Discovering a new lump or bump on your skin can be a source of immediate concern. In a world where health information is at our fingertips, distinguishing between a benign growth and a potentially serious condition like skin cancer is paramount. One common skin growth that often leads to anxiety is the dermatofibroma. It’s a firm, often reddish-brown lesion that can sometimes mimic the appearance of certain skin cancers. This article aims to provide a comprehensive, authoritative guide on Dermatofibroma vs. Skin Cancer, helping you understand the key differences, diagnostic methods, and when to seek professional medical advice. Understanding these distinctions is not just about alleviating worry; it's about empowering you with the knowledge to protect your skin health in 2025 and beyond.
Dermatofibromas, also known as benign fibrous histiocytomas, are common, harmless skin lesions. They are typically small, firm bumps that can range in color from pink to red, brown, or even purple, depending on your skin tone and how long the lesion has been present. While they can appear anywhere on the body, they are most frequently found on the arms and legs.
A dermatofibroma is essentially a scar-like reaction within the skin, consisting of a proliferation of fibrous tissue (collagen) and histiocytes (a type of immune cell). They often feel firm or hard, almost like a small pebble under the skin. A defining characteristic, known as the "dimple sign" or "buttonhole sign," occurs when you gently pinch the skin around the lesion: the dermatofibroma tends to dimple inwards. This happens because the growth is tethered to the underlying tissue.
The exact cause of dermatofibromas is not always clear, but they are often thought to develop after minor skin trauma, such as an insect bite, a splinter, or even a shave cut. It’s as if the skin overreacts to the injury, forming a small, localized scar. Some individuals may be more prone to developing them, and they can sometimes be multiple. They are more common in women than in men and tend to appear in adulthood. There's no strong genetic link, nor are they contagious.
While dermatofibromas are benign, it's crucial to have any new or changing skin lesion evaluated by a dermatologist. The primary reason for this is to differentiate it from skin cancer. Even if you suspect it's a dermatofibroma, a professional diagnosis is vital to ensure peace of mind and accurate identification. If a dermatofibroma becomes painful, bleeds, grows rapidly, or changes significantly in appearance, a doctor should assess it promptly.
Skin cancer is the uncontrolled growth of abnormal skin cells. It is the most common form of cancer, and early detection is key to successful treatment. There are several types of skin cancer, each with distinct characteristics and varying degrees of aggressiveness.
Skin cancer arises when there is damage to the DNA of skin cells, most often due to exposure to ultraviolet (UV) radiation from the sun or tanning beds. This damage triggers mutations that cause skin cells to grow rapidly and form malignant tumors. Unlike dermatofibromas, which are benign, skin cancers have the potential to invade surrounding tissues and, in some cases, spread to other parts of the body (metastasize).
The three most common types of skin cancer are:
Several factors increase your risk of developing skin cancer:
The "ABCDE" rule is a simple guide to help you identify suspicious moles that might be melanoma:
Distinguishing between a dermatofibroma and skin cancer is crucial for timely diagnosis and appropriate treatment. While some visual similarities might exist, especially to the untrained eye, there are significant differences in their clinical features, behavior, and potential for harm.
FeatureDermatofibromaBasal Cell Carcinoma (BCC)Squamous Cell Carcinoma (SCC)MelanomaSizeTypically small (0.5 - 1.5 cm)Varies, often small initiallyVaries, can be larger than BCCVaries, often >6mm when concerning, but can be smallerShapeDome-shaped nodule, firm, well-defined bordersPearly or waxy bump, flat, scar-like, open soreFirm, red nodule; scaly patch; open soreOften irregular or asymmetricalColorPink, red, brown, purple; often darker in centerFlesh-colored, pearly, pink, brown. May have visible blood vessels (telangiectasias)Red, flesh-colored, scaly, crustedMultiple colors: shades of brown, black, red, white, blueTexture/FeelFirm, hard, rubbery; "dimple sign" when pinchedSmooth, waxy, sometimes crusty or bleedingRough, scaly, firm; may bleed easily, especially if pickedSmooth or bumpy; can be itchy, tender, or bleedingGrowth PatternStable or very slow growth over years, often appears after traumaSlow-growing, locally invasive; rarely metastasizesCan grow rapidly; higher risk of metastasis than BCCRapid growth and change; highest risk of metastasis if not treated earlySymptomsUsually asymptomatic; sometimes itchy or tenderUsually asymptomatic; may bleed easilyMay be tender, painful, bleed easilyCan be itchy, tender, painful, bleeding, crusting, or oozing (Evolving - ABCDEs)LocationMost common on legs and armsSun-exposed areas: face, neck, ears, scalp, chest, backSun-exposed areas: face, lips, ears, neck, hands, arms, legs; also mucous membranesCan appear anywhere, including non-sun-exposed areas (soles, palms, nail beds)Dimple SignPresent (classic diagnostic feature)AbsentAbsentAbsentPotential for HarmBenign (no cancerous potential)Malignant, locally destructive; very low metastatic potentialMalignant, can metastasize; moderate metastatic potentialHighly malignant, high metastatic potential; life-threatening if untreated
The "dimple sign" is a crucial clinical differentiator for dermatofibromas. When you gently squeeze a dermatofibroma from the sides, it will often pucker inward, creating a dimple. This happens because the fibrous tissue of the dermatofibroma is tethered to the underlying subcutaneous tissue. Skin cancers, on the other hand, do not exhibit this dimpling phenomenon. This simple test, while not 100% definitive on its own, is a strong indicator of a dermatofibroma.
