Have you ever noticed a small, firm bump on your skin and wondered whether it's a harmless growth or a scar from an old injury? The confusion between dermatofibroma vs scar tissue is remarkably common, even among healthcare professionals at first glance. These two skin conditions can appear deceptively similar, yet they represent fundamentally different biological processes with distinct characteristics, causes, and treatment approaches.
Understanding the difference between dermatofibroma and scar tissue isn't just an academic exercise—it has real implications for diagnosis, treatment decisions, and peace of mind. While both conditions are generally benign, knowing which one you're dealing with can help you make informed choices about whether to seek medical evaluation, pursue treatment, or simply monitor the lesion over time.
A dermatofibroma (also called fibrous histiocytoma or sclerosing hemangioma) is a common benign skin lesion that develops within the dermal layer of the skin. These growths represent a proliferation of fibroblasts, histiocytes, and other cellular components that create a firm, nodular structure beneath the skin's surface [1].
Dermatofibromas present with several distinctive features that help identify them:
One of the most characteristic clinical signs is the "dimple sign" or "buttonhole sign"—when you pinch the lesion between your fingers, it dimples inward rather than protruding outward [2]. This occurs because the dermatofibroma is tethered to the overlying epidermis while being surrounded by normal, more flexible skin.
The exact cause of dermatofibromas remains somewhat mysterious. Unlike scar tissue, these lesions don't always have a clear traumatic trigger. However, several theories exist:
Dermatofibromas are more common in women than men and typically develop in young to middle-aged adults [3]. They're completely benign with no malignant potential, though very rarely, atypical variants may require closer monitoring.
Scar tissue represents the body's natural wound healing response to injury. When skin or other tissues are damaged—whether through surgery, trauma, burns, or inflammation—the body initiates a complex repair process that ultimately results in scar formation.
Not all scars are created equal. When discussing dermatofibroma vs scar tissue, it's important to understand the different types of pathological scarring:
Hypertrophic scars are raised, thickened scars that remain confined to the boundaries of the original injury. They develop due to excessive collagen production during the healing process but don't extend beyond the wound margins [4].
Key characteristics include:
Keloids represent a more aggressive form of scarring that extends beyond the original wound boundaries. These scars result from an overproduction of collagen—approximately 20 times greater than normal tissue—creating thick, hyalinized collagen bundles arranged in a haphazard pattern [5].
Distinguishing features include:
Most wounds heal with normal scar formation—flat, pale scars that fade over time and don't cause functional or cosmetic concerns. These represent successful wound healing without excessive collagen deposition.
Understanding scar tissue formation requires knowledge of the wound healing cascade:
Abnormal scarring occurs when this process becomes dysregulated, particularly during the proliferative and remodeling phases, leading to excessive collagen production and disorganized tissue architecture.
When comparing dermatofibroma vs scar tissue, several critical distinctions emerge across clinical presentation, etiology, histology, and behavior. Understanding these differences is essential for accurate diagnosis and appropriate management.
