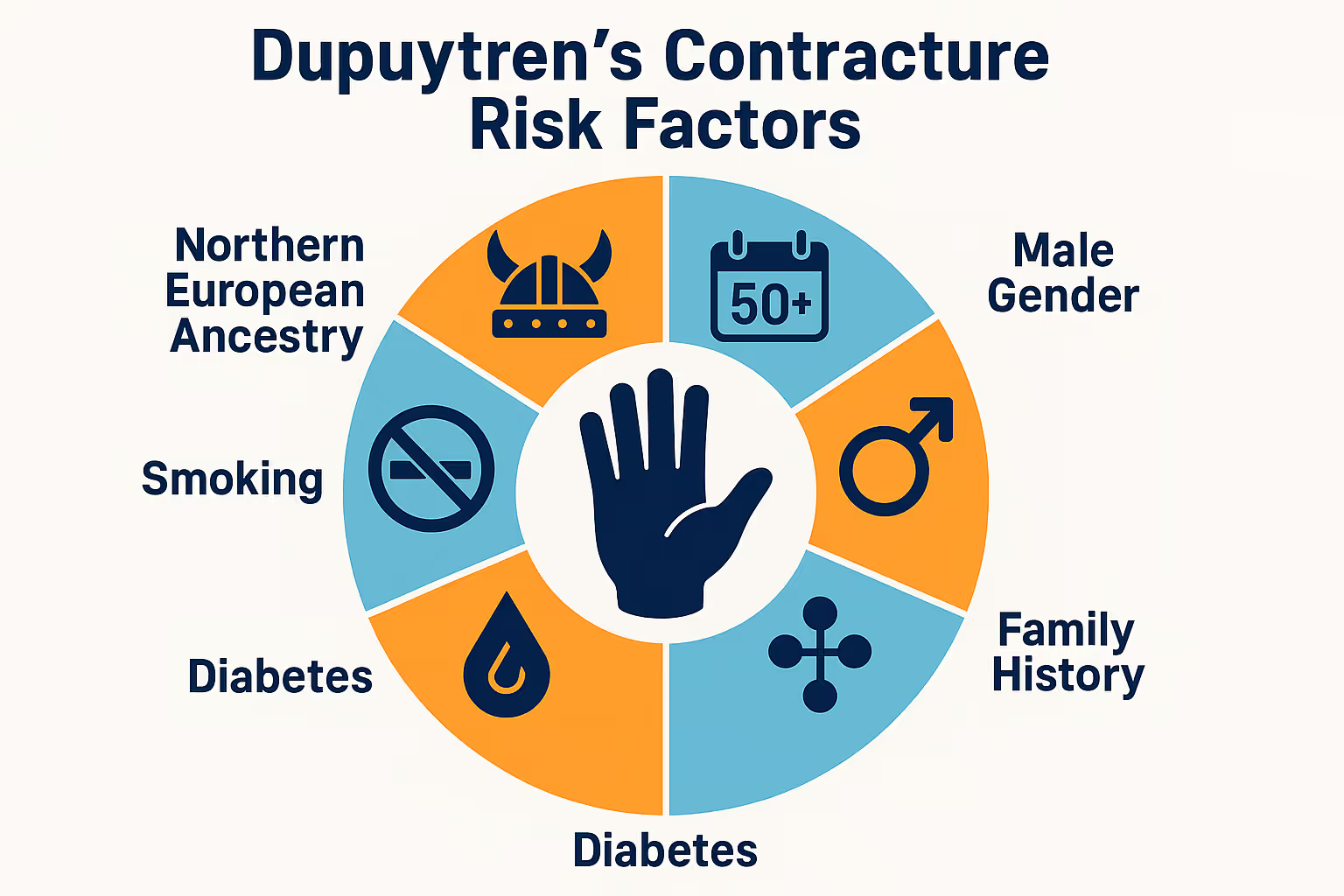
Understanding your risk factors can help you recognize early signs and seek appropriate evaluation. Dupuytren's contracture doesn't affect everyone equally—certain populations and individuals face significantly higher risk.