Despite their clear differences, certain skin cancers can sometimes be mistaken for a dermatofibroma, especially in their early stages or if they present atypically.
Because of these potential overlaps, self-diagnosis is not recommended. Professional dermatological evaluation is always the safest course of action.
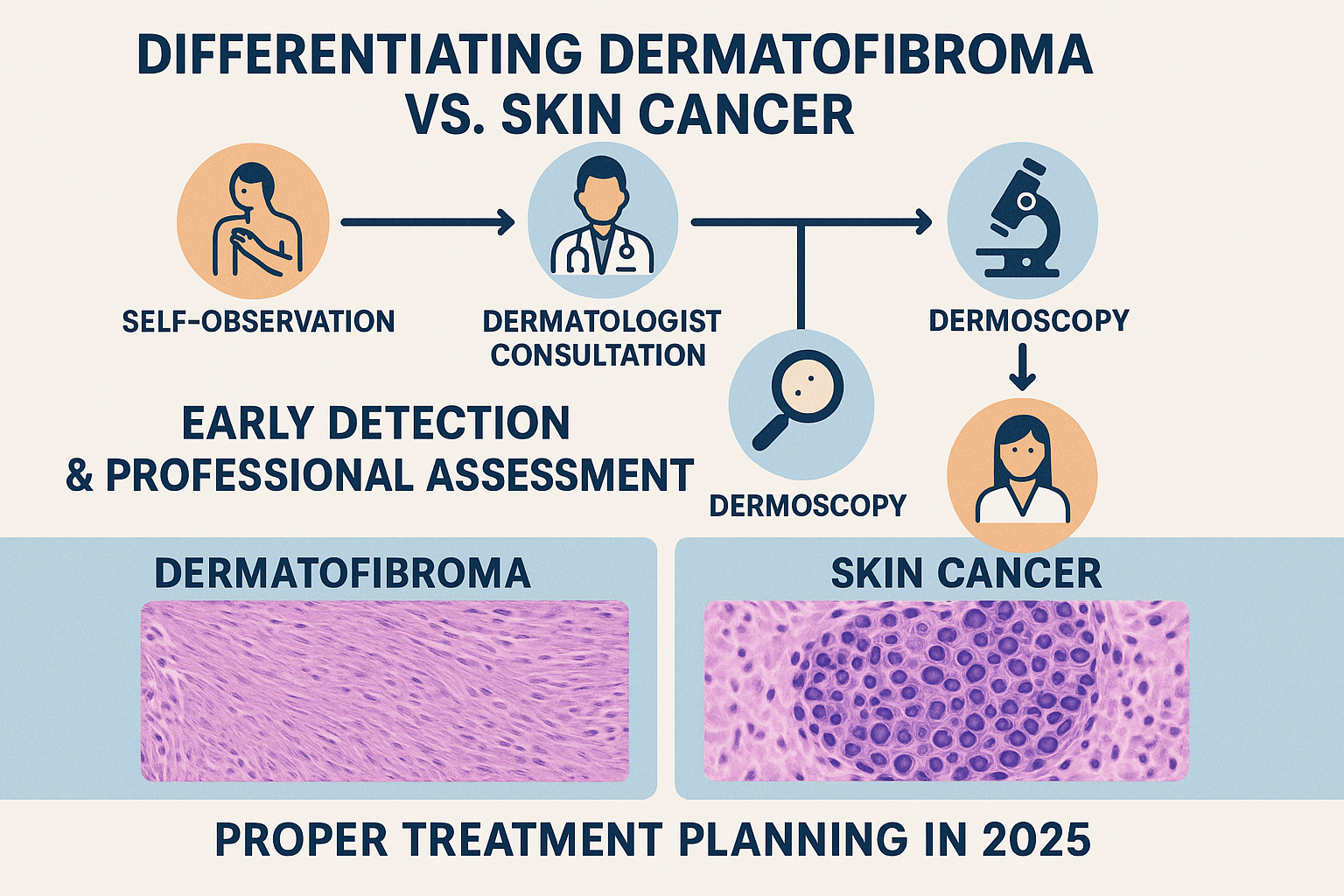
When you notice a new or changing spot on your skin, the most responsible action is to schedule an appointment with a board-certified dermatologist. They are specialists trained to identify and differentiate various skin conditions, including Dermatofibroma vs. Skin Cancer. The diagnostic process typically involves a combination of visual examination, specialized tools, and sometimes, tissue analysis.