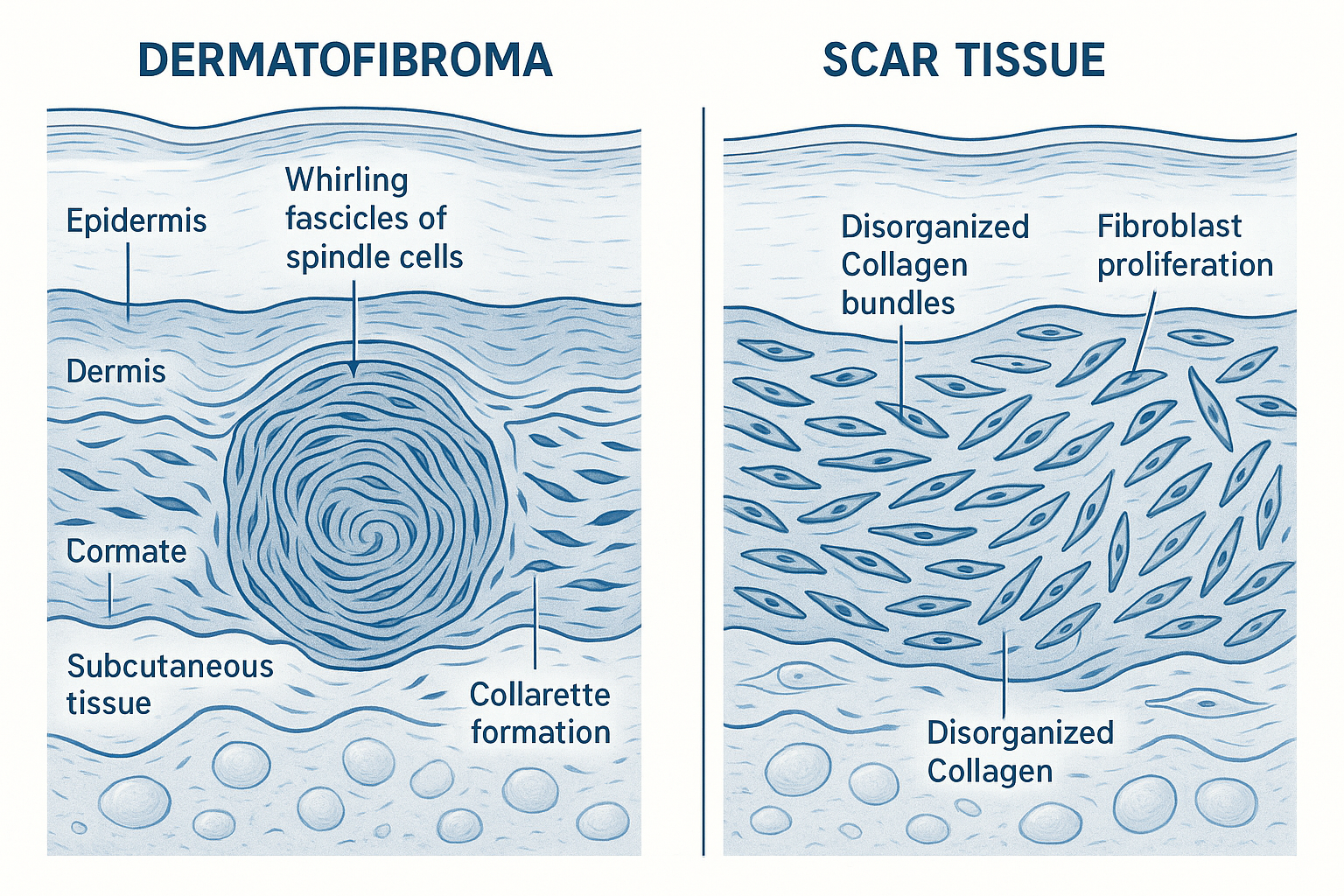
The microscopic examination reveals fundamental differences in tissue architecture:
Dermatofibromas display:
Scar tissue (keloids and hypertrophic scars) shows:
Dermoscopy—examination with a specialized magnifying device—reveals distinct patterns that aid in differentiating dermatofibroma vs scar tissue:
Dermatofibroma dermoscopic patterns:
Scar tissue dermoscopic patterns:
These dermoscopic differences can help clinicians make accurate diagnoses without requiring biopsy in many cases.
The natural history of these conditions differs significantly:
Dermatofibromas:
Scar tissue:
Accurate diagnosis is crucial when evaluating dermatofibroma vs scar tissue. Healthcare professionals employ several complementary approaches to distinguish between these conditions and rule out other possibilities.
The diagnostic process begins with a thorough clinical evaluation:
History taking should include:
Physical examination assesses:
Dermoscopic examination provides magnified visualization of skin structures invisible to the naked eye. This non-invasive technique can often differentiate dermatofibroma from scar tissue based on the characteristic patterns described earlier [8].