Ancestry and Ethnicity 🌍
Dupuytren's contracture is sometimes called the "Viking disease" because it's most prevalent in people of Northern European descent, particularly those with Scandinavian, Scottish, Irish, or English ancestry. The condition is far less common in Asian, African, and Southern European populations.
Age
The likelihood of developing Dupuytren's contracture increases significantly with age. While it can occasionally appear in younger adults, most people develop symptoms after age 50, with prevalence continuing to rise through the 70s and 80s.
Gender
Men are approximately 3-9 times more likely to develop Dupuytren's contracture than women. When women do develop the condition, it typically appears later in life and progresses more slowly.
Family History
Genetics play a crucial role—if you have a close relative with Dupuytren's contracture, your risk increases substantially. Studies suggest that up to 70% of people with the condition have a family history, indicating strong hereditary components.
FactorImpact on RiskDiabetes2-3x increased risk; may lead to earlier onsetSmokingSignificantly increases risk and disease severityAlcohol consumptionHeavy drinking associated with higher prevalenceManual laborRepetitive hand trauma may contribute (controversial)Epilepsy medicationsSome anti-seizure drugs linked to increased riskHIV/AIDSAssociated with more aggressive disease progression
It's important to note that having risk factors doesn't guarantee you'll develop Dupuytren's contracture, and some people develop the condition without any identifiable risk factors. However, awareness of your risk profile helps you stay vigilant for early signs.

Early detection of Dupuytren's contracture allows for better monitoring and timely intervention when necessary. The condition typically develops gradually, sometimes over years or even decades, making it easy to dismiss initial symptoms as normal aging or minor hand issues.
Small Lumps or Nodules 👆
The first sign is usually a small, firm lump in the palm, typically near the base of the ring or little finger. These nodules may feel like calluses or small peas beneath the skin. Initially, they might be tender or sensitive to pressure, though this discomfort often subsides over time.
Skin Pitting and Thickening
You might notice small indentations or dimples in the palm skin, accompanied by thickening of the skin itself. The skin may also become difficult to pinch or lift away from the underlying tissue.
Tender Areas
While Dupuytren's contracture isn't typically painful once established, early nodules can cause discomfort, especially when gripping objects or applying pressure to the palm.
As the condition advances, additional symptoms emerge:
Visible Cords
Thick, rope-like bands of tissue become visible and palpable beneath the skin, running from the palm toward one or more fingers.
Finger Bending
Affected fingers begin to curl toward the palm. This typically starts subtly—you might notice difficulty laying your hand flat on a table (the "tabletop test"). As contracture progresses, the bend becomes more pronounced.
Functional Limitations
Daily activities become challenging:
Bilateral Involvement
Many people eventually develop Dupuytren's contracture in both hands, though one side is often more severely affected than the other.
It's equally important to understand what symptoms are not typical of Dupuytren's contracture:
❌ Severe pain – While early nodules may be tender, significant pain is uncommon and suggests other conditions
❌ Sudden onset – This is a gradual condition, not an acute injury
❌ Joint swelling or redness – These symptoms indicate inflammation or arthritis, not Dupuytren's
❌ Numbness or tingling – Nerve symptoms suggest conditions like carpal tunnel syndrome
❌ Weakness – Muscle weakness points to neurological issues rather than fascial contracture
If you notice any lumps, thickening, or finger contracture in your palm, it's worth seeking professional evaluation at a specialized facility like The Minor Surgery Center, where experienced practitioners can provide accurate diagnosis and guidance.
Diagnosing Dupuytren's contracture is typically straightforward and doesn't require extensive testing. The condition has distinctive physical characteristics that trained healthcare providers can identify through clinical examination.
Medical History Review
Your healthcare provider will ask about:
Physical Examination
The cornerstone of diagnosis is a thorough hand examination:
Visual Inspection: Your provider will look for nodules, cords, skin changes, and finger positioning.
Palpation: Feeling the palm and fingers helps identify the location, size, and firmness of nodules and cords.
The Tabletop Test: You'll be asked to place your hand flat on a table. Inability to lay the hand completely flat suggests contracture is present.