During your visit, the dermatologist will begin by taking a detailed medical history. They will ask about:
Following the history, a thorough visual examination will be conducted. This involves looking at the suspicious lesion, as well as checking other areas of your skin for any other concerning spots. The dermatologist will pay close attention to the lesion's:
A powerful tool in the dermatologist's arsenal is the dermatoscope. This is a handheld device that combines a powerful magnifying lens (typically 10x magnification) with a polarized light source. Dermoscopy allows the dermatologist to visualize structures and patterns within the skin lesion that are not visible to the naked eye.
For dermatofibromas, dermoscopy often reveals a characteristic central white scar-like area surrounded by a delicate pigmented network. Skin cancers, particularly melanoma, show highly specific dermoscopic patterns that help distinguish them from benign lesions. For instance, melanoma might display atypical pigment networks, dots, globules, streaks, or regression structures. BCCs often show arborizing (tree-like) telangiectasias (blood vessels), while SCCs can show keratin plugs or white circles.
Dermoscopy significantly improves the accuracy of diagnosis and helps dermatologists decide whether a lesion requires a biopsy.
If a lesion remains suspicious after visual examination and dermoscopy, the dermatologist will recommend a biopsy. A biopsy is the definitive diagnostic tool, as it involves removing a small piece of tissue from the lesion for microscopic examination by a pathologist.
There are several types of biopsies:
The tissue sample is then processed and examined under a microscope by a dermatopathologist, who specializes in diagnosing skin conditions from tissue samples. This examination allows for a conclusive diagnosis, determining whether the lesion is a dermatofibroma, a specific type of skin cancer, or another skin condition.
Early diagnosis of skin cancer, especially melanoma, is critical. Melanoma detected and treated at an early stage has a very high cure rate. If left untreated, it can quickly spread to lymph nodes and other organs, becoming much more difficult to treat and significantly reducing survival rates. For BCC and SCC, early diagnosis prevents extensive local damage and reduces the (albeit lower) risk of metastasis. For dermatofibromas, an accurate diagnosis eliminates unnecessary worry and avoids potentially aggressive treatments for a benign condition. Regular skin checks, both self-checks and professional examinations, are your best defense. For example, staying informed about your health and financial future is always a good idea, much like understanding your 2025 Canadian Housing Market Outlook can help you plan ahead.
The approach to treatment differs significantly between dermatofibromas and skin cancers, reflecting their benign versus malignant nature. Understanding these differences is essential for patients once a diagnosis has been confirmed.
Since dermatofibromas are benign, treatment is generally not medically necessary. Many people choose to leave them alone. However, there are situations where removal might be considered:
Treatment options for dermatofibromas include:
It's important to discuss the pros and cons of each removal method with your dermatologist, including potential scarring and recurrence rates.
Treatment for skin cancer is always necessary and aims to completely remove or destroy the cancerous cells to prevent growth, invasion, and metastasis. The specific treatment approach depends on the type of skin cancer, its size, location, and the patient's overall health.
For BCC and SCC, a variety of effective treatments are available:
Melanoma treatment is typically more aggressive due to its higher metastatic potential.
The choice of treatment for skin cancer is highly individualized and determined by a multidisciplinary team of specialists, including dermatologists, surgeons, oncologists, and radiation oncologists. Regular follow-up appointments are crucial after skin cancer treatment to monitor for recurrence or new lesions. Just like understanding mortgage options, knowing your treatment path is vital. For example, learning about alternative down payment options in Canada can open new avenues for homeownership, much like new therapies open doors for cancer treatment.