For those seeking professional guidance on important life decisions, understanding the difference between various conditions—whether in healthcare or finance—requires expert evaluation and careful consideration.
When clinical and dermoscopic findings are inconclusive, or when there's concern about atypical features, a biopsy may be necessary:
Indications for biopsy:
Biopsy techniques:
Histopathological analysis examines:
The histological examination provides definitive diagnosis and can identify rare variants or unexpected findings that might require different management approaches.
Immunohistochemical staining uses antibodies to identify specific proteins within tissue samples. This technique is particularly valuable in distinguishing dermatofibroma vs scar tissue:
FXIIIa (Factor XIIIa):
Other markers that may be used:
Both dermatofibromas and pathological scars must be distinguished from other skin conditions:
Conditions that may mimic dermatofibroma:
Conditions that may mimic scar tissue:
A systematic diagnostic approach combining clinical assessment, dermoscopy, and when necessary, histopathology ensures accurate identification and appropriate management.
The management strategies for dermatofibroma vs scar tissue differ significantly, reflecting their distinct nature and behavior. Treatment decisions should be individualized based on symptoms, cosmetic concerns, and patient preferences.
Most dermatofibromas require no treatment as they are benign and typically asymptomatic. However, intervention may be considered in certain situations:
For asymptomatic dermatofibromas with typical features, observation is often the recommended approach:
Advantages:
Monitoring guidelines:
Complete surgical removal is the definitive treatment for dermatofibromas:
Indications:
Considerations:
Important caveat: Patients should understand that excision of a dermatofibroma often leaves a scar that may be more cosmetically noticeable than the original lesion [10]. This consideration is particularly important for lesions in visible areas.
Cryotherapy (freezing with liquid nitrogen) can flatten dermatofibromas:
Characteristics:
Shave excision removes the raised portion of the dermatofibroma:
Features:
Managing pathological scars (keloids and hypertrophic scars) is more complex and often requires multimodal approaches. Prevention is ideal, but various treatments exist for established scars.
For individuals prone to abnormal scarring, prevention is the best approach:
Corticosteroid injections (typically triamcinolone) are the first-line treatment for keloids and hypertrophic scars:
Mechanism: Reduces inflammation, decreases collagen synthesis, and promotes collagen breakdown
Protocol:
Side effects:
Silicone gel sheets or topical silicone gel are effective for scar management:
Mechanism: Hydration, occlusion, and possibly growth factor modulation
Application:
Evidence: Studies show 60-100% improvement in scar appearance with consistent use [11]
Surgical removal of keloids or hypertrophic scars carries high recurrence risk (50-100% for keloids) when used alone. Therefore, excision is typically combined with adjuvant treatments:
Adjuvant options:
Various laser modalities can improve scar appearance:
Pulsed dye laser (PDL):
Fractional laser:
CO2 laser:
Several newer approaches show promise:
Many practitioners combine multiple modalities for optimal results, such as corticosteroid injections with silicone therapy, or laser treatment followed by topical medications.
For those navigating complex decisions about treatment options, consulting with experienced professionals can help ensure you make informed choices tailored to your specific situation.
While both dermatofibromas and scar tissue are typically benign, certain situations warrant professional medical evaluation to ensure accurate diagnosis and appropriate management.
Seek medical attention if you notice any of the following concerning features:
For any skin lesion (suspected dermatofibroma or scar):
⚠️ Rapid growth: Significant enlargement over weeks to months
⚠️ Color changes: Development of multiple colors, darkening, or variegated pigmentation
⚠️ Ulceration or bleeding: Surface breakdown or spontaneous bleeding without trauma
⚠️ Pain or tenderness: New onset or increasing discomfort (beyond typical keloid symptoms)
⚠️ Size: Lesions larger than 1.5 cm or continuing to grow
⚠️ Asymmetry or irregular borders: Particularly if changing over time
⚠️ Satellite lesions: Development of multiple small lesions around the primary lesion
For suspected scar tissue:
Even experienced clinicians may find it challenging to distinguish dermatofibroma vs scar tissue based on appearance alone. Professional evaluation is warranted when:
Certain individuals should maintain lower thresholds for seeking evaluation:
Personal or family history of:
Occupational or recreational exposures:
For individuals managing multiple important health and financial decisions simultaneously, understanding when to seek expert guidance can prevent complications and ensure optimal outcomes.