Range of Motion Assessment: Your provider will measure how much each finger can extend and bend, documenting the degree of contracture.
Functional Assessment: Discussion of how the condition impacts specific activities helps guide treatment decisions.
In most cases, imaging is not necessary for diagnosing Dupuytren's contracture. The clinical examination provides sufficient information. However, in certain situations, additional tests may be ordered:
Ultrasound: Can help visualize the fascia and assess disease extent, particularly when planning treatment.
MRI: Rarely used, but may be helpful if diagnosis is uncertain or if other conditions need to be ruled out.
Blood tests: Not used to diagnose Dupuytren's itself, but may be ordered to check for diabetes or other conditions that influence treatment planning.
Your healthcare provider will also consider other conditions that can cause similar symptoms:
The expertise of qualified professionals, like those on our team, ensures accurate diagnosis and appropriate treatment recommendations tailored to your specific situation.
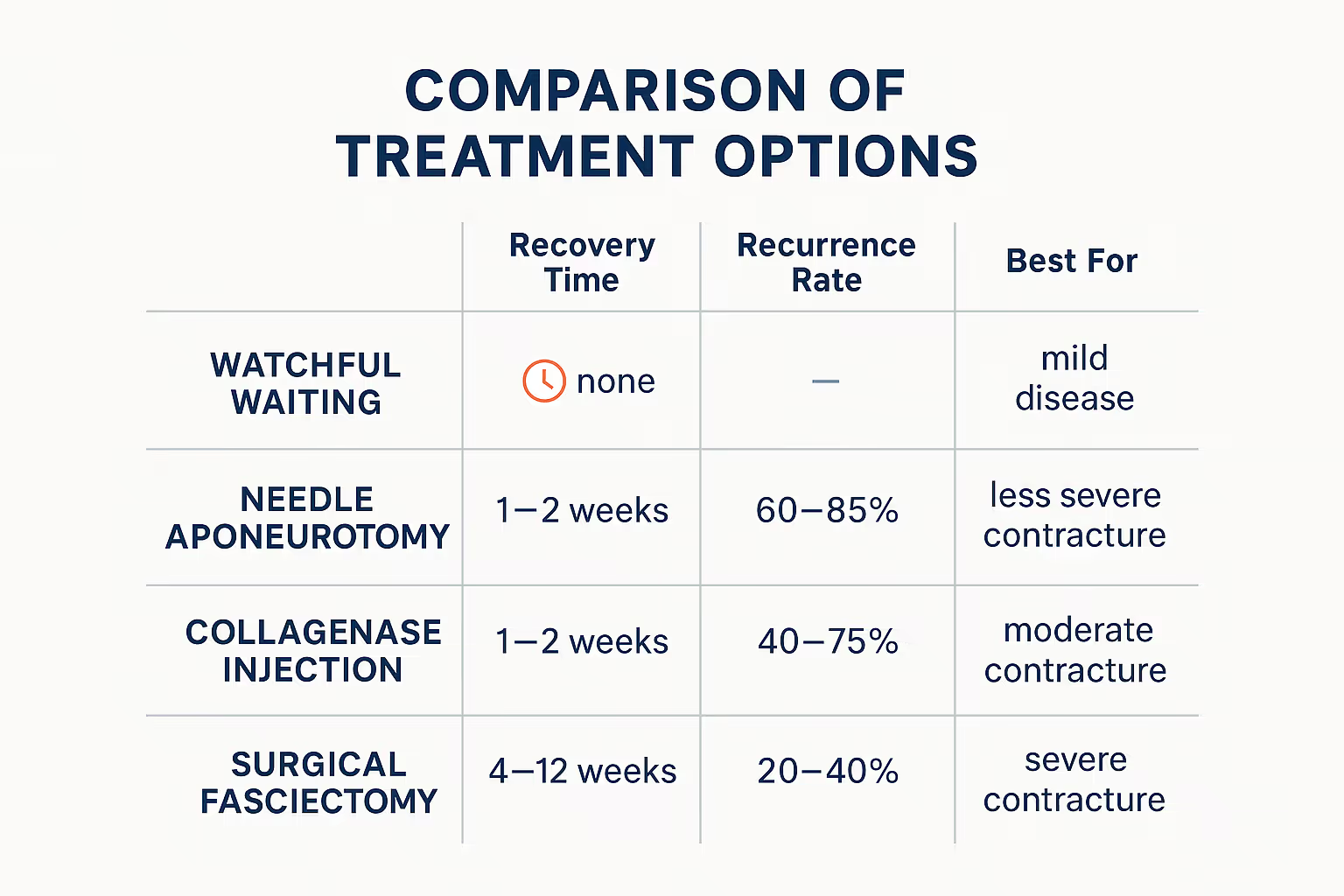
Treatment for Dupuytren's contracture isn't one-size-fits-all. The appropriate approach depends on several factors: the severity of your contracture, how quickly it's progressing, how much it affects your daily life, and your overall health status. Let's explore the full spectrum of treatment options available in 2025.