The best defense against skin cancer is prevention and early detection. Being proactive about your skin health in 2025 involves adopting sun-safe habits and regularly examining your skin for any suspicious changes.
Minimizing your exposure to harmful UV radiation is the most effective way to reduce your risk of skin cancer.
Regular self-skin exams are vital for early detection. The goal is to become familiar with your skin's normal appearance, so you can quickly spot any new or changing lesions.
How to Perform a Self-Skin Exam (Monthly):
In addition to self-exams, annual professional skin checks by a dermatologist are highly recommended, especially for individuals with increased risk factors for skin cancer (e.g., fair skin, numerous moles, family history of melanoma, significant sun exposure history). Dermatologists are trained to spot subtle changes and can use tools like dermoscopy to examine lesions in detail that you might miss. Think of it like getting a professional assessment for your financial health; a best mortgage rates calculator can give you a baseline, but an expert like a mortgage agent (such as Anahita Shamei or Manzeel Patel) offers personalized advice.
For individuals with a history of skin cancer, more frequent professional skin checks (every 3-6 months) may be necessary. These regular evaluations are crucial for monitoring existing moles and identifying any new or recurrent lesions at the earliest possible stage.
Beyond sun protection and regular checks, maintaining overall skin health can contribute to prevention. A balanced diet rich in antioxidants, staying hydrated, and avoiding smoking can all play a role in supporting your skin's resilience. While these won't prevent all skin cancers, they contribute to a healthier body and skin. Furthermore, understanding the broader health landscape, like the 2025 Canadian Mortgage Rule updates, can reflect a proactive approach to managing all aspects of your life.
If you've been diagnosed with a dermatofibroma, it's natural to have questions about its long-term implications. The good news is that dermatofibromas are benign, meaning they are not cancerous and pose no threat to your health.
A dermatofibroma will not turn into skin cancer. Once diagnosed, it typically remains stable, though it might slowly grow or shrink over many years. They are not contagious and do not spread to other parts of the body. In rare cases, they might spontaneously regress, but usually, they persist indefinitely. The prognosis is excellent, and there are no associated health risks once a definitive diagnosis is made.
Most dermatofibromas are asymptomatic. However, if yours is itchy, tender, or causes mild pain, there are a few things you can do:
For many, the biggest concern with a dermatofibroma is the initial anxiety surrounding the "what if it's cancer?" question. Receiving a definitive diagnosis of a benign lesion can bring immense relief. It's important to remember that it's a very common skin finding, and countless individuals live with dermatofibromas without any issues.
If you have multiple dermatofibromas, or if their appearance causes significant cosmetic distress, discuss your concerns openly with your dermatologist. They can provide reassurance, discuss management strategies, and explore removal options if appropriate. Sometimes, simply understanding that it is harmless is enough to alleviate concern.
The information presented in this article about Dermatofibroma vs. Skin Cancer is for educational purposes only and should not replace professional medical advice. If you have any concerns about a skin lesion, a prompt consultation with a dermatologist is always the best course of action.
Any of the following signs should prompt an immediate visit to a dermatologist:
Dermatologists undergo extensive training to diagnose and treat a wide range of skin conditions. Their expertise allows them to:
Remember, early detection is critical for successful skin cancer treatment. Don't procrastinate or try to self-diagnose based on internet searches alone. Trusting your skin's health to a professional ensures the best possible outcome.
Navigating the landscape of skin lesions can be unsettling, but armed with knowledge about Dermatofibroma vs. Skin Cancer, you are better prepared to recognize potential warning signs and seek timely professional help. While a dermatofibroma is a harmless, benign growth characterized by its firm texture and unique "dimple sign," skin cancers – including basal cell carcinoma, squamous cell carcinoma, and the more dangerous melanoma – are malignant and require prompt diagnosis and treatment.
The key takeaway is that vigilance and professional evaluation are your strongest allies in maintaining skin health. Regularly check your skin for any new or changing spots, paying close attention to the ABCDEs of melanoma. If you identify any suspicious lesions or have concerns, do not hesitate to consult a board-certified dermatologist. Their expertise, coupled with diagnostic tools like dermoscopy and biopsy, can accurately differentiate between benign and malignant conditions, ensuring you receive the correct diagnosis and appropriate care in 2025. Prioritizing your skin health is an investment in your overall well-being.