Both dermatofibromas and pathological scars are generally benign conditions that many people live with without significant impact on their health. However, understanding how to manage these conditions can improve quality of life and prevent complications.
For dermatofibromas:
✅ Regular self-examination: Check monthly for changes in size, color, or symptoms
✅ Avoid trauma: Minimize irritation from shaving, tight clothing, or scratching
✅ Sun protection: While not specifically required for dermatofibromas, general sun protection supports overall skin health
✅ Photography: Take periodic photos to objectively track any changes over time
✅ Symptom management: If itchy, avoid scratching; consider topical moisturizers or mild hydrocortisone cream
For scar tissue:
✅ Massage: Gentle scar massage can improve pliability and appearance
✅ Moisturization: Keep scars well-hydrated with fragrance-free moisturizers
✅ Sun protection: Critical for preventing hyperpigmentation; use SPF 30+ sunscreen
✅ Silicone therapy: Continue silicone gel or sheets as recommended
✅ Avoid trauma: Protect scars from injury, which can trigger worsening
✅ Compression: For large scars or keloids, compression garments may help
Both conditions can impact self-esteem and body image, particularly when located in visible areas:
Coping strategies:
Realistic expectations:
While dermatofibromas cannot be reliably prevented, scar tissue formation can be minimized:
Optimal wound care:
For keloid-prone individuals:
Early intervention:
Understanding the prognosis for each condition helps set appropriate expectations:
Dermatofibromas:
Scar tissue:
Both conditions are compatible with normal, healthy lives. The decision to pursue treatment should be based on symptoms, functional impairment, cosmetic concerns, and personal preferences rather than medical necessity in most cases.
No, dermatofibromas are benign lesions with no malignant potential. They do not transform into cancer. However, if a lesion previously diagnosed as a dermatofibroma begins showing concerning changes (rapid growth, ulceration, color changes), re-evaluation is warranted to ensure the original diagnosis was correct and to rule out other conditions.
Dermatofibromas rarely disappear completely on their own, though they may slowly regress over many years. Most remain stable in size or may become slightly less prominent over time. If removal is desired for cosmetic or symptomatic reasons, active treatment is necessary.
The key distinguishing features include:
However, professional evaluation is the most reliable way to distinguish between these conditions.
No, while both represent pathological scarring, they differ:
Both result from excessive collagen production but represent different degrees of dysregulated wound healing.
Absolutely not. Attempting to remove any skin lesion at home carries serious risks:
Always seek professional medical care for lesion removal.
Unfortunately, there is no reliable prevention for dermatofibromas. Since their exact cause remains unclear and they often develop without identifiable triggers, preventive measures are not available. General skin health practices are beneficial but won't specifically prevent dermatofibroma formation.
Keloids have a high recurrence rate (50-100% after excision alone) because:
This is why multimodal treatment (combining excision with radiation, corticosteroids, or other adjuvant therapies) is recommended to reduce recurrence risk.
Most dermatofibromas are asymptomatic (painless). However, some people experience:
Significant pain is unusual and should prompt medical evaluation to confirm the diagnosis.
While this guide provides comprehensive information about dermatofibroma vs scar tissue, it cannot replace professional medical evaluation. Self-diagnosis of skin lesions carries inherent risks and limitations.
Accurate diagnosis is essential because:
A dermatology consultation typically includes:
Initial assessment:
Diagnostic procedures (if needed):
Treatment planning:
For skin lesion evaluation, consider consulting:
Just as finding the right professional is crucial in healthcare, the same principle applies to other important life decisions. Whether you're seeking expert financial guidance or medical care, working with qualified professionals ensures the best outcomes.