For many people, especially those with early-stage disease, no immediate treatment is the best approach. If you have small nodules without significant finger contracture or functional impairment, your healthcare provider may recommend regular monitoring.
When observation is appropriate:
What to expect: Regular check-ups (typically every 6-12 months) to monitor progression, along with education about signs that would warrant intervention. Many people live comfortably with mild Dupuytren's contracture for years without needing active treatment.
Physical Therapy and Stretching
While stretching exercises cannot reverse Dupuytren's contracture or prevent progression, they may help maintain finger mobility and function. A hand therapist can teach you appropriate exercises and provide splinting recommendations.
Radiation Therapy
Low-dose radiation therapy has shown promise in slowing disease progression when used in very early stages. This approach is more common in Europe than North America and is typically reserved for rapidly progressing disease in younger patients.
Steroid Injections
Corticosteroid injections into tender nodules may provide temporary relief from discomfort, though they don't address the underlying contracture or prevent progression.
Needle Aponeurotomy (Percutaneous Needle Fasciotomy)
This office-based procedure uses a small needle to puncture and break the contracted cord, allowing the finger to straighten. It's performed under local anesthesia and offers quick recovery.
Advantages:
Limitations:
Collagenase Injection (Xiaflex)
This FDA-approved treatment involves injecting an enzyme that dissolves the collagen in the contracted cord. The finger is then manipulated to break the cord, typically the day after injection.
Advantages:
Limitations:
When contracture is severe (typically more than 30-40 degrees), progressing rapidly, or significantly impacting function, surgery often provides the most effective and durable solution.
Fasciectomy
This procedure involves surgically removing the diseased fascia. It can be performed as:
Limited (Selective) Fasciectomy: Removal of only the affected cords and nodules—the most common approach.
Regional Fasciectomy: Removal of all potentially affected fascia in a region, used for more extensive disease.
Dermofasciectomy: Removal of both diseased fascia and overlying skin (for severe or recurrent cases), followed by skin grafting.
What to expect from surgery:
Before the procedure:
During the procedure:
After the procedure:
Treatment TypeRecurrence RateRecovery TimeTypical Cost RangeNeedle Aponeurotomy50-85% at 5 years1-2 weeks$$Collagenase Injection35-65% at 5 years2-4 weeks$$$Limited Fasciectomy20-50% at 5 years4-12 weeks$$$$Dermofasciectomy10-20% at 5 years8-16 weeks$$$$$
Understanding the costs associated with various treatments is important. You can explore estimated costs for different procedures using our cost estimator tool to help plan your care.
The decision about which treatment to pursue should be made collaboratively with your healthcare provider, considering:
While Dupuytren's contracture is a progressive condition, many people manage it successfully and maintain good hand function throughout their lives. Whether you're monitoring early-stage disease or recovering from treatment, practical strategies can help you adapt and thrive.
Hand Function Strategies 🖐️
When contracture limits finger extension, small modifications can maintain independence:
Workplace Accommodations
If Dupuytren's contracture affects your work, consider:
While you can't prevent Dupuytren's contracture or stop its progression through lifestyle changes alone, certain practices support overall hand health:
Avoid Excessive Trauma: While the link between hand trauma and Dupuytren's is debated, protecting your hands from repetitive injury is sensible.
Manage Related Conditions: Keep diabetes well-controlled and address other health issues that may influence disease progression.
Quit Smoking: Smoking is associated with more aggressive Dupuytren's disease, and cessation benefits overall health.
Moderate Alcohol Consumption: Heavy drinking correlates with higher disease prevalence.
Stay Active: Gentle hand exercises and activities maintain mobility and strength.
If you've undergone treatment for Dupuytren's contracture, proper follow-up care maximizes results:
Follow Hand Therapy Recommendations
Physical or occupational therapy is crucial after most treatments, especially surgery. Your therapist will guide you through:
Attend Follow-Up Appointments
Regular check-ins with your healthcare provider help identify recurrence early and address any complications promptly.
Monitor for Recurrence
Dupuytren's contracture can return after treatment. Stay alert for:
Be Patient with Recovery
Full recovery from surgical treatment takes time—often several months. Swelling, stiffness, and sensitivity are normal during the healing process.
Living with a visible hand condition can affect self-esteem and social interactions. It's normal to feel:
Coping strategies:
If you suspect you might have Dupuytren's contracture or have been monitoring early-stage disease, knowing when to seek professional evaluation is important.
Initial Symptoms
Schedule an evaluation if you notice:
Disease Progression
If you're already diagnosed, seek follow-up when:
Post-Treatment Concerns
After any intervention, contact your provider if you experience:
Dupuytren's contracture can be evaluated and treated by various specialists:
Hand Surgeons: Orthopedic or plastic surgeons specializing in hand conditions—ideal for surgical cases.
Orthopedic Surgeons: Specialists in musculoskeletal conditions, many with hand expertise.
Plastic Surgeons: Often have extensive hand surgery training and experience.
Primary Care Physicians: Can provide initial evaluation and referrals to specialists.
For comprehensive evaluation and treatment of hand conditions, facilities like The Minor Surgery Center offer specialized expertise in a patient-focused environment, making the process straightforward and accessible.
Come Prepared 📋
Maximize your appointment by:
Questions to Ask Your Provider
Don't hesitate to ask for clarification if something isn't clear. Understanding your condition and options empowers you to make informed decisions about your care.
The field of Dupuytren's contracture treatment continues to evolve, with ongoing research exploring new approaches and refining existing ones. Understanding what's on the horizon offers hope for even better outcomes in the future.
Genetic Studies
Researchers have identified multiple genetic variations associated with Dupuytren's contracture, improving understanding of who's at risk and potentially paving the way for targeted preventive strategies.
Molecular Mechanisms
Scientists are investigating exactly how normal fascia transforms into the thickened, contracted tissue of Dupuytren's disease. This research may reveal new treatment targets.
Improved Collagenase Treatments
Work continues on optimizing enzyme injection protocols, improving outcomes, and reducing side effects.
Novel Minimally Invasive Approaches
Development of new techniques that balance effectiveness with minimal invasiveness and quick recovery.
Recurrence Prevention
Understanding why contractures return after treatment is a major research focus, with studies examining factors that influence recurrence and strategies to prevent it.
Radiation Therapy Protocols
While not new, radiation therapy for early Dupuytren's is being studied more extensively in North America, with trials examining optimal timing, dosing, and patient selection.
Pharmacological Approaches
Research into medications that might slow or prevent disease progression is ongoing, though no proven pharmaceutical prevention exists yet.
Biological Treatments
Investigation of growth factors, stem cells, and other biological agents that might influence disease behavior.
Enhanced Surgical Techniques
Refinement of surgical approaches to improve outcomes, reduce complications, and lower recurrence rates.
While these developments are promising, it's important to maintain realistic expectations:
For the latest information on treatment options and conditions we address, healthcare providers stay current with evolving research and guidelines.