Understanding the differences between dermatofibroma vs scar tissue empowers individuals to make informed decisions about their skin health. While these conditions may appear similar at first glance, they represent fundamentally different biological processes with distinct characteristics, causes, and management approaches.
Key points to remember:
✨ Dermatofibromas are benign fibrous growths that typically appear spontaneously, most commonly on the lower legs, with characteristic features including the dimple sign and organized histological patterns
✨ Scar tissue (keloids and hypertrophic scars) results from wound healing responses, always corresponds to injury sites, and displays disorganized collagen architecture
✨ Clinical examination, dermoscopy, and histopathological analysis (when needed) provide accurate differentiation between these conditions
✨ Treatment approaches differ significantly: dermatofibromas often require no intervention, while scar tissue may benefit from various therapeutic modalities
✨ Professional evaluation is essential for accurate diagnosis, especially when lesions show atypical features or cause concern
If you have a skin lesion and are wondering whether it's a dermatofibroma or scar tissue:
Both dermatofibromas and pathological scars are common, benign conditions that affect millions of people. While they may cause cosmetic concerns or occasional symptoms, they don't pose serious health risks. The decision to pursue treatment should be individualized based on symptoms, functional impact, cosmetic concerns, and personal preferences.
Modern dermatology offers effective diagnostic tools and treatment options for both conditions. With accurate diagnosis and appropriate management, most individuals can achieve satisfactory outcomes and peace of mind about their skin health.
Remember that skin health is an important component of overall well-being. Regular self-examination, sun protection, optimal wound care, and prompt evaluation of concerning lesions contribute to maintaining healthy skin throughout life.
Whether you're navigating healthcare decisions or other important life choices, seeking professional expertise and making informed decisions based on accurate information leads to the best possible outcomes.
[1] Calonje E, Brenn T, Lazar A, McKee PH. McKee's Pathology of the Skin. 4th ed. Philadelphia: Elsevier Saunders; 2012.
[2] Zaballos P, Puig S, Llambrich A, Malvehy J. Dermoscopy of dermatofibromas: a prospective morphological study of 412 cases. Archives of Dermatology. 2008;144(1):75-83.
[3] Alves JV, Matos DM, Barreiros HF, Bártolo EA. Variants of dermatofibroma—a histopathological study. Anais Brasileiros de Dermatologia. 2014;89(3):472-477.
[4] Gauglitz GG, Korting HC, Pavicic T, Ruzicka T, Jeschke MG. Hypertrophic scarring and keloids: pathomechanisms and current and emerging treatment strategies. Molecular Medicine. 2011;17(1-2):113-125.
[5] Bran GM, Goessler UR, Hormann K, Riedel F, Sadick H. Keloids: current concepts of pathogenesis (review). International Journal of Molecular Medicine. 2009;24(3):283-293.
[6] Luzar B, Calonje E. Cutaneous fibrohistiocytic tumours—an update. Histopathology. 2010;56(1):148-165.
[7] Lee JY, Yang CC, Chao SC, Wong TW. Histopathological differential diagnosis of keloid and hypertrophic scar. American Journal of Dermatopathology. 2004;26(5):379-384.
[8] Ferrari A, Soyer HP, Peris K, et al. Central white scarlike patch: a dermatoscopic clue for the diagnosis of dermatofibroma. Journal of the American Academy of Dermatology. 2000;43(6):1123-1125.
[9] Zelger BW, Zelger BG, Burgdorf WH. Dermatofibroma—a critical evaluation. International Journal of Surgical Pathology. 2004;12(4):333-344.
[10] Han TY, Chang HS, Lee JH, Lee WM, Son SJ. A clinical and histopathological study of 122 cases of dermatofibroma (benign fibrous histiocytoma). Annals of Dermatology. 2011;23(2):185-192.
[11] Mustoe TA, Cooter RD, Gold MH, et al. International clinical recommendations on scar management. Plastic and Reconstructive Surgery. 2002;110(2):560-571.