Dupuytren's contracture typically is not painful once established. Early nodules may be tender or sensitive to pressure, but this usually resolves over time. The primary issue is loss of finger extension and functional limitation rather than pain. If you're experiencing significant pain, it may indicate another condition, and you should seek evaluation.
Unfortunately, there's no proven way to prevent Dupuytren's contracture if you're genetically predisposed. However, you can potentially reduce risk or slow progression by:
These measures support overall hand health but don't guarantee prevention.
Many people with Dupuytren's contracture eventually develop it in both hands, though one side is often more severely affected. If you have the condition in one hand, there's approximately a 40-60% chance the other hand will eventually be affected. Bilateral involvement doesn't necessarily mean both hands will require treatment.
Recovery time varies based on the extent of surgery and individual healing:
Following your surgeon's post-operative instructions and hand therapy recommendations significantly influences recovery success.
Yes, recurrence is possible with all treatment types, though rates vary:
Recurrence doesn't mean treatment failed—it reflects the progressive nature of the disease. If contracture returns, additional treatment can be performed.
No, these are distinct conditions. Dupuytren's contracture affects the palmar fascia, causing finger contracture without nerve symptoms. Carpal tunnel syndrome involves compression of the median nerve, causing numbness, tingling, and sometimes pain—but not finger contracture. However, it's possible to have both conditions simultaneously.
Hand therapy cannot reverse contracture or prevent progression, but it plays an important role in:
Hand therapy is especially crucial after surgical treatment to optimize outcomes.
For additional questions about hand conditions and treatment options, visit our FAQ section for more information.
Dupuytren's contracture doesn't have to control your life. Whether you're noticing early signs or living with advanced contracture, understanding this condition empowers you to make informed decisions about your care.
If you're experiencing early symptoms:
If you have established contracture:
If you've had treatment:
Dupuytren's contracture treatment requires expertise and experience. At The Minor Surgery Center, we provide:
✅ Expert evaluation by experienced professionals who understand hand conditions
✅ Personalized treatment plans tailored to your specific situation and goals
✅ Clear communication about your options, without confusing medical jargon
✅ Patient-focused environment designed to reduce anxiety and streamline care
✅ Accessible locations making quality care convenient—find our clinics near you
We believe you deserve to feel confident in your care and comfortable with your treatment decisions. Our team of skilled surgeons brings both technical expertise and compassionate understanding to every patient interaction.
Thousands of people successfully manage Dupuytren's contracture every day. With proper evaluation, appropriate treatment when needed, and ongoing monitoring, most people maintain good hand function and quality of life.
Don't let uncertainty or anxiety prevent you from seeking the care you need. Whether you're looking for an initial evaluation, a second opinion, or ready to discuss treatment options, professional guidance makes all the difference.
Dupuytren's contracture is a progressive hand condition that affects the fascia beneath your palm's skin, causing nodules, cords, and eventually finger contracture that can significantly impact daily life. While this condition is more common in people of Northern European descent, men over 50, and those with family history, it can affect anyone.
Early recognition of symptoms—small lumps in the palm, skin thickening, or difficulty laying your hand flat—allows for appropriate monitoring and timely intervention when needed. Treatment options range from watchful waiting for mild cases to minimally invasive procedures like needle aponeurotomy and collagenase injection, to surgical fasciectomy for more severe contractures.
The key to successfully managing Dupuytren's contracture lies in:
🔍 Early awareness of symptoms and risk factors
🩺 Professional evaluation by experienced healthcare providers
💡 Informed decision-making about treatment options
🎯 Personalized care tailored to your specific needs and goals
🔄 Ongoing monitoring to address progression or recurrence
Remember, Dupuytren's contracture is a manageable condition. With proper care, most people maintain good hand function and continue enjoying their daily activities. Whether you're experiencing early symptoms or living with established contracture, expert guidance and appropriate treatment can help you feel confident in your hands again.
If you're ready to take the next step, The Minor Surgery Center is here to provide the expert, compassionate care you deserve. Don't let hand contracture limit your life—reach out today to learn more about your options and start your journey toward better hand health.
For more information about the conditions we treat and how we can help, explore our blog for additional resources and patient education materials.